Review Article - Interventional Cardiology (2015) Volume 7, Issue 4
Physiological assessment of coronary stenosis: a view from the coronary microcirculation
- Corresponding Author:
- Jan J Piek
AMC Heartcenter, Academic Medical Center – University of Amsterdam
Meibergdreef 9, Room B2–250, PO Box 22660, 1100 DD Amsterdam, The Netherlands
E-mail: j.j.piek@amc.uva.nl
Abstract
The complexity of ischemic heart disease (IHD) comprehends disease in the succeeding perfusion domains of the vascular tree. Fractional flow reserve and coronary flow reserve are validated diagnostic modalities to identify myocardial ischemia, but solitarily do not suffice to objectify the respective contribution of obstructive and nonobstructive disease to IHD. Combined pressure and flow measurements deliver a comprehensive intracoronary assessment of IHD, although fractional flow reserve and coronary flow reserve disagree in 40% of the cases. Discrepancy between the indices does not reflect methodological failure, but explores divergent extremes of epicardial and microvascular disease, which holds vital prognostic value. We advocate critical revision of the current diagnostic and therapeutic approaches toward IHD. In this review, we deliver a perspective on the future developments in the diagnosis and treatment of IHD.The complexity of ischemic heart disease (IHD) comprehends disease in the succeeding perfusion domains of the vascular tree. Fractional flow reserve and coronary flow reserve are validated diagnostic modalities to identify myocardial ischemia, but solitarily do not suffice to objectify the respective contribution of obstructive and nonobstructive disease to IHD. Combined pressure and flow measurements deliver a comprehensive intracoronary assessment of IHD, although fractional flow reserve and coronary flow reserve disagree in 40% of the cases. Discrepancy between the indices does not reflect methodological failure, but explores divergent extremes of epicardial and microvascular disease, which holds vital prognostic value. We advocate critical revision of the current diagnostic and therapeutic approaches toward IHD. In this review, we deliver a perspective on the future developments in the diagnosis and treatment of IHD.
Keywords
coronary artery disease, coronary flow reserve, coronary microvascular dysfunction, coronary microvascular resistance, fractional flow reserve, ischemic heart disease
For almost 40 years, epicardial stenoses have been considered the dominant substrate for ischemic heart disease (IHD). Until today, coronary angiography remains the cornerstone of IHD diagnosis, and its treatment remains governed by the mechanical alleviation of epicardial stenoses deemed to impair myocardial perfusion. In this regard, the physiological appraisal of epicardial disease severity by means of the coronary pressure-derived fractional flow reserve (FFR) has advanced the identification of the functional significance of epicardial stenosis in stable IHD [1–4], but has concomitantly furthered a stenosis-centered approach to IHD. Notwithstanding the superiority of FFR-guided percutaneous coronary intervention (PCI) over angiographic guidance in terms of both clinical outcomes and cost– effectiveness [5–7], up to 60% of stenoses deemed functionally significant by FFR do not require mechanical revascularization up to 2 years after deferral of revascularization. Moreover, around 10% of stenoses deemed not functionally significant by FFR may actually be at high risk for a major adverse event during early follow-up, and a substantial number of patients remain to demonstrate persistent angina after mechanical revascularization [8,9]. These data suggest insufficiency of a stenosis-focused approach in IHD diagnosis and treatment. Accumulating evidence highlights the contribution of microvascular dysfunction in the pathogenesis of IHD, and its obscuring effect on stenosis assessment by coronary pressure measurements [10–13]. These novel insights may urge a critical revision of current diagnostic approaches toward IHD. In this review, we discuss the complexity of IHD from a microvascular viewpoint. We discuss the physiology and pathophysiology of the coronary microvasculature, illustrate its consequences for physiological assessment of epicardial stenosis and the spectrum of IHD, and highlight the potential of multilevel physiological testing as part of future developments in IHD diagnosis.
Physiology of the coronary microcirculation
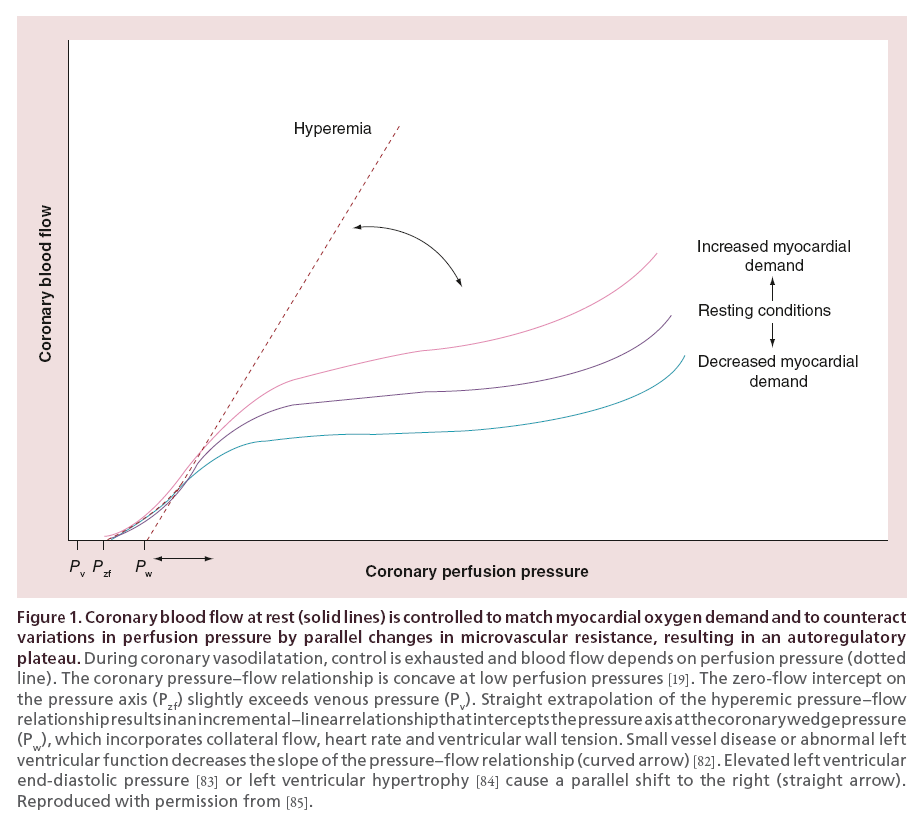
Myocardial function evidently depends on tissue perfusion [14]. Blood flow to the myocardium is therefore strictly regulated at the level of the coronary arterioles, which maintain substantial vasoconstrictor tone and present the dominant site of flow regulation [15]. By adapting resistance of these vessels, blood flow to the myocardium is kept constant for a given myocardial demand, independent from perfusion pressure fluctuations; a mechanism referred to as coronary autoregulation (Figure 1) [16–18]. Similarly, alterations in myocardial demand are compensated by vasodilatation or -constriction of the resistance vessels; a process called metabolic adaption (Figure 1) [18]. Autoregulation and metabolic adaption are interrelated and maintain coronary flow to match myocardial demand. At complete abolishment of vasoconstrictor tone in the resistance vessels, the vasoactive control of blood flow is lost, and perfusion pressure dictates blood flow (Figure 2) [19].
