Case Series - Clinical Investigation (2022) Volume 12, Issue 6
Presentation of adrenal mass in a tertiary care centre in Kolkata
- Corresponding Author:
- Rahul Roy
Nil Ratan Sircar Medical College and ospital, Kolkata, India
E-mail: rahulroy654@gmail.com
Received: 8-June-2022, Manuscript No. fmci-22-66227; Editor assigned: 9-June-2022, PreQC No. fmci-22-66227 (PQ); Reviewed: 13-June-2022, QC No. fmci-22-66227 (Q); Revised: 17-June-2022, Manuscript No. fmci-22-66227 (R); Published: 24-June-2022; DOI: 10.37532/2041-6792.2022.12(6).119-123
Abstract
This article aims to provide a series of 11 cases of adrenal mass presenting at the Urology department with varied clinical presentations and their management along with their follow-up. Adrenal tumors are not infrequent nowadays. In most of the cases, adrenal incidentaloma is usually an asymptomatic and non-functional adrenal mass which is detected incidentally and does not require any therapeutic intervention. However, conditions like Adrenocortical Carcinoma (ACC), pheochromocytoma, hormone-producing adenoma or metastasis require therapeutic intervention. This study is a retrospective observational analysis of patients presented with adrenal mass in the department of Nil Ratan Sircar Medical College and Hospital (NRSMCH), Kolkata. Out of 11 patients, 6 were male and 5 were female. Thus the Male:Female (M:F) ratio was almost 50:50 in our series. Regarding presentation, 4 patients presented with incidental finding. Another 6 patients presented with abdominal pain. One patient presented with abdominal mass and rest one patient presented with functional features like headache, palpitations and sweating. Among the 11 cases, 8 patients were having myelolipoma (75%), 2 patients were of ACC and 1 patient was having pheochromocytoma.
Keywords
Pheochromocytoma • Adrenal adenoma • Adrenocortical carcinoma • Adrenal tumor
Introduction
Most of the adrenal tumors are discovered incidentally with imaging done due to causes unrelated to the adrenal disorders. In most cases, adrenal incidentalomas are nonfunctioning adrenocortical adenomas [1,2], but may also represent conditions requiring therapeutic intervention (e.g. adrenocortical carcinoma, pheochromocytoma, hormone-producing adenoma or metastasis). Treatment is based on various factors such as, nature of adrenal mass, age of presentation, size of tumor, and the functional status of tumor [3-8]. Adrenocortical tumors can be sporadic or hereditary, with the former representing the overwhelming majority. Close clinical followup, endocrine work-up, and Contrast-Enhanced Computed Tomography (CECT) are helpful in assessing the adrenal mass and optimizing the success of adrenalectomy [1-3]. We here in this brief review will describe a series of 11 cases of adrenal mass presenting at our department with their presentations, management and follow-up.
Materials and Methods
This was a retrospective observational analysis of patients presented with adrenal mass in the Department of Urology, NRSMCH in last 3 years (2019-2021).
Aims and objectives
To study the incidence, presentations, functionality, pathological types of adrenal tumors presented in a tertiary care centre in Kolkata, Eastern India.
Inclusion criteria
• Patient presented with adrenal tumors
• Both sex will be included
• Age group 8 yrs-80 yrs
Exclusion criteria
• Already operated patients
• Surgically unfit patients
• Patient unwilling to undergo surgery
Patient’s clinical information, preoperative imaging findings, biochemical parameters, operative findings, complications if any and follow-up data has been recorded. A few patients with uncommon presentation will also be described [9-12].
Results
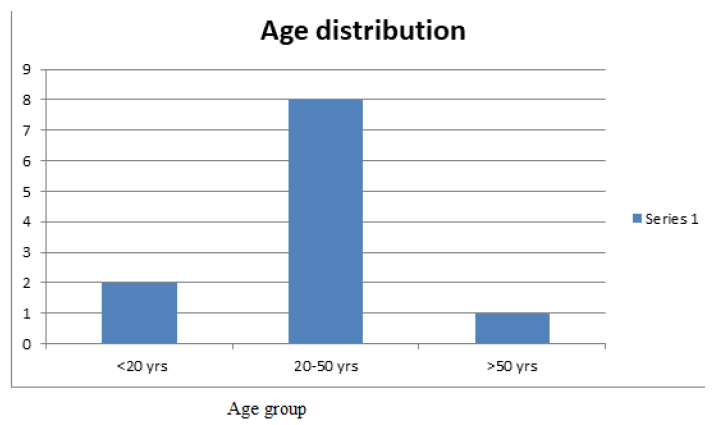
A total of 11 patients presented with adrenal mass at our Out Patient Department (OPD) in between January 2019 to December 2021. Minimum age was 17 yrs and maximum was 55 yrs. We divided the patients into three age groups. Group a (<20 yrs), group B (20-50 yrs) and group C (>50 yrs). 2 patients were below 20 yrs (group A %), 8 were in the group B (%) and 1 patient were above 50 yrs (group c %) (Figure 1).
