Research Article - Clinical Investigation (2022) Volume 12, Issue 12
Pre-treatment Verification of Carcinoma Breast VMAT plan based on Mono-isocentric technique : Assessment of the combined fields feature of new 2D MatriXX arrays
Raoui Yasser*
1Esmar Team, Department of Physics, Faculty of Sciences, Mohammed V University in Rabat, Morocco
- Corresponding Author:
- Raoui Yasser
Esmar Team, Department of Physics, Faculty of Sciences, Mohammed V University in Rabat, Morocco
E-mail: raoui.yasser@gmail.com
Received: 03-Aug-2022, Manuscript No. fmci- 22-71094; Editor assigned: 05- Aug -2022, PreQC No. fmci-22- 71094 (PQ); Reviewed: 06- Aug -2022, QC No. fmci-22-71094 (Q); Revised: 09- Aug -2022, Manuscript No. fmci-22-71094 (R); Published: 30-Dec-2022; DOI: 10.37532/2041-6792.2022.12(12).261-271
Abstract
Objective: The aim of our work is to verify Mono-Isocentric technique based Volumetric Modulated Arc Therapy (VMAT) plan for carcinoma breast and regional nodes employing the new 2D arrays Matrix Resolution from IBA dosimetry systems, Schwarzenbruck, Germany loaded with the combined field feature.
Methods: This study included 12 Mono Iso-centric VMAT plans for breast cancer with supraclavicular and axillary nodes. The radiotherapy planning was performed by the Monaco TPS (5.51 Elekta Limited, Crawley, UK) following the departmental planning protocols employing 6 MV photons using XVMC algorithm for Dose calculation.
The plans were optimized using an arc geometry with 25 increments in gantry angle spacing between control points with a 3 mm resolution dose grid size and 1% per calculation dose to medium, minimum segment width 0.5 cm and high fluence smoothing.
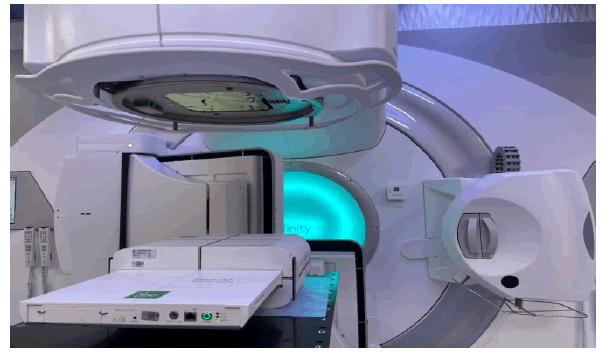
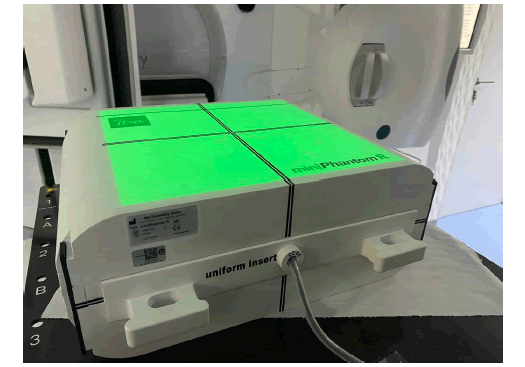
These plans were delivered clinically by an Elekta Infinity linear accelerator equipped with Agility 160 leaf MLC (Elekta Limited, Crawley, UK). Two CT scans of the Matrix resolution inserted in the Mini Phantom R were acquired using CT simulator (GE discovery (General Electricals, USA). Out of these two scans, the first one taken as the default CT and the second one as the extended CT, in order to use it for large fields combination.
In this study, normal and combined fields were compared using my QA patients’ software (IBA Dosimetry, Germany) based on the gamma index analysis and point dose measurements with the ion chamber cc04 according to IAEA Protocol TRS398.
