Review Article - Interventional Cardiology (2021)
Prediction and assessment of the long-term outcomes of coronary chronic total occlusion-percutaneous coronary intervention
- Corresponding Author:
- Soichiro Ebisawa
Department of Cardiovascular Medicine,
Shinshu University School of Medicine,
Matsumoto,
Japan,
E-mail: ebifender@yahoo.co.jp
Received date: June 25, 2021 Accepted date: July 09, 2021 Published date: July 16, 2021
Abstract
Coronary Chronic Total Occlusions (CTOs) are completely occluded coronary arteries that have no antegrade coronary flow for an estimated duration of at least 3 months. Although Percutaneous Coronary Intervention (PCI) for CTO lesions (CTO-PCI) has a lower success rate and a higher complication rate than PCI for nonocclusive lesions, owing to recent improvements in devices and strategies, CTO-PCI may be a valid strategy for patients with ischemic heart disease. The clinical benefits of CTO-PCI have remained ambiguous because most investigations on CTO-PCI are non-randomized observational trials that compared successful and unsuccessful cases of CTO-PCI. Recent randomized controlled trials that compared CTO-PCI and optimal medical therapy or the non-use of CTO-PCI failed to reveal the clinical benefits of CTO-PCI. Although the initial success rate of CTO-PCI was improved, no obvious indication for CTO-PCI was established, except for the relief of symptoms and the improvement of quality of life. However, there are cases in which CTO-PCI provides significant benefits in daily practice.
The following actions are required to establish the validity of CTO-PCI:
1) Determining indications for which CTO-PCI would result in the most favorable outcomes and
2) Developing standardized pre-procedural risk assessment tools that can assist the identification of patients who are at a high risk of developing long-term clinical events.
Keywords
Chronic total occlusion • Percutaneous coronary intervention • Longterm outcome • Coronary artery disease
Abbreviations
AUC: Area Under the Curve; CAD: Coronary Artery Disease; CABG: Coronary Artery Bypass Grafting; CI: Confidence Interval; CTO: Chronic Total Occlusion; ICD: Implantable Cardioverter-Defibrillator; LV: Left Ventricle; LVEF: Left Ventricular Ejection Fraction; MACCEs: Major Adverse Cardiac And Cerebrovascular Events; MI: Myocardial Infarction; OR: Odds Ratio; OMT: Optimal Medical Therapy; PCI: Percutaneous Coronary Intervention; QOL: Quality of life; RCTs: Randomized Clinical Trials; ROC: Receiver Operator Characteristic
Introduction
Percutaneous Coronary Intervention (PCI) is a valid treatment option for patients with Chronic Total Occlusion (CTO). However, post-PCI patient outcomes vary significantly among medical centers. Additionally, the optimal treatment strategies remain controversial, despite technological and methodological advancements [1-4] in medicine. Moreover, the high incidence of long-term Major Adverse Cardiac and Cerebrovascular Events (MACCEs) remains unresolved. Under the current treatment protocols, over 20.7% of post-CTO-PCI patients experience restenosis within 5 years of the procedure, which is considerably higher than the restenosis rate in non-CTO-PCI patients [5]. Conversely, the long-term outcome of Coronary Artery Bypass Grafting (CABG) for CTO is favorable, with the achievement of over 90% patency of the left internal mammary artery [6]. In current guidelines and the global consensus concerning CTO-PCI, the recommendation level is limited [7-9].
The CTO-PCI procedure is generally complex [10-13], requiring high volumes of contrast media and radiation [14,15]. The effectiveness of CTO-PCI is limited to the relief of angina symptoms and Quality Of Life (QOL) improvement, while the long-term clinical outcomes have not been established in Randomized Controlled Trials (RCTs). CTO-PCI is the most difficult aspect of the treatment strategy for Coronary Artery Disease (CAD), and it is laborious and is associated with the risk of severe complications. The inclusion of CTO-PCI in the current treatment strategy for CAD necessitates determining when CTO-PCI would be beneficial for patients with CAD, along with the pre-procedural prediction of long-term mortality to ensure favorable long-term outcomes.
Literature Review
Clinical benefits of CTO-PCI
• From observational trials: Historically, the clinical benefits of CTO-PCI have been assessed using registry data and nonrandomized observational studies [16-19]. Several clinical benefits of CTO-PCI were observed in these studies.