Coronary stenosis: physiology of the epicardial vessels & microvasculature
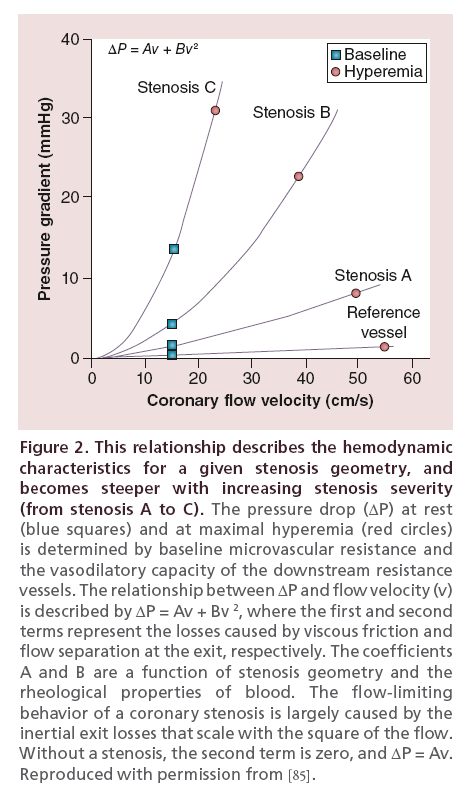
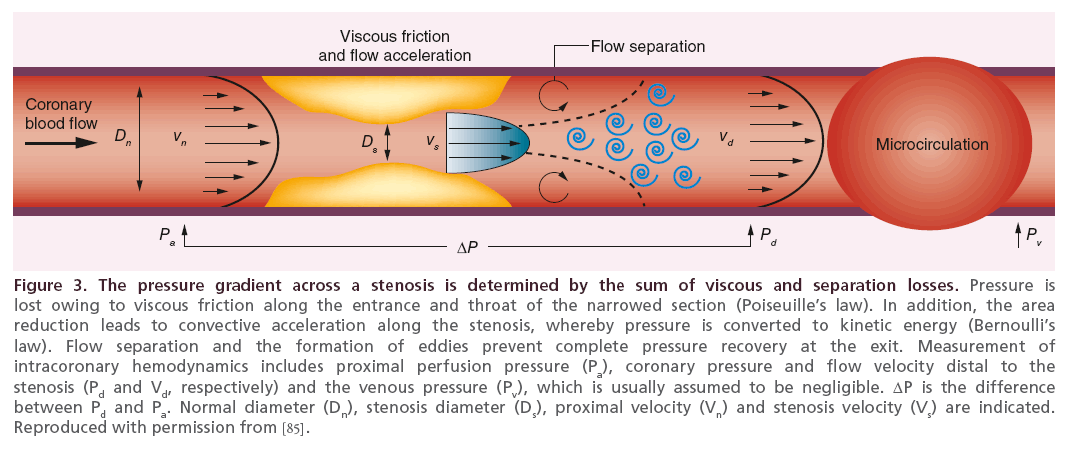
Atherosclerotic narrowing of the epicardial coronary artery impairs myocardial perfusion and induces a pressure drop across the stenosis. This pressure drop results from the loss of kinetic energy due to viscous friction at the entrance and along the course of the lesion, as well as losses due to convective flow acceleration and subsequent flow separation at the stenosis exit leading to flow turbulence and eddy formation. The pressure drop across the stenosis (ΔP) is formed by the sum of viscous friction losses, which increase linearly with the magnitude of flow through the stenosis (v), and separation losses, which increase with the square of flow through the stenosis. The relationship between viscous friction, flow separation losses and stenosis pressure drop is described by the equation ΔP = Av + Bv2, where coefficients A and B are defined by stenosis geometry and rheological properties of blood (viscosity and density), respectively. Stenosis severity is of pivotal influence on the magnitude of the pressure drop, which is illustrated by the fact that it enters both the A and B terms with its inverse fourth power. In the absence of a stenosis, and hence in the absence of quadratic flow separation losses, the equation reduces to a linear term where ΔP equals Av. The relationship between flow through a stenosis and the resulting pressure drop (dP-v relationship) characterizes the hemodynamic behavior of a particular stenosis (Figure 3), where increasing stenosis severity is characterized by a steeper slope, and vice versa.
Figure 3: The pressure gradient across a stenosis is determined by the sum of viscous and separation losses.
With the accumulation of atherosclerotic disease, perfusion of the myocardial tissue is increasingly impaired. As a result, resistance in the coronary micro-vasculature decreases by adaptive vasodilation of the coronary resistance vessels [20,21]. This compensatory vasodilation ensures adequate tissue perfusion up to the point where all reserve vasodilatory capacitiy of the resistance vessels is lost. At this point, any increase in myocardial demand will lead to myocardial ischemia and its clinical sequelae [22].
The relevance of the coronary microvasculature
Accumulating evidence indicates that dysfunction of the coronary microvasculature contributes to the occurrence of myocardial ischemia, and may even comprise its sole cause in the absence of epicardial disease [10–13,23]. Coronary microvascular dysfunction (CMD) is characterized by an insufficient vasodilatory capacity of the coronary resistance vessels to compensate increases in metabolic demand. In clinical terms, CMD can be classified into four different settings: CMD in the absence of obstructive myocardial and epicardial disease, CMD in the presence of myocardial disease, CMD in the presence of obstructive coronary artery disease (CAD) and iatrogenic-induced CMD as the result of PCI-related distal embolization or vasoconstriction [11,23,24]. In the absence of epicardial disease, independent structural and functional microvascular abnormalities, alongside myocardial atherosclerotic disease, are known to disrupt coronary microvascular physiology [23,25,26]. Structural myocardial abnormalities rationally associate with arterial hypertension and hypertrophic cardiomyopathy, and are also documented in various clinical conditions that induce inflammation or enhance pro-oxidative stress. The structural vessel adaptations are characterized by adverse remodeling of the intramural coronary arterioles that emanates from medial wall thickening and intimal thickening induced by smooth muscle cell hypertrophy and elevated collagen deposition, which impedes normal microvascular function. Functional microvascular abnormalities represent a spectrum of endothelial-dependent mechanisms consistent with diabetes mellitus, obesity, smoking and dyslipidemia, as well as nonendothelial-dependent mechanisms, like the manifest of smooth muscle dysfunction due to nitrate resistance. The pathogenic mechanisms underlying structural and functional alterations can coexist for various clinical disorders, though their respective contribution for microvascular dysfunction varies in different clinical settings [11,23,24].
Even though microvascular dysfunction may induce myocardial underperfusion without evident ischemic manifestations on perfusion imaging [11], approximately half of patients with angina pectoris and angiographically normal coronary arteries do display per fusion defects as defined by radionuclide myocardial perfusion scan (MPS) [27,28]. Patients with CMD typically demonstrate poorer prognosis as shown in multiple cohort studies [29–35].
