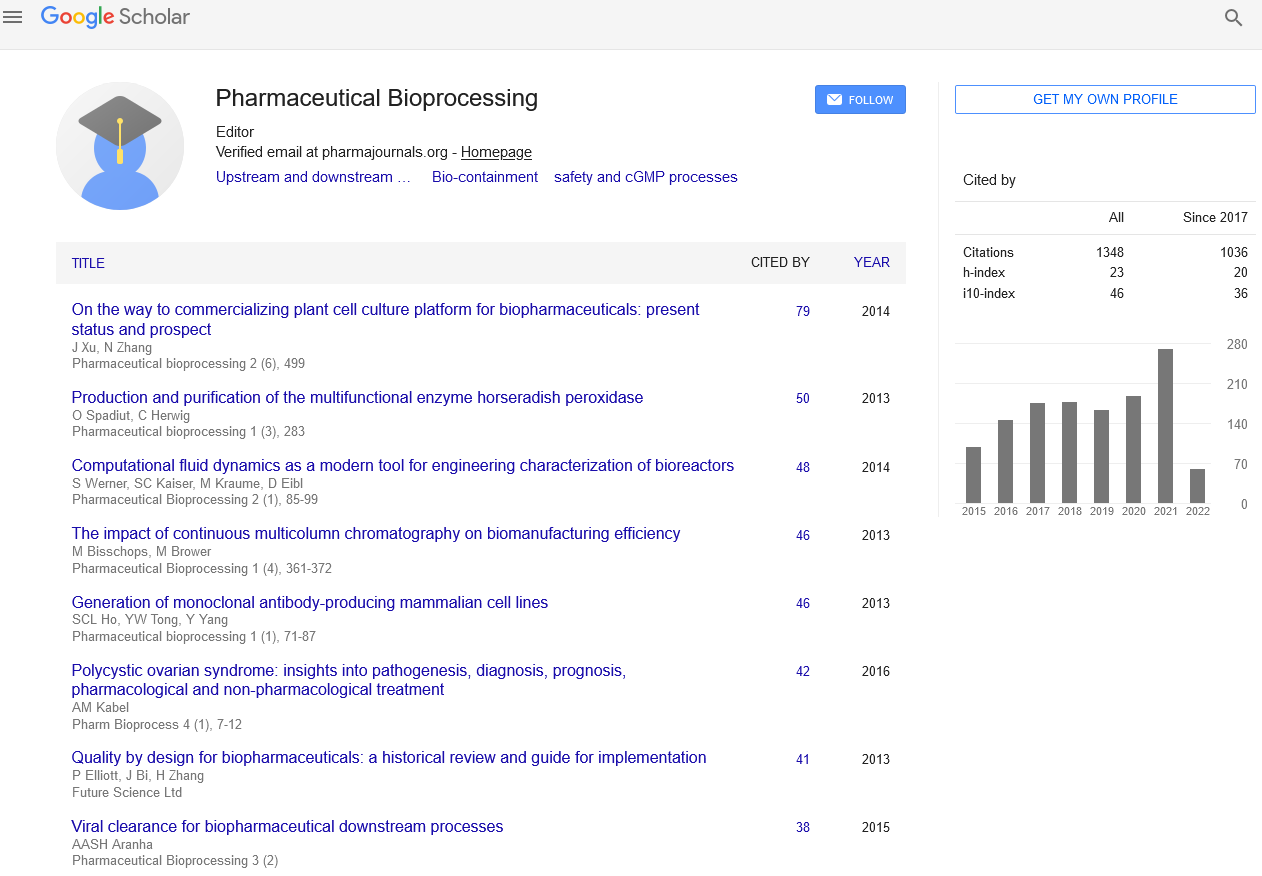
Review Article - Pharmaceutical Bioprocessing (2016) Volume 4, Issue 1
Polycystic Ovarian Syndrome: Insights Into Pathogenesis, Diagnosis, Prognosis, Pharmacological And Non-Pharmacological Treatment
- Corresponding Author:
- Ahmed M Kabel
Department of Pharmacology, Faculty of Medicine, Tanta University, Tanta, Egypt
E-mail: drakabel@gmail.com
Abstract
Keywords
PCOS, pathogenesis, diagnosis, tyreatment
Introduction
Polycystic ovarian syndrome (PCOS) is one of the most common female endocrine disorders. PCOS is a complex heterogeneous disorder of uncertain etiology, but there is strong evidence that it can, to a large degree, be classified as a genetic disease. Other names for this syndrome include polycystic ovary disease, functional ovarian hyperandrogenism, ovarian hyperthecosis, sclerocystic ovary syndrome and Stein-Leventhal syndrome [1,2].