6 patients were male and 5 were female. So M:F ratio was almost 50:50 in our series (Figure 2).
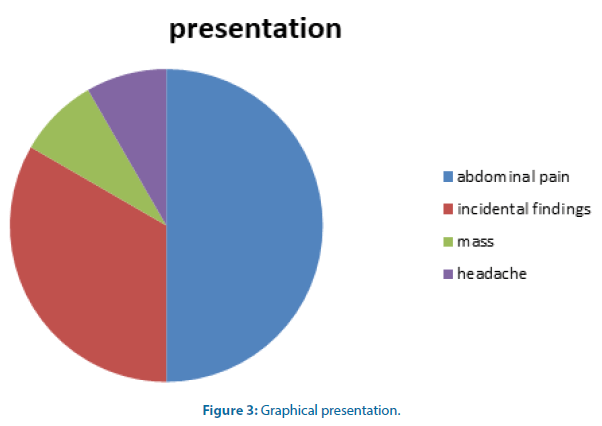
Regarding presentation, 4 patients presented with incidental finding (Figure 3). Another 6 patients presented with abdominal pain. One patient presented with abdominal mass and rest one patient presented with functional features like headache, palpitations and sweating. This patient was having a pheochromocytoma [13,14].
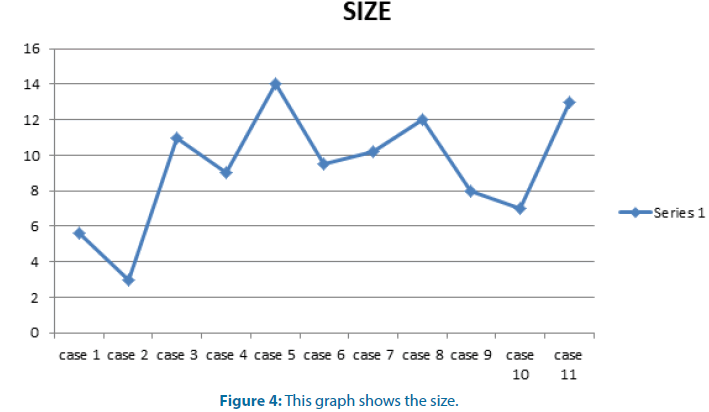
Preoperative imaging findings: average mass size on CT scan was 7.5 cm with the maximum size of 14 cm and the minimum mass size of 3 cm. 3 masses were found to be abutting Inferior Vena Cava (IVC) (Figure 4).
Among the 11 cases only one patient has a functional tumor and which on Histopathological Examination (HPE) was found to be pheochromocytoma. Rest of the adrenal masses were non-functional even also including the two cases of ACC who undergone laparoscopic adrenalectomy. One case has been converted to open because of the size of tumor and dense adhesions all around. Rest 6 cases a thoraco-abdominal open approach has been taken. Complete excision of all the cases done. No significant intraoperative complications happened except for IVC lateral tear in one case which has been managed with vascular suturing. On HPE-8 patients were having myelolipoma (73%), 2 patients were of ACC and 1 patient was having pheochromocytoma. Both the ACC were non-functional.
We followed up the patients for a mean duration of 18 months. Follow-up protocols include clinical examinations, CECT whole abdomen and pelvis 6 monthly in first years then Ultrasonography whole abdomen (USG) biannually, biochemical assessments including routine blood tests, hormonal assays. None of the patients develop any kind locoregional recurrences. Two patients develop hypertension in the follow up time and been well controlled with single antihypertensive.
Discussion
The etiology of adrenal incidentalomas varies and includes benign and malignant lesions derived from the adrenal cortex, the medulla or of extra-adrenal origin. The reported frequency varies, depending on the context of the study and inclusion size criteria (Table 1).
Table 1: The reported frequency varies, depending on the context of the study and inclusion size criteria
| Tumor entity | Median (%) | Range (%) |
|---|---|---|
| Adenoma | 80 | 33-96 |
| Nonfunctioning | 75 | 71-84 |
| Autonomously cortisol-secreting | 12 | 1.0–29 |
| Aldosterone-secreting | 2.5 | 1.6-3.3 |
| Pheochromocytoma | 7 | 1.5-14 |
| Adrenocortical carcinoma | 8 | 1.2-11 |
| Metastasis | 5 | 18 |
| Adenoma | 55 | 49-69 |
| Nonfunctioning | 69 | 52-75 |
| Cortisol secreting | 10 | 1.0-15 |
| Aldosterone secreting | 6 | 2.0-7.0 |
| Pheochromocytoma | 10 | 23-Nov |
| Adrenocortical carcinoma | 11 | 1.2-12 |
| Myelolipoma | 8 | 7.0-15 |
| Cyst | 5 | 4.0-22 |
| Ganglioneuroma | 4 | 0-8.0 |
| Metastasis | 7 | 0-21 |
The frequency of small benign adrenocortical tumors gradually increases with age, ranging between 3%-7% in adults over 50 years [1,2]. Usually they are discovered incidentally, in the context of abdominal Computed Tomographic (CT) or Magnetic Resonance Imaging (MRI) scans performed for various unrelated purposes. Hormone-secreting benign adrenal adenomas are rare; equally rare are hormonally silent or hormonesecreting adrenocortical carcinomas. Malignant neoplasias of the adrenal cortex account for 0.05%- 0.2% of all cancers, with an approximate prevalence of two new cases per million of population per yr [1-3]. Adrenal cancer occurs at all ages, from early infancy to the seventh and eight decades of life [3- 8]. A bimodal age distribution has been reported, with the first peak occurring before age 5 yr, and the second in the fourth to fifth decade [3]. In all published series, females clearly predominate, accounting for 65%-90% of the reported cases [3- 8]. Whereas some investigators report a left-sided prevalence, others note a right-sided preponderance [3, 7, 8, 15-17]. Bilaterality has been reported in 2%- 10% of the cases [3, 7].