Data from large randomized clinical trials on the subject of PCI also support an important pathophysiological role of the coronary microcirculation in the occurrence of IHD among patients with evident epicardial coronary narrowing. The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial randomly assigned patients with stable CAD (>50% visually assessed occlusion) to undergo PCI plus optimal medical therapy (OMT) or OMT alone. The adjusted and unadjusted 4.6-year cumulative rate of combined death or myocardial infarction was equal between both randomized treatment arms. Although the incidence of angina was reduced by adjuvant PCI treatment as compared with OMT alone, a notable 35% of patients in the PCI arm reported continued angina regardless of mechanical relief of the epicardial stenosis [36]. In addition, 15% of patients in the PCI plus OMT cohort displayed more than 10% inducible ischemia on MPS after mechanical revascularization, suggesting a pertinent role of the coronary microvasculature in the occurrence of ischemia [37]. Evaluation of functional stenosis severity by FFR provides a more accurate selection of hemodynamically significant epicardial lesions that would clinically benefit from mechanical revascularization [1,2]. FFR-guided revascularization trumped angiography-guided revascularization with regard to clinical outcome [5,6]. In the recent Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) II trial, patients whom were referred to the cardiac catheterization laboratory with stable CAD underwent FFR evaluation of all potential revascularization targets. Those patients in whom all stenoses had FFR more than 0.80 were not randomized and were considered the reference group. Those patients in whom at least one stenosis had FFR ≤0.80 were randomized to OMT or OMT plus PCI. Although, similar to COURAGE, adjuvant PCI was associated with a more pronounced reduction in angina complaints, angina class II–IV remained present in 11% of patients in whom all FFR-positive stenoses were relieved, and was present in 15% of patients in whom no hemodynamically significant stenosis was documented, regardless of the initiation of OMT [8,9]. These data support the hypothesis that epicardial stenoses do not occur solitarily, but that myocardial ischemia is a reflection of advanced atherosclerotic disease that affects both the epicardial and microvascular compartment of the coronary circulation. This hypothesis is additionally supported by the fact that atherosclerosis is a nonfocal phenomenon, which suggests that at the stage where clinical sequelae of myocardial ischemia occur; it is a distinct combination of epicardial and microvascular abnormalities that determine their occurrence.
Physiological appraisal of IHD: stenosis assessment
From flow to pressure
The introduction of sensor-equipped guide wires has enabled physiological assessment of CAD severity. The flow-based concept of coronary flow reserve (CFR) has been applied to a wide variety of diagnostic modalities, beyond invasive Doppler flow velocity including transthoracic echocardiography, intracoronary thermodilution, positron emission tomography (PET) and magnetic resonance imaging (MRI). CFR is defined as the ratio of maximal flow during hyperemia to flow in rest in a given coronary artery. In Doppler flow velocity, a guide wire equipped with a Doppler crystal is used to obtain flow velocity waveforms. CFR derived from Doppler (CFRDoppler) is then defined as the ratio of hyperemic to basal average peak flow velocity distal to the stenosis. The invasive thermodilution technique defines CFR (CFRthermo) using coronary thermodilution curves obtained from a guide wire equipped with a temperature-sensitive pressure sensor. Thermodilution curves are obtained in triplicate, and are exploited to measure the mean transit time (Tmn) of a bolus of cold saline injected directly into the coronary artery. CFRthermo is defined as the ratio of hyperemic Tmn to resting Tmn. Recent validation studies confirmed CFRthermo as a feasible alternative, which correlates favorably with CFRDoppler. However, widespread application of CFRthermo is currently restricted by its limited validation [38–43] and concerns with respect to the requisite rapid injection of saline to obtain the thermodilution curve. The latter may limit its use to determine CFR, since saline injections may particularly affect basal transit times since they are known to induce a reactive hyperemic state. Noninvasive modalities like transthoracic echocardiography [44–46] and PET [32] also allow the measurement of global and regional myocardial blood flow and CFR, and may serve as noninvasivebased gatekeepers before invasive physiological interrogation of the coronary circulatory.
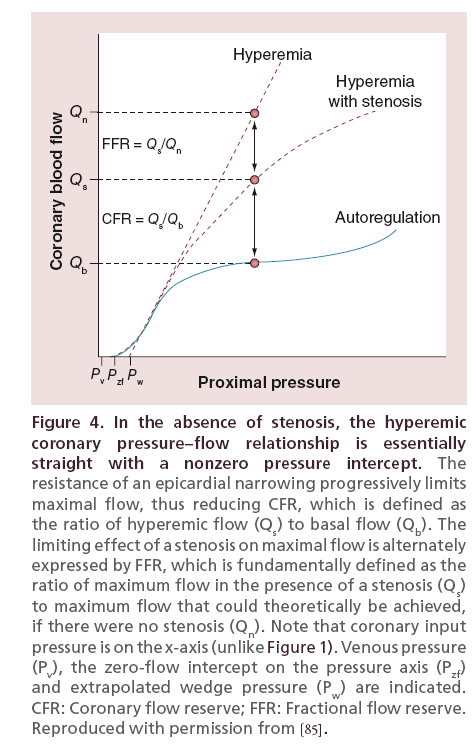
Although the prognostic relevance of CFR is undisputed [20,47,48], its application to clinical decision-making in the setting of PCI has been troublesome. Not only was CFR not introduced for the purpose of clinical decision-making regarding coronary revascularization, but also its application as such was hampered by its dependence on factors influencing the stability of resting conditions, such as volume loading conditions, contractility, tachycardia, and clinical conditions such as cardiac hypertrophy, anemia, hypoxia and fever [49,50]. FFR was subsequently introduced as a pressure-derived proxy measure of relative CFR: the pressure-derived estimate of flow in the stenosed artery, represented by the coronary pressure distal to the stenosis at maximal vasodilation, as a fraction of the pressure-derived estimate of flow in the same coronary artery without the stenosis, represented by the aortic pressure during maximal vasodilation (Figure 4) [51,52]. The use of coronary pressure measurements during maximal vasodilation as a surrogate of flow impairment was derived from the assumption that under conditions of maximal vasodilation a linear relationship exists between coronary pressure and flow (Figure 5) [53,54]. The introduction of FFR has boosted the role of physiology in the catheterization laboratory, mainly as a result of the practical ease of coronary pressure measurements in the catheterization lab, which are technically much less demanding and less time consuming than measurements of coronary flow velocity. Moreover, FFR is independent of resting hemodynamics, which was seen as a large advantage over the use of CFR [55–57]. Both FFR and CFR display equivalent diagnostic accuracy if compared with noninvasive stress testing [58–60]. Despite this equivalence, initial combined evaluations of FFR and CFR have noted a substantial frequency of disagreements between the two measures, which was contributed to the technical difficulties and diagnostic inefficiency of CFR [61,62]. Subsequent clinical evaluation of physiological assessment in the catheterization laboratory consequently focused on the use of FFR, and developments in invasive coronary flow assessment were largely put on hold. The use of FFR has subsequently shown to improve identification of hemodynamically severe coronary stenosis over coronary angiography, and it seems that stenosis deemed hemodynamically severe by FFR is better of treated by PCI than by OMT alone [5–9]. Nonetheless, as noted previously, the fact that a dominant part of FFR-positive lesions does not require revascularization up to 2 years of follow-up and the fact that FFR-negative stenosis suffers from adverse events in up to 10% of cases suggest the contribution of alternative factors than pressure-derived severity of coronary stenosis to the clinical consequences of IHD.