The condition was first described in 1935 by the American gynecologists Irving F Stein and Michael L Leventhal, from whom its original name of Stein-Leventhal syndrome was taken. The earliest published description of a patient with what is now recognized as PCOS was in 1721 in Italy. Cyst-related changes to the ovaries were described in 1844 [3].
PCOS produces symptoms in approximately 5-10% of women of reproductive age (12– 45 years old). It is thought to be one of the leading causes of female subfertility and the most frequent endocrine problem in women of reproductive age [4,5].
The main features of PCOS are anovulation, hyperandrogenism and insulin resistance. Anovulation results in irregular menstruation, amenorrhea, ovulation-related infertility and polycystic ovaries. Hyperandrogenism results in acne and hirsutism. Insulin resistance is often associated with obesity, Type 2 diabetes, and high cholesterol levels. The symptoms and severity of the syndrome vary greatly among the affected women. Moreover, it may affect daily physical activities [6].
Epidemiology of PCOS
The prevalence of PCOS depends on the choice of diagnostic criteria. The World Health Organization estimates that it affects 116 million women worldwide as of 2010 (3.4% of the population). One community-based prevalence study using the Rotterdam criteria found that about 18% of women had PCOS and that 70% of them were previously undiagnosed [7].
Predisposing factors for PCOS
The predisposing factors for PCOS include the following [8]:
Genetic factors: Family history of PCOS.
High maternal androgen: Prenatal exposure to androgens poorly controlled maternal congenital adrenal hyperplasia, Androgen-secreting tumors, Low birth weight/small for gestational age, Premature adrenarche.
Endocrinal factors: Onset of type 1 diabetes mellitus before menarche, insulin resistance and obesity.
Drugs: such as anti-epileptic drugs (e.g., Valproate).
PCOS is a complex disorder of uncertain etiology. There is strong evidence that it is a genetic disease. Such evidence includes the familial clustering of cases, greater incidence in monozygotic than in dizygotic twins and heritability of endocrine and metabolic features of PCOS [1].
The genetic component appears to be inherited in an autosomal dominant fashion. This means that each child has a 50% chance of inheriting the predisposing genetic variant(s) from a parent. The genetic variant(s) can be inherited from either the father or the mother and can be passed along to both sons (who may be asymptomatic carriers or may have symptoms such as early baldness and/or excessive hair) and daughters who will show signs of PCOS. The genetic variant manifests itself at least via elevated androgen levels secreted by ovarian follicle theca cells. The exact gene affected has not yet been identified. The clinical severity of PCOS symptoms appears to be largely determined by factors such as obesity [9,10].
Pathogenesis of PCOS
Polycystic ovaries develop when the ovaries are stimulated to produce excessive amounts of male hormones (androgens), particularly testosterone, by either the release of excessive luteinizing hormone by the anterior pituitary gland, high levels of insulin in the blood (hyperinsulinaemia) in women whose ovaries are sensitive to this stimulus or reduced levels of sexhormone binding globulin (SHBG) resulting in increased free androgens [9].