A meta-analysis including 25 studies with 28,486 patients (29,315 CTO-PCI procedures) revealed that a successful CTO-PCI was a significant predictor of all-cause mortality (Odds Ratio (OR) 0.52; 95% Confidence Interval (CI), 0.43–0.63). It was also observed that angina symptoms were improved in the CTO-PCI success group compared with those in the CTO-PCI failure group (OR=0.38; 95% CI, 0.24-0.60) [20].
Jones, et al. [21] and George, et al. [22] reported that successful CTO-PCI, compared to unsuccessful CTO-PCI, improved longterm survival. Mehran, et al. also demonstrated that successful CTO-PCI decreased the need for CABG (hazard ratio, 0.21; 95% CI, 0.13–0.40; p<0.01) [23].
CTO-PCI is also expected to improve Left Ventricular (LV) contraction. Galassi, et al. investigated the effects of CTO-PCI for the improvement of low LV function in a prospective longitudinal multicenter study of consecutive patients. The authors divided 839 patients into three groups based on their pre-procedural Left Ventricular Ejection Fraction (LVEF) (≤ 35%, 35%-50%, and ≤ 50%). The success rate of CTO-PCI did not differ between the three groups (93.5% vs. 94.4% vs. 91.7%, respectively; p-values were not significant). In patients with LVEF ≤ 35%, LVEF improved significantly, that is, from 29.1% ± 3.4% to 41.6% ± 7.9% (p<0.001), when CTO-PCI was performed successfully [24].
The OPEN-CTO (Outcomes, Patient Health Status, and Efficiency in Chronic Total Occlusion Hybrid Procedures) study was designed to address the methodological limitations of prior studies on CTO-PCI, including efforts to ensure consecutive enrollment, complete and systematic reporting of adverse events, and comprehensive health status assessments before and after CTO-PCI. The technical success was high (86%). In-hospital and 1-month mortalities were 0.9% and 1.3%, respectively. Notably, among patients who survived and completed the 1-month interview, Seattle Angina Questionnaire QOL scores improved from 49.4 ± 0.9 to 75.0 ± 0.7 (p<0.01), mean Rose Dyspnea Scale scores improved (decreased) from 2.0 ± 0.1 to 1.1 ± 0.1 (p<0.01), and physician health questionnaire (for depression) scores improved (decreased) from 6.2 ± 0.2 to 3.5 ± 0.1 (p<0.01) at 1 month [12].
• From randomized controlled trials: The majority of nonrandomized studies on the clinical benefits of CTO-PCI compared the outcomes of patients who underwent successful CTO-PCI with those of patients who underwent unsuccessful CTO-PCI, including bias such as the assumption that patients who have more complex background clinical features are more likely to have unsuccessful CTO-PCI. Furthermore, undergoing an attempt that expected to fail, at PCI for a CTO could be potentially harmful because the CTO-PCI is a high-risk procedure that includes the risk of complications associated with the collateral donor artery, along with cardiac tamponade caused by vessel perforation. Therefore, because non-randomized trials for CTO-PCI may include certain biases, the results of these trials may not be considered absolute evidence. In recent years, RCTs on CTO-PCI have been performed worldwide [25,26].
The Randomized Multicentre Trial to Evaluate the Utilization of Revascularization or Optimal Medical Therapy for the Treatment of Chronic Total Coronary Occlusions was a prospective RCT that included 396 patients who were divided into two groups: A group that received CTO-PCI plus Optimal Medical Therapy (OMT) and a group that received OMT alone (in a ratio of 2:1). This trial was performed in 28 European centers [27]. The primary endpoint of the trial was change in health status at 12 months, which was assessed using the Seattle Angina Questionnaire. Of 259 patients randomized to the CTO-PCI group, the procedural success rate was 86.6%. At 12 months, in the intention-to-treat analysis, greater improvement in the Seattle Angina Questionnaire subscales was observed in patients who underwent PCI compared to those who received OMT. Importantly, the PCI group showed lower angina frequency, higher rates of freedom from angina, and higher QOL scores, suggesting a role of CTO-PCI with respect to both relief of symptoms and improve QOL. However, the patients and clinicians were not blinded to the treatment type, which may have influenced the effect of the treatment. Although the sample size was relatively small for a comparison of clinical events, the incidence of ischemia-driven PCI was significantly lower in the CTO-PCI group (2.9% vs. 6.7%, p<0.05). There were no statistical differences in the incidence of clinical events, such as death, Myocardial Infarction (MI), or re-hospitalization.