Physiological appraisal of IHD: stenosis assessment from a microvascular view
From pressure back to flow
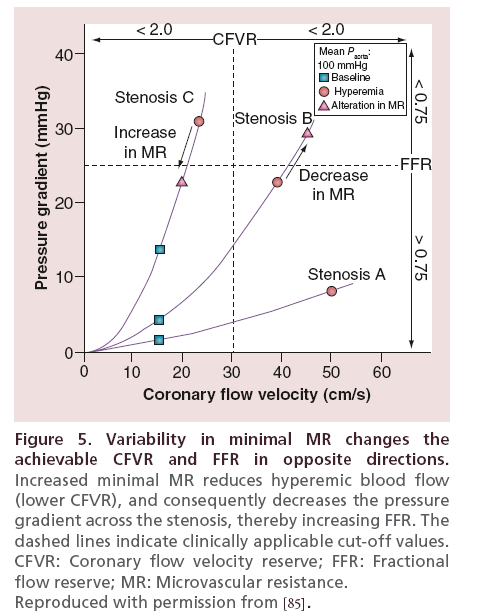
As noted previously, the magnitude of the transstenotic pressure gradient, the mainstay of FFR, depends on the magnitude of coronary flow through the stenosis during maximal vasodilation: the pressure drop increases with increasing maximal coronary flow, and vice versa. Hence, the higher the maximal transstenotic flow, the lower the FFR. In contrast, CFR increases with increasing maximal transstenotic flow: the higher maximal flow, the higher CFR. Since coronary flow is in turn dictated by microvascular function, a change in the latter influences CFR and FFR in opposite directions [62]. This illustrates how discordances between FFR and CFR can occur merely on the basis of basic stenosis physiology, and stresses the important contribution of microvascular function. Consequently, in contrast to the previous attribution of FFR/CFR discordance to diagnostic inefficiency of CFR, a body of evidence now supports that pertinent coronary patho-physiology underlies this phenomenon [61–64].
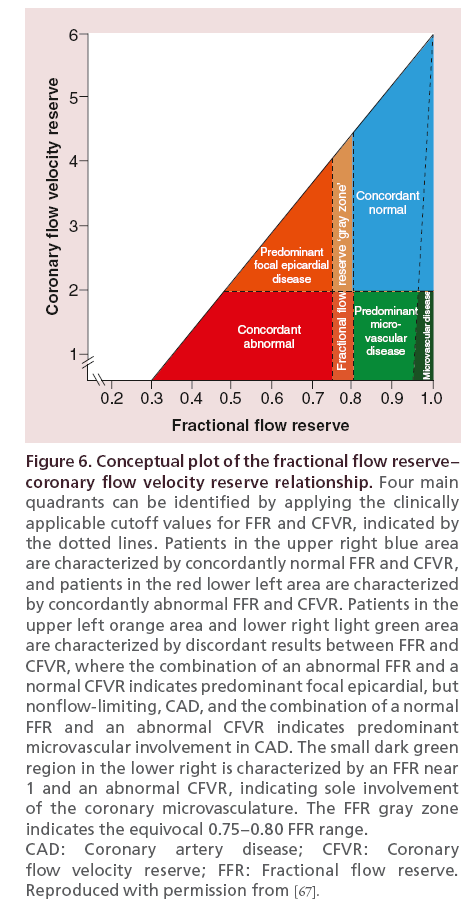
Considering the dichotomous evaluation of FFR and CFR, their agreement and discordance can be described as depicted in Figure 6. On one end of the spectrum, FFR and CFR are concordant and normal. In this situation, both the vasodilatory capacities of the coronary circulation are normal, and no pressure loss along the epicardial vessel occurs. On the other side of the spectrum, FFR and CFR are concordant and both below common interventional thresholds. In this situation, the vasodilator reserve capacity of the coronary circulation is diminished in the presence of a substantial epicardial narrowing that induces a significant pressure drop across the vessel. Amidst these extremes of the FFR/CFR relationship lie the discrepancies between FFR and CFR. On the one hand, FFR may be abnormal while CFR is normal. Here, the vasodilatory capacity of the circulation, and hence the available increase in transstenotic flow, are large as reflected by the normal CFR. Such large increases in coronary flow may induce significant pressure gradients, and thus abnormal FFR values, even in the presence of relatively trivial epicardial stenoses. Considering the high flow through the circulation, and the fact that flow governs myocardial function [14], these epicardial stenoses are nonflow limiting, and their relief by PCI is likely not indicated. On the other hand, FFR may be normal while CFR is below interventional thresholds [61], which may reflect three distinct pathophysiological patterns. First, this may represent a mild focal epicardial stenosis superimposed on a background of diffuse and/or microcirculatory disease. Second, this pattern may reflect pure diffuse disease, where abnormal FFR is unlikely in the absence of focal narrowing of the coronary artery. Finally, it may be a reflection of pure microcirculatory disease, which is likely when CFR is reduced in the presence of a near normal FFR (roughly 0.95 or greater).
Crucial in this interpretation is the role of the coronary microcirculation in the relationship between FFR and CFR, particularly in the setting of equivocal epicardial stenosis. Taking the dP-v curve of the stenosis as its fingerprint, largely determined by the geometrical properties of the stenosis, the position of the physiological assessment on the ΔP-v curve is defined by the extent of microvascular resistance. As, for a given stenosis, microvascular resistance alters, the position of the measurement will move along this stenosisspecific dP-v curve. When microvascular resistance increases, FFR values will increase and CFR values will decrease [62], and vice versa. Consequently, a change in the magnitude of microvascular resistance can alter FFR from functionally significant to nonsignificant, and vice versa.
This illustrates that discordance between FFR and CFR values does not originate from inefficiency of either tool, but reflects divergent extremes of epicardial and microvascular disease. The presence of discordance is not uncommon in clinical practice, as it occurs in up to 40% of cases [61,62] and yields important prognostic information. Considering the dominant role of coronary flow in myocardial function [14], the prognostic value of discordance between CFR and FFR is likely primarily determined by the magnitude of coronary flow. In agreement with this physiological background of discordance and the importance of flow, and the paramount prognostic value identified in large studies on noninvasively determined CFR [32,33,65,66], deferral of stenoses with discordance between FFR and CFR was documented to be associated with significantly increased MACE rates at 10-year follow-up compared with concordant normal FFR and CFR results [67]. The combination of an abnormal FFR with a normal CFR, indicating predominant focal but nonflow-limiting epicardial disease, was associated with equivalent clinical outcome compared with concordant normal FFR and CFR. In contrast, a normal FFR and an abnormal CFR, indicating predominant microvascular disease, was associated with significantly higher frequency of MACE compared with concordantly normal FFR and CFR, already early after deferral of revascularization. Nonetheless, although these data were derived from a retrospective analysis of unique data derived from the pre-FFR era, it comprised a relatively small number of patients. To confirm the hypotheses on the relevance of FFR/CFR discordance regarding clinical outcomes, the large prospective multicenter Combined Pressure and Flow Measurements to Guide Treatment of Coronary Stenoses study (DEFINE-FLOW; NCT: NCT02328820) is now actively enrolling. In DEFINE-FLOW, patients referred for invasive assessment of coronary stenoses will be evaluated using a sensor-equipped guide wire with both a pressure and flow velocity sensor (ComboWire, Volcano Corporation, CA, USA). Whereas stenosis in which FFR and CFR are concordantly abnormal is considered ischemia generating, and will be treated by PCI, treatment will be deferred in all other stenoses. DEFINE-FLOW thereby aims to document the clinical pertinence of FFR/CFR discordance on a 2-year MACE end point.
