Abstract - Interventional Cardiology (2009) Volume 1, Issue 2
Professor Raimund Erbel speaks to Laura Dormer, Launch Editor
- Corresponding Author:
- Raimund Erbel
Department of Cardiology, West-German Heart Center Essen
Hufelandstrasse 55, Essen, 45122, Germany
Tel: +49 201 723 4801
Fax: +49 201 723 5401
E-mail: erbel@uk-essen.de www.wdhz.de
Abstract
▪ You have been Director of the Department of Cardiology at the West-German Heart Center, Essen, Germany, since 1993. What led to your interest in interventional cardiology in particular?
Dealing with myocardial infarction in the early 1970s, it was disappointing to take care of patients, because we could only treat complications but not the myocardial infarction itself. It was really frustrating. The development of intracoronary thrombolysis and percutaneous coronary angioplasty (PTCA) in 1976/1977 changed the world, and treatment of acute myocardial infarction with interventional techniques became one of my research topics.
As a young fellow I was fascinated by the first pictures of Andres Grüntzig in 1977 demonstrating PTCA of coronary artery stenosis. It was the beginning and the beginning was difficult, time-consuming and not very successful. But the perspectives for the technique, which was pointed out, were more than fascinating and took my full interest for many years, so that I could start doing interventions by myself in 1982.
Interventional cardiology was also the reason why I went with Jürgen Meyer to Mainz, where I worked for 11 years from 1982 to 1993. Since 1993 I have been the Head of the Department of Cardiology in Essen, University Duisburg-Essen (Figure 1).
▪ Are there any particular scientists you have worked with who have had an impact on the path your research has taken?
During my lifetime in interventional cardiology I have been mainly influenced by the following scientists:
Jürgen Meyer
Jürgen Meyer did the first coronary PTCA in Aachen in 1978. I was chosen as a fellow who was able to assist and document the results, and I noticed his technical skills. The first attempts lasted between 3 to 5 h and only a few cases were successful.
William O´Neill & Andrew Buda
In 1986 I was invited by Andrew Buda to come to Ann Arbor (MI, USA). It was Bill O´Neill who demonstrated to me the high-frequency rotation angioplasty device, the rotablator, developed by D Auth. This contact led to the first rotablation in Germany in 1988, which had to be postponed due to the burning down of the cardiac surgery department. Otherwise, we possibly would have been the first in the world, even before Michel Bertrand in Lille.
Richard Schatz
During the first course of coronary stent implantation I could follow the demonstration of the balloon-expandable stent developed by Richard Schatz. I was immediately convinced that his approach was the most promising of all that were demonstrated and a close friendship developed between us. We were able to implant the first stent in Germany and the first Palmaz-Schatz stent worldwide in Mainz, in 1988.
Uri Rosenschein
A further important influence was the close contact with Uri Rosenschein (Tel Aviv, Israel), who had developed ‘ultrasound angioplasty’.
Bernd Heublein & Max Schaldach
For many years, I developed a close relationship with Bernd Heublein, Hannover, and Max Schaldach, Erlangen. Based on these contacts I was able to implant the first bioabsorble magnesium stent in 2004 and present the PROGRESS study.
Also, I do not want to forget many other scientists, to whom I have close contacts in interventional cardiology, such as Carlo Di Mario, Eberhad Grube, Martin Leon, P Yock, Peter Fitzgerald, Ron Waksman, Neil Weissman, David Holmes, Ian Penn, Donald Ricci and Pauline Margolis.
▪ How is your time balanced between managing the department & clinical & research work?
A lot of time is taken up by managing the department and seeing patients. But in my daily clinical work, I always try to include clinical research. In all cases that I see, clinical problems are present, and my main emphasis is to solve clinical problems. Based on their characteristics, many areas of interventional cardiology have been influenced.
▪ You recently reported the 5‑year outcomes of the Heinz Nixdorf Recall Study. Briefly, could you describe the main findings of the study?
The Heinz Nixdorf Recall Study tries to demonstrate the predictive value of coronary artery calcification in comparison with traditional and new risk factors. In 4814 participants, a detailed interview, clinical examination, analyses of risk factors and computed tomography had been performed between 2000 and 2003. A 5‑year follow-up observational period took place between 2003 and 2008. After 5 years, we evaluated the hard events (cardiac death and myocardial infarction) and could demonstrate that a high calcium score of more than 400 was highly predictive of increased risk, which was beyond that which could be given by traditional risk factors. For those with an Agatston Score in the electron beam computerized tomography of more than 400 during 5 years a more than 8% event rate was found, although this was less than 1% in those without coronary artery calcification. Currently, those at low risk are advised to live a healthy lifestyle, whereas those with high-risk scores are advised to begin riskfactor modification and therapy. In men and women with an intermediate risk, and an event rate of 1–2% per year or 10–20% over 10 years, imaging and nonimaging techniques are proposed for further risk stratification. When we applied coronary calcification in this group, we could reclassify approximately 15% to the high-risk group and approximately 60% to the lowrisk group. Only a total of 6% of the study group remained in the intermediate-risk category, meaning that we could improve the current risk stratification significantly.
Thus, in the first observational study in the general population, coronary calcium scoring has demonstrated improved risk prediction, which should be implemented in daily clinical work.
▪ What impact do you hope these results will have on the treatment of patients?