The drug-eluting stent implantation versus optimal medical treatment in patients with chronic total occlusion trial was also a prospective, open-label RCT that compared CTO-PCI with OMT (in a 1:1 fashion), based on clinical endpoints [28]. This trial was a non-inferiority study that hypothesized that the efficacy of treatment without CTO-PCI is not inferior to that with CTO-PCI. The inclusion criteria were individuals with stable angina, acute coronary syndrome, and silent ischemia, and the primary endpoints were all-cause mortality, MI, stroke, or repeat revascularization. However, due to a slow recruitment, the study was terminated before the completion of its 1284 planned enrollments; finally, 834 patients were included in the study. The overall success rate of CTO-PCI was 90.6%. In the intention-totreat analysis, the primary endpoint was not statistically significant between the two groups at 3 years (PCI vs. OMT: 20.6% vs. 19.6%, p=0.5). The two groups demonstrated a similar degree of improvement in QOL, which was sustained for 30 months. Therefore, this study showed no evident clinical benefits of CTOPCI, and no difference in QOL scores was observed between the groups. However, there was significant crossover within the groups (18.1% of individuals in the OMT group underwent PCI, while 15.6% of individuals in the PCI group received OMT alone). The early termination of enrollment due to the slow enrollment might have resulted in an underpowered study. Furthermore, many patients in this study had multivessel diseases at the time of enrollment, and several patients in both groups underwent revascularization of non-CTO lesions, which might have affected the results of clinical events and symptoms.
In brief, these two well-conducted RCTs demonstrated similar negative results regarding long-term clinical event rates associated with CTO-PCI, although they had several limitations. Although an appropriately powered study is required to validate the outcomes of these studies, to make CTO-PCI a more effective treatment option for patients with CAD, the results of these studies are noteworthy and the indication for CTO-PCI should be reconsidered.
• Prediction of initial success: The CTO-PCI procedure is generally complex [12] and requires a high volume of contrast media and radiation during the procedure [14,15]. The worldwide success rate of CTO-PCI is low. A meta-analysis that included 61 studies identified strong negative predictors of the clinical success of CTO-PCI [29]. Furthermore, several risk models for the prediction of initial procedural success have been developed [30-32].
The Multicenter CTO Registry in Japan (J-CTO) score was established in 2011, and this score predicted the probability of successful guidewire crossing within 30 min [30]. The variables included in the J-CTO score were calcification, bending, blunt stump, occlusion length >20 mm, and lesions with previous failure. The performance of this scoring model was assessed by Receiver Operator Characteristic (ROC) analysis (Area Under the Curve [AUC], 0.82; validation cohort, 0.76).
The Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS-CTO) [31] score was developed based on 781 CTO-PCIs in seven U.S. centers with significant expertise in CTO-PCI, using variables such as no interventional collaterals, proximal cap ambiguity, moderate or severe tortuosity, and left circumflex CTO. The resulting score demonstrated good calibration and discriminatory capacity in the derivation (Hosmer-Lemeshow chi-square=2.633; p=0.268, and ROC area=0.778) and validation (Hosmer-Lemeshow chisquare= 5.333; p=0.070, and ROC area=0.720) subsets.
The clinical and lesion-related score (CL score) was established to predict the final procedural success of CTO-PCI and was based on the prospectively collected data of 1,657 consecutive patients who underwent a first-attempt CTO-PCI [32]. Independent predictors of unsuccessful CTO-PCI were scored according to the corresponding OR size. The scores were as follows: Severe calcification=2, previous CABG=1.5, lesion length ≥ 20 mm=1.5, previous MI=1, blunt stump=1, and non-left anterior descending artery CTO location=1.
The performance of both the PROGRESS-CTO and CL-scores was compared with that of the J-CTO score in each cohort, and the performance of both scores was similar to that of the J-CTO score.