Results: The new 2D array detector provided good agreement for dose maps without combined field feature over the field lengths ranging from 22 cm to 24 cm and excellent agreement for maps with combined fields for lengths ranging from 24 cm to 28 cm. VMAT Clinical cases passed with more than 95% for the set criteria of 3% DD & 3 mm. The absolute point dose measurement agreement was found to be more than 98%.
Conclusion: The Matrix Resolution is a convenient, fast, robust, and practical tool for routine large-field pre-treatment verification in IMRT, VMAT and other advanced techniques.
Keywords
Patient specific quality assurance •Combined field •My QA software •2D array detector
Introduction
Breast cancer is one of the most commonly diagnosed cancers, contributing up to 30% of all new cancer cases in women placing a significant burden on the workload of most radiotherapy departments [1]. Radiotherapy is an essential component in the local and regional management of breast cancer, reducing local recurrence in higher risk patients improving adjuvant survival.
The topology of this case is complex and achieving both the dose homogeneity to the target volume and dose constraints to the surrounding tissues poses great challenges in radiotherapy treatment planning.
In recent years Intensity-Modulated Radiotherapy (IMRT) and Volumetric Modulated Arc Therapy (VMAT) have been adopted for the use of breast or chest wall treatments with supraclavicular and axillary nodes and they proved to be more suitable for creating an optimal treatment plan [2].
A dual isocenter approach accommodates patients with larger targets volumes, but prolonged treatment time may introduce uncertainty in the dose at the matching plane due to daily setup variations.
Multi-partial arc VMAT can provide plans with better dose homogeneity within the target and helps in achieving dose constraints to Organ at Risk (OARs).
Furthermore, by combining continuous gantry rotation, variable dose rate, and dynamic beam modulation, highly conformal dose distributions are achieved [3, 4]. Patient-Specific Quality Assurance is required for increasingly complex VMAT plans with sharp gradients (PSQA). Pre-treatment verification is fundamental for detecting any discrepancies between planned and delivered doses in all VMAT plans [5]. This is usually accomplished by applying the treatment plan to a diametric phantom and comparing the measured and calculated phantom dose distributions using the Gamma Index (GI).
Low et al. introduced the method of quantitatively comparing measured and calculated dose maps [6]. Absolute dose distribution measurements in a 2D plane or 3D geometries can be performed using detector arrays made up of ion chambers or diodes. The present study was taken to investigate the performance of the new 2D detector from IBA Dosimetry, the matrix resolution, and a Mini Phantom R in large fields with and without the feature combined field in my QA software for Mono Iso centric VMAT plans in case of breast cancer with supraclavicular and axillary nodes [7, 8].
Materials and Methods
In the present study, 12 patients of ca breast including the supraclavicular and axillary nodes were studied to achieve the aim of this study. All the 12 patients were planned using Mono-Iso-centric VMAT techniques. First, CT scans (Discovery, General Electric, USA) of all the 12 patients were acquired simulating as per the institutional guidelines for VMAT planning (Table 1). The slice thickness of these CT acquisitions was 2.5 mm done on 120 KV. Then acquired CT image set was transferred to the contouring work station where different organs including body and targets were delineated. Also, CT to ED curve, generated with the help of CIRS electron density phantom was applied in these 12 patient’s VMAT planning using Monaco TPS (V 5.5.1, Elekta Medical system, Sweden) utilizing the XVMC algorithm. Table 1 shows the constraints and the parameters applied in these.
Table 1. Optimization parameters used to plan a VMAT cases.
| Parameter | Value |
|---|---|
| Beamlet width | 0.3 cm |
| Surface margine | 0.2 cm |
| Auto flash margine | 1.5 cm |
| Target margine | tight 2 mm |
| Arcs geometry | 2 Arcs : 1 Auto , 2 Fixed only on the breast |
| Incrément | 25 Deg |
| Séquentiel | 180 CP |
| Collimator | 0 Deg |
| Leaf Width | 0.5 mm |
| Fluence Smoothing | High |
The VMAT plan for each of the 12 patient was optimized using Monaco planning system with the constrained mode and the parameters listed in the Table 1 below: An auto-flash margin option was used for VMAT plans and the Multileaf Collimator (MLC) leaves were opened outside of the body contour
A 6 MV photon energy and Agility MLC were used to create the Monaco VMAT treatment plans. The final dose was calculated using X-Ray Voxel Monte Carlo (XVMC) with 0.3 cm voxel size and 1% calculation uncertainty. To achieve agreement with the physician prescription and OAR tolerances, IMRT constrained was used as shown in Table 2.