Selective evaluation of epicardial & microvascular contribution to flow impairment
New insights in the diagnostic and prognostic importance of elevated microvascular resistance have increased interest in novel physiological indices that enable the evaluation of microvascular function. Moreover, the obscuring effect of microvascular function on the FFRguided identification of ischemia-generating stenoses has raised interest in more stenosis-specific parameters [62,64]. Coronary pressure or flow-based assessment by means of FFR or CFR does not allow to selectively identify alterations in epicardial or microvascular resistance to coronary flow. FFR represents a stenosis-oriented physiological parameter that is by definition unable to assess the coronary microvasculature selectively. Moreover, FFR values are influenced by alterations in microvascular resistance, as discussed previously, and are therefore not stenosis-specific. Furthermore, CFR results from the effect of both epicardial and microvascular impairment of coronary flow. Hence, in the presence of epicardial obstructions, the relative contribution of the epicardial and microvascular domains of the coronary circulation to the impairment of flow reserve cannot be elucidated by CFR. In the absence of epicardial lesions, CFR reflects microvascular vasodilator function, and is closely related to clinical outcomes [32,33,64,65]. However, microvascular function imparts an important diagnostic and prognostic value also in case of concomitant epicardial disease [67].
With the introduction of dual sensor-equipped guide wires, simultaneous pressure and flow measurements have introduced the opportunity not only to measure FFR and CFR at once, but also to selectively evaluate the epicardial and microvascular contribution to coronary flow impairment. The introduction of this innovation resulted in novel physiological parameters like hyperemic stenosis resistance index (HSR) and hyperemic microvascular resistance index (HMR) that selectively identify epicardial disease severity, and the degree of microvascular resistance, respectively. HSR is defined as the ratio of the average pressure gradient to the baseline average peak flow during a hyperemic state ([Paorta – Pdistal]/mean Qdistal). An HSR interventional threshold of more than 0.8 mm Hg/cm was documented to have better diagnostic accuracy to detect reversible perfusion defects on myocardial perfusion scintigraphy as compared with traditional physiological indices like CFR and FFR [68]. HMR is defined as the ratio of hyperemic mean distal coronary pressure to mean distal coronary flow velocity (mean Pdistal/ mean Qdistal) and enables the selective identification of microvascular resistance. Such an index of microcirculatory resistance is likely less dependent on hemodynamic changes compared with CFR, most likely as a result of their independence from basal hemodynamic conditions. Notably, elevated HMR values distal to a coronary stenosis are associated with irreversible perfusion defects on MPS [13]. Alternatively, the coronary thermodilution technique can be applied to obtain the index of microcirculatory resistance (IMR), defined as the ratio of distal pressure to the inverse of hyperemic Tmn, IMR provides a well-validated alternative to assess microcirculatory function [69,70]. However, recent data suggest that HMR may provide incremental diagnostic efficiency as compared with IMR for MRI-defined myocardial perfusion abnormalities [71]. Regardless of potential differences between IMR and HMR, these advanced physiological indices, together with HSR, FFR and CFR, allow a comprehensive evaluation of the presence and origin of IHD. With the documentation of a limited benefit of mechanical relief of FFR-positive stenosis in FAME II, and the concomitant documentation of a relatively high event rate in FFR-negative vessels, more comprehensive evaluation of the coronary circulation by these tools is likely the next frontier in clinical coronary physiology. Considering the dominant role of microvascular function in myocardial function and dysfunction, it is likely that a view on CAD severity from the microcirculation is the missing link between angiographically determined CAD and clinical outcomes in IHD.
The pertinence of the microcirculation in acute coronary syndrome
Until now, we have discussed the role of the coronary microcirculation in the pathophysiology, diagnosis and prognosis in the setting of stable IHD. Although this setting remains the most validated setting for physiological assessment of disease severity, interest is increasing in the use of physiological tools during the acute and subacute phase of acute coronary syndromes (ACS). Including unstable angina (UA) pectoris, non-ST-segment myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI), the spectrum of ACS reflects a continuum of microvascular dysfunction. In the setting of STEMI, direct ischemic effects as well as neurohumoral factors that apply to both ischemic and remote myocardial territories impair coronary microvascular function in both the acute and subacute phase of myocardial infarction. Bax et al. documented panmyocardial microvascular dysfunction in STEMI leading to an increased minimal microvascular resistance and reduced maximal coronary flow in both the infarctrelated as well as the nonculprit vessel, which gradually recovered over the course of 6 months [72]. Such panmyocardial microvascular dysfunction therefore likely impairs the diagnostic efficiency of nonstenosis-specific indices of IHD severity such as FFR in the acute phase of STEMI. These considerations should be borne in mind when these indices are applied to the individual patient in clinical practice.
In contrast to STEMI, the microvascular vasodilatory capacity in patients with NSTEMI and UA pectoris appears to remain preserved, although more limited mechanistic data are available [73]. Initial clinical experience supports the use of FFR to facilitate decision-making in NSTEMI patients over angiographic guidance [74], although larger trials are needed to confirm the benefit of FFR-guided intervention in NSTEMI in terms of clinical outcomes. Nonetheless, as it is likely that the magnitude of microvascular dysfunction relates to the severity of the ischemic event. Niccoli et al. documented an impaired diagnostic efficiency of FFR in the acute phase of NSTEMI in comparison with a stenosis-specific evaluation of stenosis severity using HSR, which is manifested by an increase in microvascular resistance that correlated with serum CRP levels [75]. In conclusion, it seems prudent to consider microvascular dysfunction in NSTEMI and UA patients, and to perform retesting of physiological severity of coronary stenosis at follow-up, once microvascular function has gradually restored.
In general, it has to be considered that ACS represents a spectrum of microvascular dysfunction secondary to the ischemic event that expands beyond the infarct-related artery and the ischemic myocardium. As such, the use of combined pressure and flow measurements yields an opportunity to identify the extent of physiological epicardial disease severity, as well as the functional status of the coronary microvasculature in the individual patient. With such a comprehensive approach, physiological testing goes beyond relying on empirically defined benefit of coronary pressure as an estimate of coronary flow impairment, and allows to identify actual disease status in the individual patient.
Conclusion
Increasing acknowledgement of the complex patho-physiology of IHD has raised interest in comprehensive physiological assessment of the coronary circulation by means of combined invasive assessment of coronary pressure and flow. The pivotal role of the coronary microcirculation in myocardial function, and, hence, in the clinical sequelae of myocardial underperfusion, mandates its objective assessment as part of clinical diagnosis of IHD. Physiological indices like FFR and CFR are, as single diagnostic modalities, not capable to objectify the relative contribution of the epicardial and microvascular compartment of the coronary circulation to diminished myocardial perfusion, and therefore solitarily do not suffice to optimally objectify the presence and origin of IHD. Their combined assessment advances the information that can be derived from physiological assessment of the coronary circulation, where the discordance between FFR and CFR identifies pertinent coronary pathophysiology related to the functional status of the coronary microvasculature. Nonetheless, the simultaneous assessment of coronary pressure and flow also enables the selective evaluation of resistance to coronary flow induced by the epicardial artery and the coronary microcirculation. With evidence for their pertinence increasing, clinical application of these advanced measures of coronary function may advance diagnosis and treatment of IHD patients.