The syndrome acquired its name due to the common sign on ultrasound examination of multiple ovarian cysts which represent immature follicles. The follicles have developed from primordial follicles but the development has stopped at an early antral stage due to the disturbed ovarian function. The follicles may be oriented along the ovarian periphery appearing as a ‘string of pearls’ on ultrasound examination [11].
Patients with PCOS have higher gonadotrophin releasing hormone (GnRH), which in turn results in an increase in LH/FSH ratio in females with PCOS. The majority of patients with PCOS have insulin resistance and/or obesity. Their elevated insulin levels contribute to or cause the abnormalities seen in the hypothalamic-pituitary-ovarian axis that lead to PCOS. Hyperinsulinemia increases GnRH pulse frequency, LH over FSH dominance, increased ovarian androgen production, decreased follicular maturation and decreased SHBG binding. All these factors contribute to the development of PCOS [2,12].
PCOS is characterized by a complex positive feedback of insulin resistance and hyperandrogenism. In most cases, it can not be determined which of those two should be regarded to be the causative agent. Experimental treatment with either anti-androgens or insulin sensitizing agents improves both hyperandrogenism and insulin resistance [13].
Adipose tissue possesses aromatase, an enzyme that converts androstenedione to estrone and testosterone to estradiol. The excess of adipose tissue in obese patients causes them to have both excess androgens (which are responsible for hirsutism and virilization) and estrogens (which inhibit FSH via negative feedback) [14].
PCOS may be associated with chronic inflammation of the ovary which may induce conformational, endocrinal and metabolic changes which may predispose to PCOS. Several studies correlate the inflammatory mediators and oxidative stress with anovulation and other PCOS symptoms [15].
It was previously suggested that the excessive androgen production in PCOS could be caused by a decreased serum level of insulin-like growth factor binding protein-1 (IGFBP-1), in turn increasing the level of free IGF-1 which stimulates ovarian androgen production, but recent data concludes this mechanism to be unlikely. PCOS has also been associated with a specific fragile X mental retardation 1 (FMR1) sub-genotype. Many studies suggested that women who have heterozygous-normal/ low FMR1 have polycystic-like symptoms of excessive follicle-activity and hyperactive ovarian function [16,17].
Clinical manifestations of PCOS
The most common symptoms of PCOS include menstrual disorders such as oligomenorrhea or amenorrhea, infertility, high levels of masculinizing hormones manifested by acne and hirsutism and metabolic syndrome which appears as a tendency towards central obesity and other symptoms associated with insulin resistance. Serum insulin, insulin resistance and homocysteine levels are higher in females with PCOS than in the normal females [2,13].
Diagnosis of PCOS
Not all women with PCOS have polycystic ovaries, nor do all women with ovarian cysts have PCOS. Although pelvic ultrasound is a major diagnostic tool, it is not the only one. Many definitions are used for diagnosis of PCOS such as National Institutes of Health (NIH) criteria, Rotterdam criteria and Androgen Excess PCOS Society criteria [18].
NIH criteria: In 1990, a workshop sponsored by the NIH suggested that a patient has PCOS if she has oligoovulation, signs of androgen excess (clinical or biochemical) and other entities are excluded that would cause polycystic ovaries [19].
Rotterdam criteria: In 2003, a consensus workshop held in Rotterdam indicated PCOS to be present if any 2 out of 3 criteria are met including oligoovulation and/or anovulation, excess androgen activity and polycystic ovaries (By gynecologic ultrasound) [20].
The Rotterdam definition is wider, including many more patients, most notably patients without androgen excess. Critics say that findings obtained from the study of patients with androgen excess cannot necessarily be extrapolated to patients without androgen excess [21].
Androgen excess PCOS Society criteria: In 2006, the Androgen Excess PCOS Society suggested a tightening of the diagnostic criteria to all of the following including excess androgen activity, oligoovulation/anovulation, polycystic ovaries and other entities are excluded that would cause excess androgen activity [5].