Table 2. Planning constraints used in VMAT cases using Monaco TPS
| Structure | Cost Function | Parameters |
|---|---|---|
| Breast PTV | Target Penalty Quadratic Overdose | Prescription 50 Gy Minimum Volume Dose (%)=95 |
| Regional Nodes PTV | Target penalty | Prescription 50 Gy |
| Minimum Volume Dose (%)=95 | ||
| Quadratic Overdose | Maximum Dose (Gy) =54.5 | |
| RMS =0.05 | ||
| Spinal Cord +0.5 cm | Serial | Equivalent Uniform Dose (Gy)=20 |
| Power Low Exponent =12 | ||
| Heart | serial | Equivalent Uniform Dose(Gy)=8 |
| Power Low Exponent =16 | ||
| Oesophagus | parallel | Reference Dose(Gy) =30 ; Mean Organ Damage(%) =40 |
| Power Low Exponent =3 | ||
| Humeral Head | serial | Equivalent Uniform Dose(Gy)=28 |
| Power Low Exponent=12 | ||
| Liver | parallel | Reference Dose (Gy)=20 ; Mean Organ Damage(%) =40 |
| Power Low Exponent =4 | ||
| Homolateral Lung | Parallel | Reference Dose(Gy) =20 ; Mean Organ Damage(%) = 27 |
| Power Low Exponent =4 | ||
| serial | Equivalent Uniform Dose(Gy) =18 | |
| Power Low Exponent =1 | ||
| serial | Equivalent Uniform Dose(Gy) =37 | |
| Power Low Exponent =12 | ||
| Over Dose DVH | Objective Dose(Gy) =30 | |
| Maximum Volume(%) =19 | ||
| Larynx | Serial | Equivalent Uniform Dose(Gy)=37 |
| Power Low Exponent=12 | ||
| parallel | Reference Dose(Gy) 30 ; Mean Organ Damage(%) =6 | |
| Power Low Exponent=4 | ||
| Body | Quadratic Overdose | Maximum Dose(Gy) =50 |
| RMS =0.3 | ||
| Quadratic Overdose | Maximum Dose(Gy)=35 | |
| RMS =1.2 | ||
| Quadratic Overdose | Maximum Dose(Gy) =25 | |
| RMS =0.04 | ||
| Maximum | Maximum dose(Gy) =54.5 | |
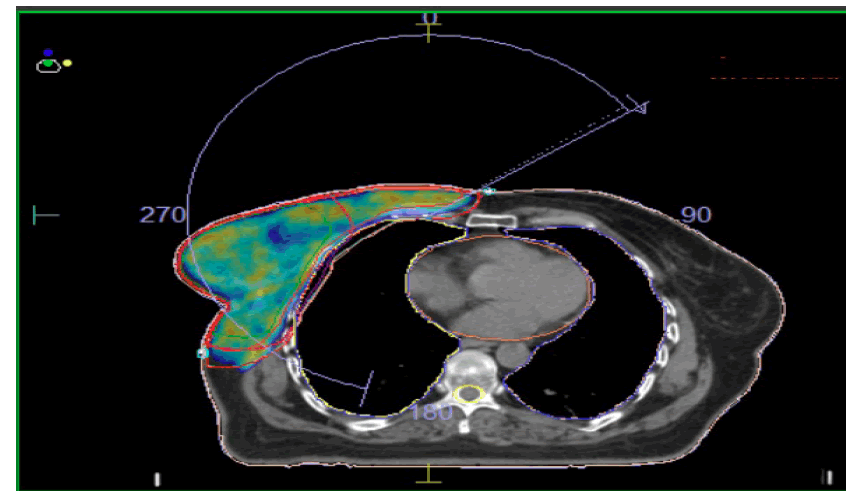
Generation of QA plan in the TPS: Firstly, CT scan images of all the patients were transferred to Monaco TPS. After this, a relative electron density of 1.016 and 1.030 were assigned to the RW3 Mini Phantom-R and Matrix Resolution detector respectively. After optimization, VMAT plan was completed shown in Figure 1, the patient specific Quality Control (QA plan) was performed using the scanned Matrix for both the cases at the planning system level, next, and exported the plan to the Mosaiq record and verify system.