Future perspective
More than three decades of clinical research focused mainly on the identification and revascularization of epicardial coronary stenosis as the mainstay of IHD. However, accumulating evidence demonstrates the pivotal contribution of microvascular disease onto the genesis of myocardial ischemia and its clinical sequelae. The pressure-derived FFR has become a routine tool in daily clinical practice to guide revascularization in patients with IHD, though it focuses solely on epicardial origin of myocardial perfusion impairment. Dual-sensor-equipped guide wires allow simultaneous assessment of coronary flow and pressure to obtain a comprehensive evaluation of the coronary vasculature. Such comprehensive assessment of the coronary circulation is likely to improve the diagnosis of IHD, and, hence, selection of those patients in whom mechanical revascularization may provide substantial clinical benefit beyond a more pronounced and timely reduction in angina complaints. For this purpose, a more prominent role of coronary flow in the diagnostic strategies regarding IHD is required. As discussed, the invasive assessment of coronary flow remains hampered by their technical underdevelopment in comparison with coronary pressure measurements. Nonetheless, together with the cardiology community, industrial partners are gaining awareness on the importance of coronary flow and microvascular function assessment for daily clinical practice, and are now restarting technological developments in the field of invasive physiological assessment. On the other hand, advanced noninvasive imaging techniques are being developed that allow the evaluation of regional flow and flow reserve, and may serve as a flow-based gatekeeper before invasive angiography and vessel-specific comprehensive physiological testing is performed. If flow determines function and dysfunction of the myocardium, such a flow-based approach may not only improve patient-related outcomes in stable IHD patients, but may also limit patient burden associated with the diagnostic process in IHD.
The comprehensive approach to IHD discussed in this review likely provides a more complete evaluation of IHD and its origin. Although it’s inequivalent economic and clinical benefit, the adoption of physiology- guided PCI remains limited in clinical practice due to practical ambiguities. As a consequence, several investigators are directing their efforts at simplification of such physiological assessment. A common approach is found in physiological indices that do not require the administration of potent vasodilators and allow physiological testing in resting conditions. These approaches overcome many of the limitations associated with a requisite hyperemic state, which is the case for FFR and CFR, and thereby likely limit procedural time and patient burden associated with physiological assessment in the catheterization laboratory. Among these approaches are the basal stenosis resistance index (BSR), which applies combined pressure and flow velocity measures to calculate the resistance induced by the epicardial coronary segment during resting conditions [76,77]. BSR was documented to provide equivalent diagnostic accuracy as FFR against noninvasive myocardial perfusion imaging. Another vasodilator-free approach to physiological testing is the instantaneous wave-free ratio (IFR), which equals the distal coronary to aortic pressure ratio during a restricted time window in cardiac diastole termed the wave-free period [76,78–81]. IFR has repeatedly shown to agree with FFR in 80% of cases, and data are emerging that it even provides a more accurate reflection of the vasodilator capacity of the coronary circulation than FFR [79]. These vasodilatorfree approaches may well improve adoption of physiological testing in clinical practice, while technical advances in coronary flow assessment are awaited to boost clinical application of simultaneous coronary pressure and flow measurements.
Financial & competing interests disclosure
MA van Lavieren, TP van de Hoef and JJ Piek have served as speakers at educational events organized by either Volcano, St. Jude Medical, and Boston Scientific, manufacturers of sensor- equipped guide wires. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript.
Executive summary
The relevance of the coronary microcirculation
• Ischemic heart disease (IHD) originates from obstructive and nonobstructive abnormalities present in the succeeding perfusion domains of the vascular tree.
Physiological appraisal of IHD: stenosis assessment from a microvascular view
• Fractional flow reserve (FFR) and coronary flow reserve (CFR) disagree in 40% of the cases. Discordance reflects divergent extremes of epicardial and microvascular disease, which hold pivotal prognostic value.
Selective evaluation of epicardial and microvascular contribution to flow impairment
• FFR and CFR solitarily do not suffice to optimally objectify the presence and origin of IHD, but combined deliver a comprehensive intracoronary assessment of IHD.
Conclusion & future perspective
• Combined measurements are mandated for selective evaluation of epicardial lesions that are likely to benefit from mechanical revascularization. We recommend critical revision of the epicardial-orientated diagnostic and therapeutic guidelines with regard to the IHD.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- Task Force on Myocardial Revascularization of theEuropean Society of Cardiology (ESC) and the European Association forCardio-Thoracic Surgery (EACTS), European Association for Percutaneous CardiovascularInterventions (EAPCI), Wijns W et al. Guidelines on myocardial revascularization. Eur. Heart J. 31(20), 2501–2555 (2010).
- Van De Hoef TP, Van Lavieren MA, Henriques JP, Piek JJ, Claessen BE. Fractional flow reserve-guided percutaneous coronary intervention: does coronary pressure never lie? Curr. Treat. Options Cardiovasc. Med. 16(4), 294 (2014).
- De Bruyne B, Baudhuin T, Melin JA et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation 89(3), 1013–1022 (1994).
- Pijls NH, De Bruyne B, Peels K et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N. Engl. J. Med. 334(26), 1703–1708 (1996).
- Pijls NH, Fearon WF, Tonino PA et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the fame (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J. Am. Coll. Cardiol. 56(3), 177–184 (2010).
- Tonino PA, Fearon WF, De Bruyne B et al. Angiographic versus functional severity of coronary artery stenoses in the fame study fractional flow reserve versus angiography in multivessel evaluation. J. Am. Coll. Cardiol. 55(25), 2816–2821 (2010).
- Fearon WF, Bornschein B, Tonino PA et al. Economic evaluation of fractional flow reserve-guided percutaneous coronary intervention in patients with multivessel disease. Circulation 122(24), 2545–2550 (2010).
- De Bruyne B, Pijls NH, Kalesan B et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N. Engl. J. Med. 367(11), 991–1001 (2012).
- De Bruyne B, Fearon WF, Pijls NH et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N. Engl. J. Med. 371(13), 1208–1217 (2014).
- Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121(21), 2317–2325 (2010).
- Camici PG, Crea F. Coronary microvascular dysfunction. N. Engl. J. Med. 356(8), 830–840 (2007).
- Marzilli M, Merz CN, Boden WE et al. Obstructive coronary atherosclerosis and ischemic heart disease: an elusive link. J. Am. Coll. Cardiol. 60(11), 951–956 (2012).
- Nolte F, Van De Hoef TP, Meuwissen M et al. Increased hyperaemic coronary microvascular resistance adds to the presence of myocardial ischaemia. EuroIntervention 9(12), 1423–1431 (2014).
- Smalling RW, Kelley K, Kirkeeide RL, Fisher DJ. Regional myocardial function is not affected by severe coronary depressurization provided coronary blood flow is maintained. J. Am. Coll. Cardiol. 5(4), 948–955 (1985).
- Tiefenbacher CP, Chilian WM. Heterogeneity of coronary vasomotion. Basic Res. Cardiol. 93(6), 446–454 (1998).
- Mosher P, Ross J, Jr., Mcfate PA, Shaw RF. Control of coronary blood flow by an autoregulatory mechanism. Circ. Res. 14, 250–259 (1964).
- Marcus ML, Chilian WM, Kanatsuka H, Dellsperger KC, Eastham CL, Lamping KG. Understanding the coronary circulation through studies at the microvascular level. Circulation 82(1), 1–7 (1990).
- Westerhof N, Boer C, Lamberts RR, Sipkema P. Cross-talk between cardiac muscle and coronary vasculature. Physiol. Rev. 86(4), 1263–1308 (2006).
- Spaan JA, Piek JJ, Hoffman JI, Siebes M. Physiological basis of clinically used coronary hemodynamic indices. Circulation 113(3), 446–455 (2006).
- Gould KL, Lipscomb K. Effects of coronary stenoses on coronary flow reserve and resistance. Am. J. Cardiol. 34(1), 48–55 (1974).
- Gould KL, Lipscomb K, Calvert C. Compensatory changes of the distal coronary vascular bed during progressive coronary constriction. Circulation 51(6), 1085–1094 (1975).