Standard diagnostic assessment
History-taking
Specifically for menstrual pattern, obesity, hirsutism and the absence of breast development. If obese, the time of onset, progression and problems should be explored. Lifestyle parameters such as diet, exercise and smoking need evaluation, as do the age of onset and progression of hirsutism and/or acne. Any medications used and their effects on acne and hirsutism should also be considered. Family history should explore infertility, menstrual disorders, age of puberty and hirsutism in female relatives [22].
Physical examination
This includes general body habitus, obesity, body mass index, blood pressure, presence of acne, male pattern of baldness and evidence of acanthosis nigricans. The severity and distribution of hirsutism should be graded clinically. Girls with PCOS with marked hyperandrogenism such as clitoromegaly, deepening of the voice or a masculine body habitus should alert one to the possibility of virilizing adrenal/ovarian tumours or congenital adrenal hyperplasia [23].
Gynecologic ultrasonography
It looks for small ovarian follicles. According to the Rotterdam criteria, 12 or more small follicles should be seen in an ovary on ultrasound examination. The numerous follicles contribute to the increased size of the ovaries that is 1.5 to 3 times larger than normal [20].
Laboratory tests
Serum levels of androgens, including androstenedione and testosterone may be elevated. Dehydroepiandrosterone sulfate (DHEA-S) levels above 700-800 mcg/dL are highly suggestive of adrenal dysfunction. The free testosterone level is thought to be the best measure, with about 60% of PCOS patients demonstrating high levels [13].
1. The ratio of LH (Luteinizing hormone) to FSH (Follicle stimulating hormone) is greater than 1:1 (sometimes more than 3:1), as tested on day 3 of the menstrual cycle [12].
2. Fasting biochemical screen and lipid profile.
3. Two-hours oral glucose tolerance test (GTT) in patients with risk factors (Obesity, family history, history of gestational diabetes) may indicate impaired glucose tolerance (insulin resistance) in patients with PCOS [5].
4. Fasting insulin level or GTT with insulin levels (also called IGTT): Elevated insulin levels have been helpful to predict response to medication and may indicate patients who will need higher doses of metformin or the use of a second medication to lower insulin levels. A hypoglycemic response in which the twohour insulin level is higher and the blood sugar lower than fasting is consistent with insulin resistance. A mathematical derivation known as the HOMAI, calculated from the fasting values in glucose and insulin concentrations, allows a direct and moderately accurate measure of insulin sensitivity (glucoselevel x insulin-level/22.5) [18].
Differential diagnosis of PCOS
Other causes of irregular or absent menstruation and hirsutism, such as hypothyroidism, congenital adrenal hyperplasia (21-hydroxylase deficiency), Cushing’s syndrome, hyperprolactinemia, androgen secreting neoplasms and other pituitary or adrenal disorders should be investigated. PCOS has been reported in other insulin-resistant situations such as acromegaly [5].
Management of PCOS
Medical treatment of PCOS aims to lowering insulin levels, restore fertility, treat hirsutism or acne, restore regular menstruation and prevent endometrial hyperplasia and endometrial cancer. General interventions that help to reduce weight or insulin resistance can be beneficial for all these aims because they are believed to be the underlying causes [5].
Diet regulation
Where PCOS is associated with overweight or obesity, successful weight reduction is the most effective method of restoring normal ovulation and menstruation. Low-carbohydrate diet and sustained regular exercise may help. It has been recommended that a diet in which a significant part of total carbohydrates is obtained from fruit, vegetables and whole grain sources may be helpful. Vitamin D deficiency may play a role in the development of the metabolic syndrome because vitamin D is essential for formation of the hormones of the adrenal cortex. So, treatment of vitamin D deficiency is indicated in the management of PCOS [24].
Medications
Reducing insulin resistance by improving insulin sensitivity through medications such as metformin and thiazolidinedione have been an obvious approach and initial studies seemed to show effectiveness. The United Kingdom’s National Institute for Health and Clinical Excellence recommended in 2004 that women with PCOS and a body mass index above 25 be given metformin when other therapy has failed to produce results [25].