Method of measurement
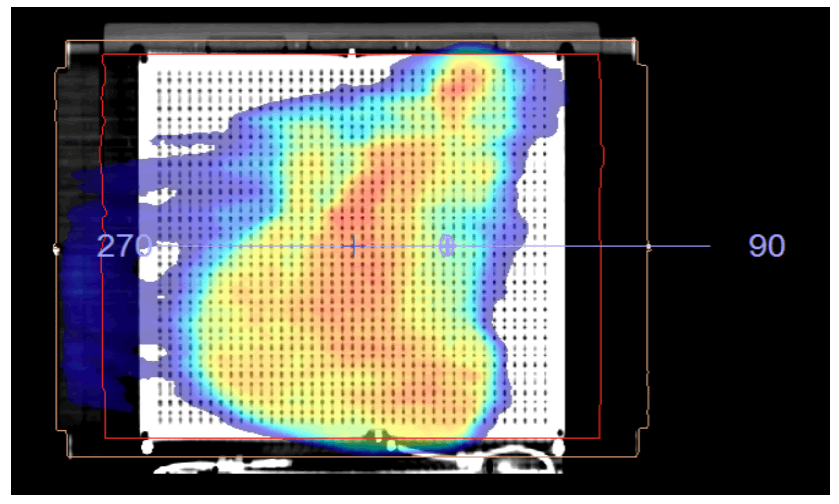
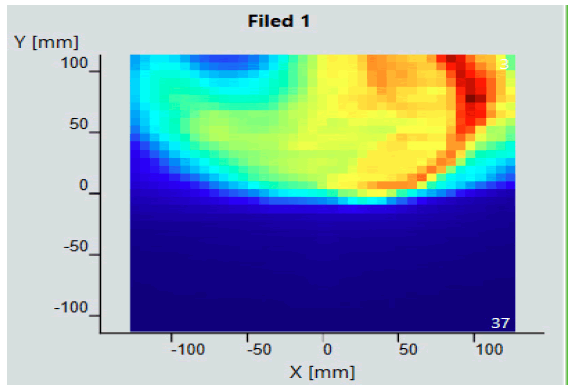
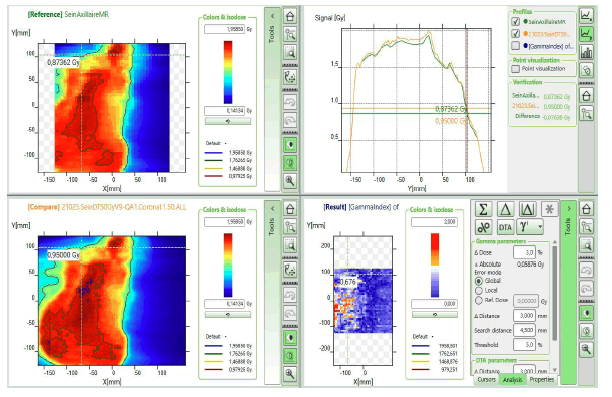
To generate the measurement maps without the combined field feature, the center of the Matrix Resolution was aligned with the isocenter of thelinac and then delivered the Arcs of the VMAT plan using Integrity MLC (Elekta Inc.). The recorded dose planes on detector is shown in Figure 2.