The Euro-CTO (CASTLE) score is the most recent scoring model developed using a prospective database. This score was established in 2008 and it was formulated based on >20,000 cases submitted by CTO expert operators (>50 cases/year) [33]. The variables of this scoring system were CABG history, age (≥ 70 years), stump anatomy (blunt or invisible), degree of tortuosity (severe or unseen), length of occlusion (≥ 20 mm), and extent of calcification (severe). When each parameter was assigned a value of 1, the technical failure increased from 8% (with a CASTLE score of 0 to 1) to 35% (with a score ≥ 4). The AUC was similar for both the derivation (AUC: 0.66) and validation (AUC: 0.68) datasets. The strength of this model is its development from the largest database of CTO cases to date. These scoring systems are well established and are used in daily clinical practice.
Discussion
Assessment and prediction of long-term outcome
As mentioned above, many risk models for assessing the initial success of CTO-PCI have been established. However, these models do not effectively predict long-term outcomes following the procedure. Forouzandeh, et al. revealed the effects of the J-CTO and PROGRESS scores for the prediction of chronic events after CTO-PCI; however, the study populations were small and the procedural success rates were lower than those in conventional CTO studies [34].
The biggest problem with CTO-PCI is the lack of evidence for its long-term clinical benefits, which may not exceed the procedural difficulty.
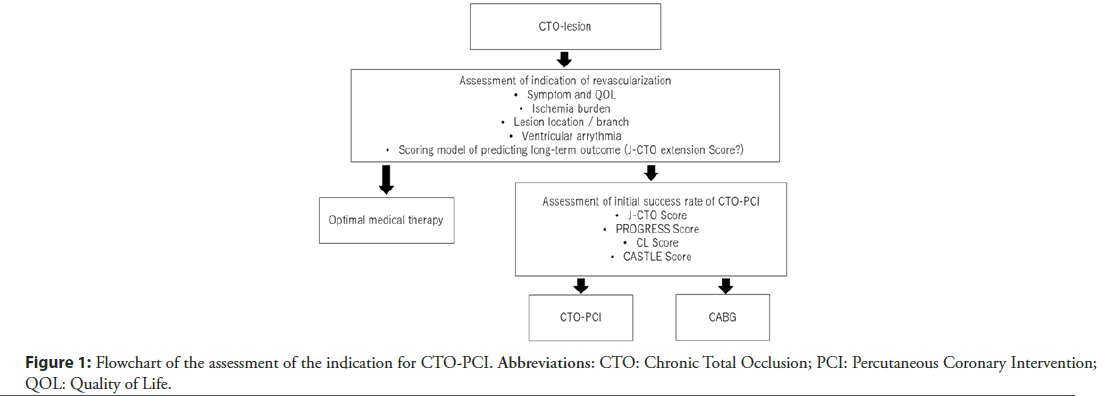
The establishment of CTO-PCI requires two actions: Determining indications for which CTO-PCI would result in the most favorable outcomes and the development of standardized pre-procedural risk assessment tools to assist the identification of patients who are at a high risk of developing long-term clinical events (Figure 1).
The ventricular arrhythmias among implantable cardioverterdefibrillator recipients for primary prevention study is an observational study that compared the occurrence of appropriate Implantable Cardioverter-Defibrillator (ICD) delivery for ventricular arrhythmias in patients with and without CTO [35]. A total of 162 CAD patients with an ICD were included in the study and were followed up for a median of 26 months. Of the 162 patients, there was at least one case of CTO in 71 patients (44%). Appropriate device therapy was detected in 18% of patients during follow-up. The presence of CTO was associated with higher ventricular arrhythmia and mortality rates (log-rank test, p<0.01). Multivariate analysis revealed that CTO was independently associated with appropriate ICD interventions.
Safley, et al. revealed that the threshold of baseline ischemic burden was 12.5% in 301 patients who underwent CTO-PCI at a single center between 2002 and 2007. Patients were included in this study if myocardial perfusion imaging was performed within 12 ± 3 months before PCI and a follow-up study was conducted within 12 ± 3 months after PCI [36]. These findings suggested a potential benefit of CTO-PCI or a limited indication of CTO-PCI, i.e., it contributed to the long-term clinical outcomes of the patients. However, to clarify and establish the indications for CTO-PCI, a well-established RCT including a population that is expected to have a favorable clinical benefit is essential.