Infertility
Not all women with PCOS have difficulty becoming pregnant. For those who do, anovulation or infrequent ovulation is a common cause. Other factors include changed levels of gonadotropins, hyperandrogenemia and hyperinsulinemia. For overweight anovulatory women with PCOS, weight loss and diet adjustments, especially to reduce the intake of simple carbohydrates, are associated with resumption of the normal ovulation [26].
For those who after weight loss still are anovulatory or for anovulatory lean women, the ovulation inducing medications such as clomiphene citrate and FSH are the principal treatments used to promote ovulation. Previously, the anti-diabetes medication metformin was the recommended treatment for anovulation, but it appears less effective than clomiphene. Assisted reproductive technology procedures such as controlled ovarian hyper-stimulation with FSH injections followed by in vitro fertilization are used for patients who do not respond to clomiphene, diet and lifestyle modification [27].
Though surgery is not commonly performed, the polycystic ovaries can be treated with a laparoscopic procedure called ovarian drilling, which often results in either resumption of spontaneous ovulations or ovulations after adjuvant treatment with clomiphene or FSH. However, there are concerns about the long-term effects of ovarian drilling on ovarian function [28].
Hirsutism and acne
Contraceptive pills are frequently effective in reducing hirsutism. A common choice of contraceptive pill is one that contains cyproterone acetate which is a progestogen with anti-androgen effects that blocks the action of male hormones that are believed to contribute to acne and the growth of unwanted facial and body hair. On the other hand, progestogens such as norgestrel and levonorgestrel should be avoided due to their androgenic effects [29].
Other drugs with anti-androgen effects include flutamide and spironolactone which can give some improvement in hirsutism. Metformin can reduce hirsutism, perhaps by reducing insulin resistance, and is often used if there are other features such as insulin resistance, diabetes or obesity that can also benefit from metformin. Eflornithine is a drug which is applied to the skin in cream form and acts directly on the hair follicles to inhibit hair growth. It is usually applied to the face. Medications that reduce acne by indirect hormonal effects also include ergot dopamine agonists such as bromocriptine [30]. 5-alpha reductase inhibitors (such as finasteride and dutasteride) may also be used. They act by blocking the conversion of testosterone to dihydrotestosterone (the latter of which is responsible for most hair growth alterations and androgenic acne) [31].
Although these agents have shown significant efficacy in clinical trials, the reduction in hair growth may not be enough to eliminate the social embarrassment of hirsutism or the inconvenience of shaving. Individuals vary in their response to different therapies and drug treatments do not work well for all individuals. For removal of facial hairs, electrolysis or laser treatments are faster and more efficient alternatives than the above mentioned drugs [32].
Menstrual irregularity and endometrial hyperplasia
If fertility is not the primary aim, then menstruation can usually be regulated with contraceptive pills. The purpose of regulating menstruation is essentially for the woman’s convenience and perhaps her sense of well-being. There is no medical requirement for regular periods, so long as they occur sufficiently often [29].
If a regular menstrual cycle is not desired, then therapy for an irregular cycle is not necessarily required. If menstruation occurs less often or not at all, some form of progestogen replacement is recommended. Some women prefer a uterine progestogen device such as the intrauterine system or the progestin implant, which provides simultaneous contraception and endometrial protection for years. An alternative is oral progestogen taken at intervals (e.g., every three months) to induce a predictable menstrual bleeding [19].
Alternative medicine
Acupuncture is one of the alternative medicine modalities that had been emerging as one of the commonly used methods for treatment of PCOS. Acupuncture may help PCOS patients to regulate and manage their periods. Moreover, it may help in decreasing body weight, reducing headache and improving patients’ mood. Also, placing acupuncture needles in the areas related to the reproductive system may improve blood supply to the reproductive area, normalize hormone levels and help the proper functioning of the reproductive system [33,34].