- Uren NG, Melin JA, De Bruyne B, Wijns W, Baudhuin T, Camici PG. Relation between myocardial blood flow and the severity of coronary-artery stenosis. N. Engl. J. Med. 330(25), 1782–1788 (1994).
- Camici PG, D’amati G, Rimoldi O. Coronary microvascular dysfunction: mechanisms and functional assessment. Nat. Rev. Cardiol. 12(1), 48–62 (2015).
- Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur. Heart J. 35(17), 1101–1111 (2014).
- Patel B, Fisher M. Therapeutic advances in myocardial microvascular resistance: unravelling the enigma. Pharmacol. Ther. 127(2), 131–147 (2010).
- Van Lavieren MA, Van De Hoef TP, Piek JJ. Primary PCI: time to change focus from epicardial reperfusion towards protection of the microvasculature. EuroIntervention 10(Suppl. T), T39–T46 (2014).
- Geltman EM, Henes CG, Senneff MJ, Sobel BE, Bergmann SR. Increased myocardial perfusion at rest and diminished perfusion reserve in patients with angina and angiographically normal coronary arteries. J. Am. Coll. Cardiol. 16(3), 586–595 (1990).
- Reis SE, Holubkov R, Conrad Smith AJ et al. Coronary microvascular dysfunction is highly prevalent in women with chest pain in the absence of coronary artery disease: results from the NHLBI WISE study. Am. Heart J. 141(5), 735–741 (2001).
- Britten MB, Zeiher AM, Schachinger V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron. Artery Dis. 15(5), 259–264 (2004).
- Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N. Engl. J. Med. 349(11), 1027–1035 (2003).
- Fukushima K, Javadi MS, Higuchi T et al. Prediction of short-term cardiovascular events using quantification of global myocardial flow reserve in patients referred for clinical 82Rb PET perfusion imaging. J. Nucl. Med. 52(5), 726–732 (2011).
- Herzog BA, Husmann L, Valenta I et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J. Am. Coll. Cardiol. 54(2), 150–156 (2009).
- Murthy VL, Naya M, Foster CR et al. Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation 124(20), 2215–2224 (2011).
- Neglia D, Michelassi C, Trivieri MG et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation 105(2), 186–193 (2002).
- Pepine CJ, Anderson RD, Sharaf BL et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia results from the national heart, lung and blood institute wise (women’s ischemia syndrome evaluation) study. J. Am. Coll. Cardiol. 55(25), 2825–2832 (2010).
- Boden WE, O’rourke RA, Teo KK et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 356(15), 1503–1516 (2007).
- Shaw LJ, Berman DS, Maron DJ et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (courage) trial nuclear substudy. Circulation 117(10), 1283–1291 (2008).
- De Bruyne B, Pijls NH, Smith L, Wievegg M, Heyndrickx GR. Coronary thermodilution to assess flow reserve: experimental validation. Circulation 104(17), 2003–2006 (2001).
- Aarnoudse W, Van’t Veer M, Pijls NH et al. Direct volumetric blood flow measurement in coronary arteries by thermodilution. J. Am. Coll. Cardiol. 50(24), 2294–2304 (2007).
- Pijls NH, De Bruyne B, Smith L et al. Coronary thermodilution to assess flow reserve: validation in humans. Circulation 105(21), 2482–2486 (2002).
- Melikian N, Kearney MT, Thomas MR, De Bruyne B, Shah AM, Maccarthy PA. A simple thermodilution technique to assess coronary endothelium-dependent microvascular function in humans: validation and comparison with coronary flow reserve. Eur. Heart J. 28(18), 2188–2194 (2007).
- Fearon WF, Farouque HM, Balsam LB et al. Comparison of coronary thermodilution and doppler velocity for assessing coronary flow reserve. Circulation 108(18), 2198–2200 (2003).
- Barbato E, Aarnoudse W, Aengevaeren WR et al. Validation of coronary flow reserve measurements by thermodilution in clinical practice. Eur. Heart J. 25(3), 219–223 (2004).
- Cortigiani L, Rigo F, Galderisi M et al. Diagnostic and prognostic value of doppler echocardiographic coronary flow reserve in the left anterior descending artery in hypertensive and normotensive patients [corrected]. Heart 97(21), 1758–1765 (2011).
- Cortigiani L, Rigo F, Gherardi S et al. Coronary flow reserve during dipyridamole stress echocardiography predicts mortality. JACC Cardiovasc. Imaging 5(11), 1079–1085 (2012).
- Cortigiani L, Rigo F, Gherardi S, Bovenzi F, Picano E, Sicari R. Implication of the continuous prognostic spectrum of doppler echocardiographic derived coronary flow reserve on left anterior descending artery. Am. J. Cardiol. 105(2), 158–162 (2010).
- Gould KL, Lipscomb K, Hamilton GW. Physiologic basis for assessing critical coronary stenosis. Instantaneous flow response and regional distribution during coronary hyperemia as measures of coronary flow reserve. Am. J. Cardiol. 33(1), 87–94 (1974).
- Hoffman JI. Maximal coronary flow and the concept of coronary vascular reserve. Circulation 70(2), 153–159 (1984).
- Hoffman JI. Problems of coronary flow reserve. Ann. Biomed. Eng. 28(8), 884–896 (2000).
- Gould KL. Does coronary flow trump coronary anatomy? JACC Cardiovasc. Imaging 2(8), 1009–1023 (2009).
- Johnson NP, Toth GG, Lai D et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J. Am. Coll. Cardiol. 64(16), 1641–1654 (2014).
- Pijls NH, Van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation 87(4), 1354–1367 (1993).
- Di Mario C, Krams R, Gil R, Serruys PW. Slope of the instantaneous hyperemic diastolic coronary flow velocity-pressure relation. A new index for assessment of the physiological significance of coronary stenosis in humans. Circulation 90(3), 1215–1224 (1994).
- Spaan JA. Coronary diastolic pressure-flow relation and zero flow pressure explained on the basis of intramyocardial compliance. Circ. Res. 56(3), 293–309 (1985).
- Mcginn AL, White CW, Wilson RF. Interstudy variability of coronary flow reserve. Influence of heart rate, arterial pressure, and ventricular preload. Circulation 81(4), 1319–1330 (1990).
- Rossen JD, Winniford MD. Effect of increases in heart rate and arterial pressure on coronary flow reserve in humans. J. Am. Coll. Cardiol. 21(2), 343–348 (1993).
- De Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation 94(8), 1842–1849 (1996).
- Joye JD, Schulman DS, Lasorda D, Farah T, Donohue BC, Reichek N. Intracoronary Doppler guide wire versus stress single-photon emission computed tomographic thallium-201 imaging in assessment of intermediate coronary stenoses. J. Am. Coll. Cardiol. 24(4), 940–947 (1994).
- Miller DD, Donohue TJ, Wolford TL, Kern MJ, Bergmann SR. Assessment of blood flow distal to coronary artery stenoses. Correlations between myocardial positron emission tomography and poststenotic intracoronary Doppler flow reserve. Circulation 94(10), 2447–2454 (1996).
- Miller DD, Donohue TJ, Younis LT et al. Correlation of pharmacological 99mTc-sestamibi myocardial perfusion imaging with poststenotic coronary flow reserve in patients with angiographically intermediate coronary artery stenoses. Circulation 89(5), 2150–2160 (1994).
- Johnson NP, Kirkeeide RL, Gould KL. Is discordance of coronary flow reserve and fractional flow reserve due to methodology or clinically relevant coronary pathophysiology? JACC Cardiovasc. Imaging 5(2), 193–202 (2012).