We are all confronted day by day with cases that are unexpected; for example, in spring 2009 to Philip Pool-Wilson, London, UK, and in autumn Helmut Drexler, Hannover. In order to prevent such events, risk prediction has to be improved, and we have to identify those who are at high risk and lead them to an improved lifestyle by intensive therapy of risk-factor modification. At the moment, calcium scoring is not yet reimbursed by insurance companies, but this has to be changed, and cardiologists have to take into account that this technique is able to demonstrate coronary atherosclerosis even before abnormalities are detected by coronary angiography.
▪ You have recently begun a study comparing the Hyper Q™ System with conventional ECG stress testing analysis. What do you hope to achieve from this study?
Risk stratification will be further improved when we can develop systems for the detection of myocardial ischemia. Risk prediction with coronary calcification scoring is not a perfect system. Therefore, additional techniques have to be developed that help to identify signs of myocardial ischemia. The Hyper Q™ System is able to give more insight into ECG recordings than we have available currently. We will try to demonstrate that with this technique, already abnormal electrophysiological signs can be detected that will help to identify those with myocardial ischemia and perfusion deficits.
▪ What other areas are you focusing your own research on at present?
I want to subdivide this question into different fields of research for interventional cardiology:
▪ The further improvement of invasive imaging techniques for identifying coronary artery sclerotic lesions and plaques at risk – vulnerable plaques – is a major project, which includes intravascular ultrasound and optical coherence tomography, but also in the future other techniques such as infrared analyses of plaque composition. The PROSPECT study of Greg Stone demonstrates the great importance of intravascular ultrasound in the field of diagnostic coronary angiography. Approximately 20–30% of coronary angiograms are regarded as normal or nearly normal in patients who are possibly at risk. I have tried to increase budgeting towards this field. Patients who leave our cathlab with a ‘normal’ result, meaning normal coronary angiogram but chest pain, abnormal ECGs or stress testings, are disappointed because we could not explain their symptoms or findings, which may be possible in up to 80% of patients using intravascular ultrasound and Doppler.
▪ The development and use of new nano coatings of stents, such as the Polyzen F, and development of bioabsorble magnesium or polymer stents.
▪ The improvement of recanalization of occluded coronary arteries by use of front-looking ultrasound in combination with intravascular ultrasound-guided coronary recanalization.
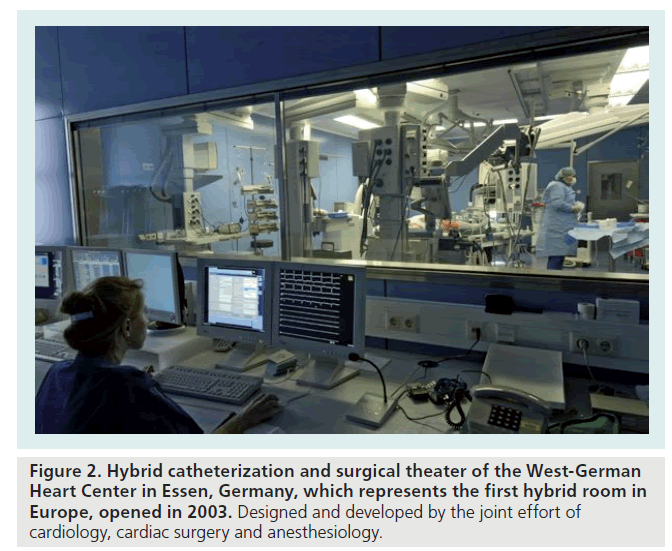
▪ Treatment of aortic dissection is one of the main topics of our research group. We have developed a new aortic stent that opens new possibilities and will hopefully improve results for treatment of patients with aortic diseases (Figure 2).
Figure 2: Hybrid catheterization and surgical theater of the West-German Heart Center in Essen, Germany, which represents the first hybrid room in Europe, opened in 2003. Designed and developed by the joint effort of cardiology, cardiac surgery and anesthesiology.
▪ The development and testing of new aortic valve prosthesis that we can implant not only in those with very severe aortic stenosis, but can also be used in those with other aortic abnormalities and valve diseases.
▪ The development of new techniques for mitral valve reconstruction such as the mitral clip and mitral ring suture techniques; possibly a combination of both.
▪ Ablation of hypertrophic obstructive cardiomyopathy with microspheres, in order to avoid alcohol ablation and the development of colliguation necrosis with the consequence of multiple conduction abnormalities (right bundle branch and left bundle branch block as well as total AV-block), and to induce microinfarcts and normal pathophysiological scar development instead of unnatural alcohol necrosis.
▪ Finally, what do you think will be the main areas of interest in the field of interventional cardiology over the next 5 years?
In the field of interventional cardiology, the treatment of valvular heart disease will be the main area of interest. People are getting older and the prevalence of degenerative diseases is increasing, which includes severe valvular aortic stenosis but also mitral regurgitation in patients with heart failure. In both fields, important progress can be expected. But in heart failure not only mitral regurgitation but also the interventional treatment of low output in the acute but also chronic setting will be the focus of a lot of attention, because in Germany, the elderly represent the largest group admitted to hospital. As heart transplantation is limited to a small group of patients, assist devices should also be used. In an aging population, diseases of the aorta are more often prevalent and have to be treated, but surgical interventions in these patients with multimorbidity is often too great a risk, and so interventional techniques are needed not only for the older population, but also for those with other vascular diseases.
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.