There is insufficient evidence to conclude an effect from D-chiro-inositol in PCOS. However, myo-inosiol appears to be effective. It is capable of restoring spontaneous ovarian activity and consequently fertility in most patients with PCOS [35].
Prognosis of PCOS
Women with PCOS are at risk for endometrial hyperplasia and endometrial cancer, insulin resistance and type II diabetes, hypertension, depression, psychological disorders, dyslipidemia, cardiovascular diseases, cerebrovascular stroke, weight gain, sleep apnea, non-alcoholic fatty liver disease, acanthosis nigricans (patches of darkened skin under the arms, in the groin, on the back of the neck) and autoimmune thyroiditis. Early diagnosis and treatment may reduce the risk of these complications, such as type 2 diabetes and heart disease [36].
Conclusion
PCOS is one of the most important endocrine disorders that affects females in the reproductive age and may lead to serious complications. Further studies are needed to determine the exact etiology of PCOS, methods of prevention and proper management.
References
- El-Sharkawy AA, Abdelmotaleb GS, Aly MK, Kabel AM. Effect of metformin on sleep disorders in adolescent girls with polycystic ovarian syndrome. J. Pediatr. Adolesc. Gynecol. 27(6), 347-352 (2014).
- Nafiye Y, Sevtap K, Muammer D, et al. The effect of serum and intrafollicular insulin resistance parameters and homocysteine levels of nonobese, nonhyperandrogenemic polycystic ovary syndrome patients on in vitro fertilization outcome. Fertil. Steril. 93(6), 1864-1869 (2010).
- Allahbadia GN, Merchant R. Polycystic ovary syndrome and impact on health. Middle. East. Fertil. Soc. J. 16(1), 19-37 (2011).
- Boomsma CM, Fauser BC, Macklon NS. Pregnancy complications in women with polycystic ovary syndrome. Semin. Reprod. Med. 26(1), 72-84 (2008).
- Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 8, 41 (2010).
- Palomba S, Santagni S, Falbo A, La Sala GB. Complications and challenges associated with polycystic ovary syndrome: current perspectives. Int. J. Womens Health. 7, 745-763 (2015).
- Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380(9859), 2163-2196 (2012).
- Hernandez MI, Mericq V. Polycystic ovarian syndrome. In: Brook C, Clayton P, Brown R, eds. Brook’s clinical paediatric endocrinology. Blackwell. pp: 559-570 (2015).
- Strauss JF. Some new thoughts on the pathophysiology and genetics of polycystic ovary syndrome. Ann. N Y Acad. Sci. 997, 42-48 (2003).
- Amato P, Simpson JL. The genetics of polycystic ovary syndrome. Best. Pract. Res. Clin. Obstet. Gynaecol. 18(5), 707-718 (2004).
- Lee TT, Rausch ME. Polycystic ovarian syndrome: role of imaging in diagnosis. Radiographics. 32(6), 1643-1657 (2012).
- Sharquie KE, Al-Bayatti AA, Al-Ajeel AI, Al-Bahar AJ, Al-Nuaimy AA. Free testosterone, luteinizing hormone/follicle stimulating hormone ratio and pelvic sonography in relation to skin manifestations in patients with polycystic ovary syndrome. Saudi Med. J. 28(7), 1039-1043 (2007).
- Pasquali R, Gambineri A. Insulin-sensitizing agents in polycystic ovary syndrome. Eur. J. Endocrinol. 154(6), 763-775 (2006).
- Sathyapalan T, Atkin SL. Mediators of inflammation in polycystic ovary syndrome in relation to adiposity. Mediators Inflamm. 758656 (2010).
- González F, Rote NS, Minium J, Kirwan JP. Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome. J. Clin. Endocrinol. Meta. 91(1), 336-340 (2006).