In our study of 11 cases, the incidence of adenoma was 73% which is bit less than the usual incidence (80%). ACC was found in 2 cases in our series (18%), which is a bit higher than the usual incidence (11%). Adrenal masses were found to be in the 17-55 yrs group, most of the patient is in age group 20-50 yrs. Male to female ratio was almost 50:50 which is in contrary to the earlier published series where female usually predominates. Functional adrenal masses were only one (9%), which was pheochromocytoma. No bilateral case has been seen in our series. Average size of the tumors were 7.5 cm with maximum size upto 14 cm. Laparoscopic adrenalectomy was done in 4 cases and open approach has been adopted in rest. For open approach, thoracoabdominal incision was required as they were very large in size. All patients had been followed up for a median of 18 months with clinical examination, biochemical evaluation and imaging initially with CECT and then USG. 2 patients developed HTN which was controlled by one drug. None of them had any recurrences.
Conclusion
To conclude, adrenal tumors have a varied presentation with most of them are incidentally discovered. Most of them are non-functional tumors and mostly are adenoma but having a large size with an average of 7.5 cm. Focused work up, timely surgical intervention and close follow up leads to complete cure in most of the cases.
References
- Nasir J, Walton C. Adrenal mass with virilisation: Importance of endocrine investigation. BMJ. 313:872‑873 (1996).
- Lim YJ, Lee SM, Shin JH, et al. Virilizing adrenocortical oncocytoma in a child: A case report. J Korean Med Sci. 25:1077‑1079 (2010).
- Tahar GT, Nejib KN, Sadok SS, et al. Adrenocortical oncocytoma: A case report and review of literature. J Pediatr Surg 43:E1‑3 (2008).
- Latronico AC, Chrousos GP. Adrenocortical tumors. J Clin Endocrinol Metab. 82:1317–1324 (1997).
- Liou LS, Kay R. Adrenocortical carcinoma in children: Review and recent innovations. Urol Clin North Am. 27(3):403-421 (2000).
- Mendonca BB, Lucon AM, Menezes CAV, et al. Clinical, hormonal and pathological findings in a comparative study of adrenal cortical neoplasms in childhood and adulthood. J Urol. 154:2004-2009 (1995).
- Luton JP, Cerdas S, Billaud L, et al. Clinical features of adrenocortical carcinoma, prognostic factors and the effect of mitotane therapy. N Engl J Med. 322:1195-1201 (1990).
- Bharwan N, Rockall AG, Sahdev A. Adrenocortical carcinoma adrenocortical carcinoma: The range of appearances on CT and MRI. Am J Roentgenol. 16:457-468 (2011).
- Pommier RF, Brennan MF. An eleven-year experience with adrenocortical carcinoma. Surgery. 112:963-971 (1992).
- Barzon L, Sonino N, Fallo F, et al. Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol. 149:273-285 (2003). (doi:10.1530/eje.0.1490273)
- Cawood TJ, Hunt PJ, O’Shea D, et al. Recommended evaluation of adrenal incidentalomas is costly, has high falsepositive rates and confers a risk of fatal cancer that is similar to the risk of the adrenal lesion becoming malignant; time for a rethink? Eur J Endocrinol. 161:513-527 (2009).
- Favia G, Lumachi F, Basso S, et al. Management of incidentally discovered adrenal masses and risk of malignancy. Surgery. 128:918-924 (2000).
- Grumbach MM, Biller BM, Braunstein GD, et al. Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med. 138:424-429 (2003).
- Kloos RT, Gross MD, Francis IR, et al. Incidentally discovered adrenal masses. Endocr Neoplasms. 16 (1995 ).
- Tahar GT, Nejib KN, Sadok SS, et al. Adrenocortical oncocytoma: A case report and review of literature. J Pediatr Surg. 43:E1-3 (2008).
- Yildiz BO, Bolour S, Woods K, et al. Visually scoring hirsutism. Hum Reprod Update. 16:51-64 (2010).
[Google Scholar] [Cross Ref]
- Sharma D, Sharma S, Jhobta A, et al. Virilizing adrenal oncocytoma. J Clin Imaging Sci. 2:76 (2012).