- Meuwissen M, Chamuleau SA, Siebes M et al. Role of variability in microvascular resistance on fractional flow reserve and coronary blood flow velocity reserve in intermediate coronary lesions. Circulation 103(2), 184–187 (2001).
- Echavarria-Pinto M, Escaned J, Macias E et al. Disturbed coronary hemodynamics in vessels with intermediate stenoses evaluated with fractional flow reserve: a combined analysis of epicardial and microcirculatory involvement in ischemic heart disease. Circulation 128(24), 2557–2566 (2013).
- Van De Hoef TP, Nolte F, Echavarria-Pinto M et al. Impact of hyperaemic microvascular resistance on fractional flow reserve measurements in patients with stable coronary artery disease: insights from combined stenosis and microvascular resistance assessment. Heart 100(12), 951–959 (2014).
- Murthy VL, Naya M, Foster CR et al. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 126(15), 1858–1868 (2012).
- Murthy VL, Naya M, Taqueti VR et al. Effects of sex on coronary microvascular dysfunction and cardiac outcomes. Circulation 129(24), 2518–2527 (2014).
- Van De Hoef TP, Van Lavieren MA, Damman P et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ. Cardiovasc. Interv. 7(3), 301–311 (2014).
- Meuwissen M, Siebes M, Chamuleau SA et al. Hyperemic stenosis resistance index for evaluation of functional coronary lesion severity. Circulation 106(4), 441–446 (2002).
- Fearon WF, Balsam LB, Farouque HM et al. Novel index for invasively assessing the coronary microcirculation. Circulation 107(25), 3129–3132 (2003).
- Ng MK, Yeung AC, Fearon WF. Invasive assessment of the coronary microcirculation: superior reproducibility and less hemodynamic dependence of index of microcirculatory resistance compared with coronary flow reserve. Circulation 113(17), 2054–2061 (2006).
- Williams RPDSK. Lumley M, Asrress K et al. Doppler indices of resistance are superior to thermodilution indices at predicting coronary microvascular dysfunction. J. Am. Coll. Cardiol. 65(10S), 3 (2015).
- Bax M, De Winter RJ, Koch KT, Schotborgh CE, Tijssen JG, Piek JJ. Time course of microvascular resistance of the infarct and noninfarct coronary artery following an anterior wall acute myocardial infarction. Am. J. Cardiol. 97(8), 1131–1136 (2006).
- Layland J, Carrick D, Mcentegart M et al. Vasodilatory capacity of the coronary microcirculation is preserved in selected patients with non-ST-segment-elevation myocardial infarction. Circ. Cardiovasc. Interv. 6(3), 231–236 (2013).
- Layland J, Oldroyd KG, Curzen N et al. Fractional flow reserve vs. angiography in guiding management to optimize outcomes in non-ST-segment elevation myocardial infarction: The British Heart Foundation FAMOUS– NSTEMI randomized trial. Eur. Heart J. 36(2), 100–111 (2015).
- Niccoli G, Falcioni E, Cosentino N et al. Impact of accuracy of fractional flow reserve to reduction of microvascular resistance after intracoronary adenosine in patients with angina pectoris or non-ST-segment elevation myocardial infarction. Am. J. Cardiol. 113(9), 1461–1467 (2014).
- Van De Hoef TP, Meuwissen M, Escaned J et al. Head-to-head comparison of basal stenosis resistance index, instantaneous wave-free ratio, and fractional flow reserve: diagnostic accuracy for stenosis-specific myocardial ischaemia. EuroIntervention doi:10.4244/EIJY14M08_17 (2014) (Epub ahead of print).
- Van De Hoef TP, Nolte F, Damman P et al. Diagnostic accuracy of combined intracoronary pressure and flow velocity information during baseline conditions: adenosine-free assessment of functional coronary lesion severity. Circ. Cardiovasc. Interv. 5(4), 508–514 (2012).
- Petraco R, Escaned J, Sen S et al. Classification performance of instantaneous wave-free ratio (IFR) and fractional flow reserve in a clinical population of intermediate coronary stenoses: results of the advise registry. EuroIntervention 9(1), 91–101 (2013).
- Petraco R, Van De Hoef TP, Nijjer S et al. Baseline instantaneous wave-free ratio as a pressure-only estimation of underlying coronary flow reserve: results of the justify-CFR study (joined coronary pressure and flow analysis to determine diagnostic characteristics of basal and hyperemic indices of functional lesion severity-coronary flow reserve). Circ. Cardiovasc. Interv. 7(4), 492–502 (2014).
- Sen S, Asrress KN, Nijjer S et al. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of clarify (classification accuracy of pressure-only ratios against indices using flow study). J. Am. Coll. Cardiol. 61(13), 1409–1420 (2013).
- Sen S, Escaned J, Malik IS et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the advise (adenosine vasodilator independent stenosis evaluation) study. J. Am. Coll. Cardiol. 59(15), 1392–1402 (2012).
- Duncker DJ, Bache RJ. Effect of chronotropic and inotropic stimulation on the coronary pressure–flow relation in left ventricular hypertrophy. Basic Res. Cardiol. 92(4), 271–286 (1997).
- Jeremy RW, Hughes CF, Fletcher PJ. Effects of left ventricular diastolic pressure on the pressure-flow relation of the coronary circulation during physiological vasodilatation. Cardiovasc. Res. 20(12), 922–930 (1986).
- Duncker DJ, Zhang J, Pavek TJ, Crampton MJ, Bache RJ. Effect of exercise on coronary pressure-flow relationship in hypertrophied left ventricle. Am. J. Physiol. 269(1 Pt 2), H271–H281 (1995).
- Van De Hoef TP, Meuwissen M, Escaned J et al. Fractional flow reserve as a surrogate for inducible myocardial ischaemia. Nat. Rev. Cardiol. 10(8), 439–452 (2013).
• The study by Pijls et al. revolutionized the assessment of intermediate coronary lesions in clinical practice. Pijls et al. demonstrated the inequivalent benefit of fractional flow reserve (FFR)-guided revascularization over angiography-guided revascularization of intermediate lesions.
• The FAME II study proved that percutaneous coronary intervention (PCI) + optimal medical therapy (OMT) exceed solitary OMT treatment in terms of clinical outcome. This study proves the benefit of additional PCI treatment in patients with hemodynamic significant lesions.
•• Johnson et al. documented that discordance between coronary flow reserve (CFR) and FFR reflects coronary pathophysiology and does not results from failure of the physiologic indices.
• This study demonstrated that the physiological indices are affected by variability in microvascular resistance. Meeuwissen et al. showed that FFR and CFR are affected in opposite direction by increases in coronary microvascular resistance.
• The study by Echavarria-Pinto et al. demonstrated the presence of abnormal microvascular hemodynamics that associate with ischemic heart disease (IHD) in a substantial number of patients with nonhemodynamic significant lesions as assessed by FFR.
•• This article issues the long-term MACE outcome of discordant FFR and CFR values. This unique dataset demonstrates the importance of a preserved coronary flow for beneficial prognostic outcome, even in the presence of a pressure-assessed functional lesion.
•• The study by Sen et al. introduced the concept of instantaneous wave-free ratio. This research group demonstrated that during the diastolic wave-free period, when coronary resistance is constant and minimal, adenosine-free pressure-derived assessment of coronary lesions correlated exquisite with FFR.