As a second step we aligned the isocenter to the 3rd row (a marker is printed in the Mini Phantom R) of the sensors from the edge of the Matrix Resolution detector.
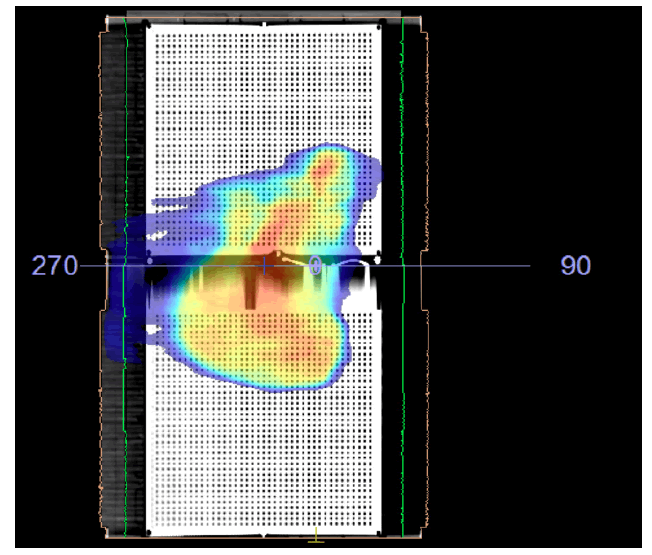
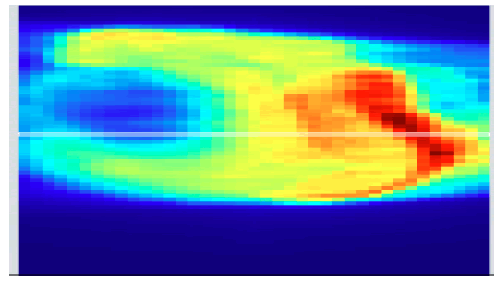
For the maps with the combined field feature, the first m easurements w as p erformed a t 0 ° o f t he devices and Arcs of the plan were delivered after this device was rotated to 180°, aligning the isocenter with the center of the 3rd row and deliver the Arcs. The dose maps of the combined field thus obtained are shown in Figure 3.
Working of matrix resolution
The sensors of the Matrix Resolution are designed in unique way of vented pixel ionization chambers. Each of these chambers has their own measurement channel. When chambers are irradiated, the air inside the chambers gets ionized. Thus the released charges are separated with the help of electrical field applied between the bottom and the top electrodes. The flow of changed constituting current is proportional to the dose rate, is measured and digitized by analogto-digital converters. The my QA patient software analyses the measured 2D dose distribution and compares it with the one calculated by the TPS.
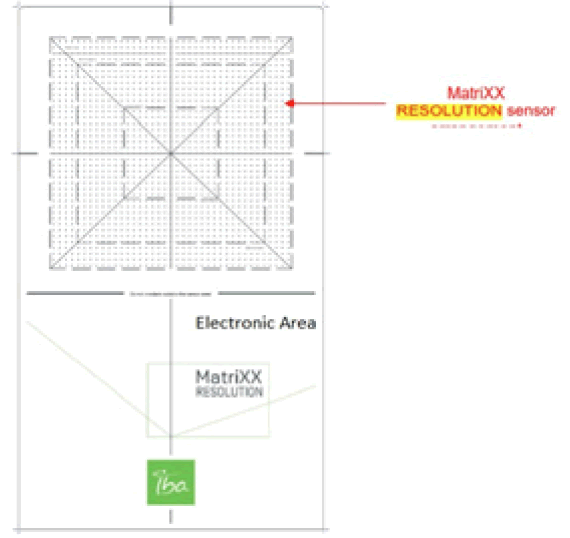
The Matrix Resolution has 1521 chambers arranged in a 39 cm × 39 cm grid matrix that cover an active field of 25.3 cm × 25.3 cm at 100 cm SDD. The effective point of measurement of the central chamber is positioned at the iso-center. The distance between the individual chambers is 6.5 mm center to center as shown in Figure 4
The combined fields feature
The Combine Fields tool, which combines two fields in the longitudinal direction, enables performing Patient QA for large fields. For a field larger than the detector sensor area, two measurements are taken, an upper and a lower section, with a small amount of overlap to ensure full coverage. Figure 5 shows the matrix assembly with isocenter location.