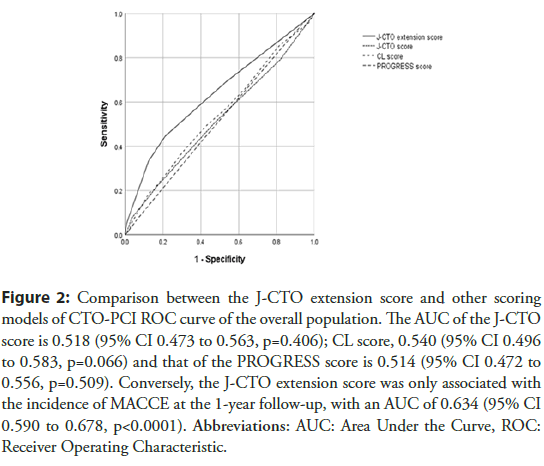
The J-CTO extension score was developed as a prediction model for long-term risk after PCI for coronary CTO, based on preprocedural clinical information, to predict the chronic outcomes of CTO-PCI [37]. The score comprises a hemodialysis score of 3, an in-stent occlusion score of 2, an LVEF<35% score of 2, and a diabetes mellitus score of 1. The J-CTO extension score can predict the incidence of MACCE, including death, stroke, revascularization, and non-fatal MI at the 1-year follow-up. Figure 2 demonstrates an ROC curve analysis for predicting the incidence of 1-year MACCE, along with a comparison among the J-CTO, CL, PROGRESS, and J-CTO extension scores. The AUCs are 0.518 (95% CI of 0.473-0.563, p=0.406), 0.540 (95% CI of 0.496-0.583, p=0.066), and 0.514 (95% CI of 0.472- 0.556, p=0.509) for the J-CTO, CL, and PROGRESS scores, respectively. The J-CTO extension score was the only score that was associated with the incidence of MACCE, with an AUC of 0.634 (95% CI, 0.590-0.678; p <0.0001). However, this model has limitations such as a low follow-up rate (approximately 45%) and the potential to miss hard endpoints (e.g., all-cause death and non-fatal MI and stroke) that might affect the results. However, pre-procedural prediction of long-term outcome is important to assess the indications of CTO-PCI, and further analysis is required in populations with a high follow-up rate.
Figure 2: Comparison between the J-CTO extension score and other scoring models of CTO-PCI ROC curve of the overall population. The AUC of the J-CTO score is 0.518 (95% CI 0.473 to 0.563, p=0.406); CL score, 0.540 (95% CI 0.496 to 0.583, p=0.066) and that of the PROGRESS score is 0.514 (95% CI 0.472 to 0.556, p=0.509). Conversely, the J-CTO extension score was only associated with the incidence of MACCE at the 1-year follow-up, with an AUC of 0.634 (95% CI 0.590 to 0.678, p<0.0001). Abbreviations: AUC: Area Under the Curve, ROC: Receiver Operating Characteristic.
Conclusion
Currently, the main benefits of CTO-PCI include the improvement of angina symptoms and QOL. The CTO-PCI procedure is difficult and is associated with the risk of complications; however, risk models for the prediction of initial success have been developed. The long-term outcomes of CTO-PCI need to be assessed, and the specific indications need to be established. Thus, conditions (i.e., ventricular arrhythmia and large ischemic burden) in which CTOPCI may produce maximum clinical benefits should be identified, along with the pre-procedural prediction of long-term outcomes. CTO-PCI should be performed only after careful selection of patients and the pre-procedural prediction of initial and long-term outcomes. CTO-PCI seems to be an effective treatment option for patients with CAD.
Acknowledgements
I am grateful to the members of the cardiac catheterization laboratories of the participating centers and the clinical research coordinators of Retrograde Summit Registry.
Funding
None.
Competing Interests
Soichiro Ebisawa; Affiliation with Endowed Department Medtronic, Abbott Vascular Japan, Boston Scientifics Japan, TERUMO, NIPRO and Cordis.References
- Teeuwen K, van der Schaaf RJ, Adriaenssens T, et al. Randomized multicenter trial investigating angiographic outcomes of hybrid sirolimus-eluting stents with biodegradable polymer compared with everolimus-eluting stents with durable polymer in chronic total occlusions: The Prison IV trial. JACC Cardiovasc Interv. 10(2): 133-43 (2017).