- Gleicher N, Weghofer A, Lee IH, Barad DH. FMR1 genotype with autoimmunity-associated polycystic ovary-like phenotype and decreased pregnancy chance. PLoS ONE. 5(12), e15303 (2010).
- Kelly CJ, Stenton SR, Lashen H. Insulin-like growth factor binding protein-1 in PCOS: a systematic review and meta-analysis. Hum. Reprod. Update. 17(1), 4-16 (2011).
- Broder-Fingert S, Shah B, Kessler M, Pawelczak M, David R. Evaluation of adolescents for polycystic ovary syndrome in an urban population. J. Clin. Res. Pediatr. Endocrinol. 1(4), 188-193 (2009).
- Carmina E. PCOS: metabolic impact and long-term management. Minerva Ginecol. 64(6), 501-505 (2012).
- Azziz R. Controversy in clinical endocrinology: diagnosis of polycystic ovarian syndrome: the Rotterdam criteria are premature. J. Clin. Endocrinol. Metab. 9(3), 781-785 (2006).
- Hart R, Hickey M, Franks S. Definitions, prevalence and symptoms of polycystic ovaries and polycystic ovary syndrome. Best Pract. Res. Clin. Obstet. Gynaecol. 18(5), 671-683 (2004).
- Diamanti-Kandarakis E. PCOS in adolescents. Best Pract Res Clin Obstet Gynaeco.l 24(2), 173-183 (2010).
- Tharian K, Warner J. Polycystic ovarian syndrome in adolescent girls. Paediatr. Child. Health. 21(7), 309-314 (2011).
- Marsh K, Brand-Miller J. The optimal diet for women with polycystic ovary syndrome. Br. J. Nutr. 94(2), 154-165 (2005).
- Leeman L, Acharya U. The use of metformin in the management of polycystic ovary syndrome and associated anovulatory infertility: the current evidence. J. Obstet. Gynaecol. 29(6), 467-472 (2009).
- Qiao J, Feng HL. Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence. Hum. Reprod. Update. 2010; 17 (1): 17
- Legro RS, Barnhart HX, Schlaff WD, et al. Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome. N. Engl. J. Med. 356(6), 551-566 (2007).
- Farquhar C, Brown J, Marjoribanks J. Laparoscopic drilling by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane. Database. Syst. Rev. 6(6), CD001122 (2012).
- Bhattacharya SM, Jha A. Comparative study of the therapeutic effects of oral contraceptive pills containing desogestrel, cyproterone acetate, and drospirenone in patients with polycystic ovary syndrome. Fertil. Steril. 98 (4), 1053-1059 (2012).
- Lumachi F, Basso SM. Medical treatment of hirsutism in women. Curr. Med. Chem. 17(23), 2530-2538 (2010).
- Farshi S, Mansouri P, Rafie F. A randomized double blind, vehicle controlled bilateral comparison study of the efficacy and safety of finasteride 0.5% solution in combination with intense pulsed light in the treatment of facial hirsutism. J. Cosmet. Laser. Ther. 14(4), 193-199 (2012).
- Schumacher B. Cosmetic therapy of hirsutism. With laser and electric current against a hairy problem. MMW. Fortschr. Med. 153(46), 14-16 (2011).
- Badawy A, Elnashar A. Treatment options for polycystic ovary syndrome. Int. J. Womens. Health. 3(3), 25-35 (2011).
- Lim CE, Wong WS. Current evidence of acupuncture on polycystic ovarian syndrome. Gynecol. Endocrinol. 26(6), 473-478 (2011).
- Unfer V, Carlomagno G, Dante G, Facchinetti F. Effects of myo-inositol in women with PCOS: a systematic review of randomized controlled trials. Gynecol. Endocrinol. 28(7), 509-515 (2012).
- Ong KJ, Theodoru E, Ledger W. Long-term consequence of polycystic ovarian syndrome. Curr. Obste. Gynaecol. 16, 333-336 (2006).