The two field sections are combined into the completed field by applying the combine fields wizard.
Point dose measurement
Also, point dose measurement was done for the same clinical cases, the TPS calculated dose on the Mini Phantom R and the ionization chamber employed in this study was CC04 (IBA Dosimetry, Germany) connected to IBA DOSE 1 electrometer. The chamber has a cavity length of 3.6 mm, a diameter of 2.0 mm, a volume of 0.04 cm3 , and a wall thickness of 0.070 g/cm2 , temperature and pressure were measured and the dose determination was performed according to IAEA TRS 398.
Statistical Analysis
Gamma IndexThe gamma index criteria is the gold standard QA tool for assessing the agreement between TPS calculated data and phantom measured one in case of VMAT planning, as well [9]. It was developed to combine the two previous assessment criteria viz Dose Difference (DD) and distance to agreement DTA. This important quantity is essential in confirming the correct delivery of the complex dose distributions seen in modern IMRT [10].
Results
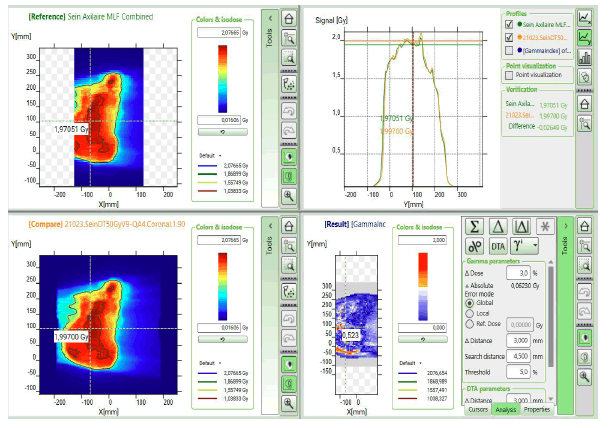
Initial setup of matrix resolution detector is shown in Figure 6. Twelve patients were undertaken for the study and the gamma measurement with and without combined field measurement was performed using IBA Matrix 2d array detector. The dose maps with lower, upper and combined fields were measured as shown in Figures 7-11 showing my QA results using combined field feature to analyse gamma index [11].
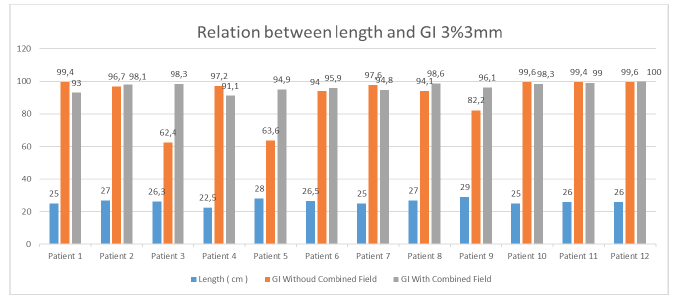
For the 3%/3 mm DTA (Dose to agreement) parameter the tumor length greater than 25 cm shows good agreement in results with combined field tool and for less than 25 cm tumor length size, the gamma index value shows good agreement even with the single field analysis tool. Figure 12 shows the G.I results obtained using combined tool are greater than 95% for tumor length size greater than 25 cm.
Figure 12:Relation between gamma index and lenth of tumor at 3%/3 mm criteria.
At 3%/3 mm DTA and tumor length 27 cm gamma index passing using combined field tool found to be 98.1% compared to the gamma index without combined field tool which was found to be 96.7%. For 26.3 cm tumor length gamma index passing percentage without using combined field tool was found to be 62.4% compared to using combined field tool which was recorded 98.3%. Similarly, for 28 cm tumor length the result obtained without using combined field was 63.6% which showed good agreement of 94.9% when using combined field tool. For smaller tumor length of 22.5 cm, the results obtained without using combined field tool was better (97.2%) than considering the analysis using combined field tool resulted lowering of gamma passing percentage to 91.1%.