- Prasad A, Rihal CS, Lennon RJ, et al. Trends in outcomes after percutaneous coronary intervention for chronic total occlusions: A 25-year experience from the Mayo Clinic. J Am Coll Cardiol. 49(15): 1611-8 (2007).
- Pershad A, Eddin M, Girotra S, et al. Validation and incremental value of the hybrid algorithm for CTO PCI. Catheter Cardiovasc Interv. 84(4): 654-9 (2014).
- Brilakis ES, Grantham JA, Riefert S, et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 5(4): 367-79 (2012).
- Kato M, Kimura T, Morimoto T, et al. Comparison of five-year outcome of sirolimus-eluting stent implantation for chronic total occlusions versus for non-chronic total occlusion (from the j-Cypher registry). Am J Cardiol. 110 (9): 1282-9 (2012).
- Zakkar M, George SJ, Ascione R. Should chronic total occlusion be treated with coronary artery bypass grafting? Chronic total occlusion should be treated with coronary artery bypass grafting. Circulation. 133 (18): 1807-1 (2016).
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 14 (14): 1435-534 (2019).
- Brilakis ES, Mashayekhi K, Tsuchikane E, et al. Guiding principles for chronic total occlusion percutaneous coronary intervention. Circulation. 140 (5): 420-33 (2019).
- Riley RF, Henry TD, Mahmud E, et al. SCAI position statement on optimal percutaneous coronary interventional therapy for complex coronary artery disease. Catheter Cardiovasc Interv. 96 (2): 346-62 (2020).
- Maeremans J, Dens J, Bagnall SJC, et al. Recharge investigators. Antegrade dissection and reentry as part of the hybrid chronic total occlusion revascularization strategy: A subanalysis of the RECHARGE registry (registry of CrossBoss and hybrid procedures in France, the Netherlands, Belgium and United Kingdom). Circ Cardiovasc Int. 10(6): e004791 (2017).
- Karatasakis A, Tarar MN, Karmpaliotis D, et al. Guidewire and microcatheter utilization patterns during antegrade wire escalation in chronic total occlusion percutaneous coronary intervention: Insights from a contemporary multicenter registry. Catheter Cardiovasc Interv. 89(4): E90-8 (2017).
- Sapontis J, Salisbury AC, Cohen YRW, et al. Early procedural and health status outcomes after chronic total occlusion angioplasty: A report from the OPEN-CTO registry (outcomes, patient health status, and efficiency in chronic total occlusion hybrid procedures). JACC Cardiovasc Interv. 10(15): 1523-34 (2017).
- Patel Y, Depta JP, DeMartini TJ. Complications of chronic total occlusion percutaneous coronary intervention. Interv Card. 5(5): 567 (2013).
- Christakopoulos GE, Christopoulos G, Karmpaliotis D, et al. Predictors of excess patient radiation exposure during chronic total occlusion coronary intervention: Insights from a contemporary multicentre registry. Can J Cardiol. 33(4): 478-84 (2017).
- Michael TT, Karmpaliotis D, Brilakis ES, et al. Temporal trends of fluoroscopy time and contrast utilization in coronary chronic total occlusion revascularization: Insights from a multicenter United States registry. Catheter Cardiovasc Interv. 85(3): 393-9 (2015).
- Teramoto T, Tsuchikane E, Yamamoto M, et al. Successful revascularization improves long-term clinical outcome in patients with chronic coronary total occlusion. Int J Cardiol Heart Vasc. 14: 28-32 (2017).
- Sanguineti F, Garot P, O’Connor S, et al. Chronic total coronary occlusion treated by percutaneous coronary intervention: Long-term outcome in patients with and without diabetes. EuroIntervention. 12(15): e1889-97 (2017).
- Kandzari DE, Kini AS, Karmpaliotis D, et al. Safety and effectiveness of everolimus-eluting stents in chronic total coronary occlusion revascularization: Results from the EXPERT CTO multicenter trial (evaluation of the XIENCE coronary stent, performance, and technique in chronic total occlusions). JACC Cardiovasc Interv. 8(6): 761-9 (2015).
- Gong X, Zhou L, Ding X. et al. The impact of successful chronic total occlusion percutaneous coronary intervention on long-term clinical outcomes in real world. BMC Cardiovasc Disord. 21(1): 182 (2021).