For 3%/2 mm DTA parameters the gamma index obtained for tumor length sizes near to 25 cm shows comparable results using combined tool and without combined tools. Again for tumor length greater than 25 cm Gamma Index passing percentage will be better while opting combined field tool and for length less than 25 cm better Gamma Index passing percentage was obtained without using combined tool. Figure 13 shows the result analysis for 3%/2 mm DTA parameters for gamma index analysis for varying tumor length using combined field and without combined field tool option in my QA software.
Figure 13: Relationship between gamma index and length of tumor at 3%/2 mm criteria.
Point dose assessments in mini phantom R setup were performed as shown in Figure 14 for all the clinical cases studied in this present research work with breast cases and supraclavicular involvement following TRS 398 protocols. The maximum variation of 1.6% was observed amongst all the 12 cases. The point dose difference criteria we re acceptable as per the recommendations for all clinical cases investigated here [12, 13]. Table 3 shows the data obtained while performing point dose measurement using mini R phantom and cc04 ionization chamber.
Table 3. Assessment of point dose differ-ences in calculated and measured values.
|
Calculated dose [Gy] | Mesured dose [Gy] | Standard deviation |
|---|---|---|---|
| Patient 1 | 1.484 | 1.485 | 0.06% |
| Patient 2 | 1.849 | 1.849 | 0.10% |
| Patient 3 | 1.733 | 1.723 | 0.58% |
| Patient 4 | 1.469 | 1.46 | 0.60% |
| Patient 5 | 1.736 | 1.757 | 1.20% |
| Patient 6 | 1.522 | 1.54 | 1.16% |
| Patient 7 | 1.698 | 1.68 | 1.07% |
| Patient 8 | 0.495 | 0.502 | 1.40% |
| Patient 9 | 1.624 | 1.614 | 0.61% |
| Patient 10 | 1.654 | 1.65 | 0.24% |
| Patient 11 | 1.903 | 1.92 | 0.88% |
| Patient 12 | 1.613 | 1.64 | 1.64% |
For tumor size less than 25 cm using combined tool results lower Gamma Index passing results for both DTA parameters of 3%/3 mm & 2%/2 mm. For all the plans, Gamma evaluation was performed using Global mode with the preferred dose to agreement passing criteria. Term “Global” indicates maximum dose normalization in a given volume. The threshold value of 5% is selected in every plan analysis to nullify the contribution of background scattered noise.
Discussion
At slightly strict Gamma index passing criteria i.e. 3%/2 mm, the results obtained for tumor size 25 cm was 98.3% without using combined field tool compared to passing rate of 91% while using combin--ed field feature [14]. For tumor size 22.5 cm, the results without using combined field option was 91.1% however it lowered downs to 86.8% while used with the combined field tool. For the tumor length 29 cm, the Gamma index passing without using combined tool option was 76.6% while the passing rate reached to 93% when combined field tool option for analysis was employed.
The Global dose gamma analysis resulted in higher passing rate for tumor length greater than 25 cm while using combined field feature other than without combined field feature. Th e ac tion limits of thresholds in all analysis was kept constant of 5% which reduces the large number of low dose regions, which may results in inflated passing rate when evaluated with the global gamma analysis. The active fi eld of detector was 25.3 cm × 25.3 cm and this is taken as the primary reason for good agreement with the results obtained for tumor length upto 25cm even without using combined field tool option.
For larger tumor length greater than 25 cm, if combined field option would not include for analysis then there is a quite high chances of losing the data outside the active area which may results in disagreement between the calculated and measured fluence. In global mode analysis methodology maximum of the normalized volume were considered for comparison which makes the greater size tumors more susceptible to be associated with the errors. Analysis without using combined tool features in case of larger length compared to active detector size leads to lowering of gamma index passing.