- Christakopoulos GE, Christopoulos G, Carlino M, et al. Meta-analysis of clinical outcomes of patients who underwent percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 115(10): 1367-75 (2015).
- Jones DA, Weerackody R, Rathod K, et al. Successful recanalization of chronic total occlusions is associated with improved long-term survival. JACC Cardiovasc Interv. 5(4): 380-8 (2012).
- George S, Cockburn J, Clayton TC, et al. Long-term follow-up of elective chronic total coronary occlusion angioplasty: Analysis from the U.K. Central Cardiac Audit Database. J Am Coll Cardiol. 64(3): 235-43 (2014).
- Mehran R, Claessen BE, Godino C, et al. Multinational chronic total occlusion registry. Long-term outcome of percutaneous coronary intervention for chronic total occlusions. JACC Cardiovasc Interv. 4(9): 952-61 (2011).
- Galassi AR, Boukhris M, Toma A, et al. Percutaneous coronary intervention of chronic total occlusions in patients with low left ventricular ejection fraction. JACC Cardiovasc Interv. 10(2): 2158-70 (2017).
- Morino Y. A contemporary review of clinical significances of percutaneous coronary intervention for chronic total occlusions, with some Japanese insights. Cardiovasc Interv Ther. 36(2): 145-57 (2021).
- Allahwala UK, Ward MR, Brieger D, et al. Indications for percutaneous coronary intervention (PCI) in chronic total occlusion (CTO): Have we reached a DECISION or do we continue to EXPLORE after EURO-CTO? Heart Lung Circ. 28(10): 1484-9 (2019).
- Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions. Eur Heart J. 39(26): 2484-93 (2018).
- Park S-J, editor. DECISION-CTO: Optimal medical therapy with or without stenting for coronary chronic total occlusion. Washington, DC: American College of Cardiology Annual Scientific Session (ACC 2017).
- Wang N, Fulcher J, Abeysuriya N, et al. Predictors of successful chronic total occlusion percutaneous coronary interventions: A systematic review and meta-analysis. Heart 104(6): 517-24 (2018).
- Morino Y, Abe M, Morimoto T, et al. CTO Registry. Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: The J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 4(2): 213-21 (2011).
- Christopoulos G, Kandzari DE, Jaffer YRW, et al. Development and validation of a novel scoring system for predicting technical success of chronic total occlusion percutaneous coronary interventions: The PROGRESS CTO (Prospective Global Registry for the Study of Chronic Total Occlusion Intervention) score. JACC Cardiovasc Interv. 9(1): 1-9 (2016).
- Alessandrino G, Chevalier B, Sanguineti LT, et al. A clinical and angiographic scoring system to predict the probability of successful first-attempt percutaneous coronary intervention in patients with total chronic coronary occlusion. JACC Cardiovasc Interv. 8(12): 1540-8 (2015).
- Szijgyarto Z, Rampat R, Werner GS, et al. Derivation and validation of a chronic total coronary occlusion intervention procedural success score from the 20,000-patient EuroCTO registry: The EuroCTO (CASTLE) score. JACC Cardiovasc Interv. 12: 335-42 (2019).
- Forouzandeh F, Suh J, Stahl E, et al. Performance of J-CTO and PROGRESS CTO scores in predicting angiographic success and long-term outcomes of percutaneous coronary interventions for chronic total occlusions. Am J Cardiol. 121(1): 14-20 (2018).
- Nombela-Franco L, Mitroi CD, Fernández-Lozano I, et al. Ventricular arrhythmias among implantable cardioverter-defibrillator recipients for primary prevention impact of chronic total coronary occlusion (VACTO primary study). Circ Arrhythm Electrophysiol. 5(1): 147-54 (2012).
- Safley DM, Koshy S, Grantham JA, et al. Changes in myocardial ischemic burden following percutaneous coronary intervention of chronic total occlusions. Catheter Cardiovasc Interv. 78(3): 337-43 (2011).
- Ebisawa S, Kohsaka S, Muramatsu T, et al. Derivation and validation of the J-CTO extension score for pre-procedural prediction of major adverse cardiac and cerebrovascular events in patients with chronic total occlusions. PLoS One. 15(9): e0238640 (2020).