The chances of error increases for tumor size less than 25 cm using combined tool option as there is always more probability of overlap of data during exposure to the active detector regions and results in compromising the scatter contribution which leads to lowering of gamma passing percentage. It is always advisable to use the combined field tool feature for tumor lengths greater than 25 cm which resulted in the good agreement with the planned fluence.
Point dose assessment in long field at i s o-center using ionization chamber CC04 shows the good agreement with the calculated TPS values and shows maximum variation of 1.64% in one case which is well acceptable as per the recommendations. The concurrence of point dose & gamma index passing gives the good idea of usefulness of combined field tool feature in long tumor structures.
Conclusion
The Matrix Resolution was found to be a handy, fast, robust and practical tool for the routine pretreatment verification of large fiel ds. Co mbined field feature is unique tool for analysis of the gamma index for tumor length greater than 25 cm and shows promising results.
References
- Kinhikar RA, Pandey VP, Jose RK, et al. Investigation on the effect of sharp phantom edges on point dose measurement during patient-specific dosimetry with Rapid Arc. J Med Phys. 38:139-42(2013).
- Ouardy k, Zerfaoui M, Herrassi Y, et al. Validation of Monaco TPS for an Elekta synergy MLCi2: Using gamma index for elekta full package beams. Mater Today Proc. 45(8)7685-89(2021).
- Raoui Y, Herrassi Y, Elouardy Kh, et al. Beam Modeling in Commercial Treatment Planning System for IMRT and VMAT performance with an Elekta MLCI 2 Multileaf Collimator. Iran J Med Phys. 18(6)1-9(2021).
[Google Scholar] [Crossref]
- Low DA, Dempsey JF. Evaluation of the gamma distribiution comparison method. Med Phys. 30:2455–64(2003).
- Teoh M, Clark CH, Wood K, et al. Volumetric modulated arc therapy: a review of current literature and clinical use in practice. Br J Radiol. 84: 967–96(2011).
- Kaneko A, Sumida I, Mizuno H, et al. Comparison of gamma index based on dosimetric error and clinically relevant dose-volume index based on three-dimensional dose prediction in breast intensity-modulated radiation therapy. Radiat Oncol. 14(1):36(2019).
[Google Scholar] [Crossref]
- Jin X, Yan H, Han C, et al. Correlation between gamma index passing rate and clinical dosimetric difference for pre-treatment 2D and 3D volumetric modulated arc therapy dosimetric verification. Br J Radiol. 88(1047):20140577(20105).
- Miften M, Olch A, Mihailidis D, et al. Tolerance limits and methodologies for IMRT measurement-based verification QA: Recommendations of AAPM Task Group No. 218. Med Phys. 45(4):53-83(2018).
- Low DA, Moran JM, Dempsey JF, et al. Dosimetry tools and techniques for IMRT. Med Phys. 38(3):1313-38(2011).
- Abbas AS, Moseley D, Kassam Z, et al. Volumetric-modulated arc therapy for the treatment of a large planning target volume in thoracic esophageal cancer. J Appl Clin Med Phys. 14(3):4269(2013).
- Wang X, Zhang X, Dong L, et al. Development of methods for beam angle optimization for IMRT using an accelerated exhaustive search strategy. Int J Radiat Oncol Biol Phys. 60(4):1325–37(2004).
- Stathakis S, Myers P, Esquivel C, et al. Characterization of a novel 2D array dosimeter for patient-specific quality assurance with volumetric arc therapy. Med Phys. 40(7):071731(2013).
- Nasseri S, Bahreyni MH, Momennezhad M, et al. Dosimetric verification of IMRT and 3D conformal treatment delivery using EPID. Appl Radiat Isot. 182:110116(2022).
- Jomehzadeh A, Shokrani P, Mohammadi M, et al. Assessment of a 2D electronic portal imaging devices-based dosimetry algorithm for pretreatment and in-vivo midplane dose verification. Adv Biomed Res. 5:171(2016).