Research Article - Clinical Practice (2021) Volume 18, Issue 4
Quality of life of families with celiac disease children in Eastern Province of Saudi Arabia
- Corresponding Author:
- Samia Saud Al Furaikh
King Abdul Aziz Hospital of Ministry of National Guard for Health Affairs, Saudi Arabia
E-mail: amelmoataz@gmail.com
Abstract
Objectives: The prevalence of Celiac Disease (CD) is increasing worldwide, and the kingdom of Saudi Arabia reports the highest seroprevalence rate. A strict Gluten-Free Diet (GFD) for lifetime is the only therapy to CD patients. It has been demonstrated that childhood CD negatively affects the health of parents. On the other hand, the emotional and social wellbeing of the parents has a great impact on the Quality Of Life (QOL) of CD children. However, limited literatures are available on the QOL of parents of CD children. This study aims to evaluate the QOL of families of celiac disease children on GFD treatment and identify modifiable risk factors for poor QOL. Methods: A total of 73 children with celiac disease living in different cities of the eastern province of the kingdom of Saudi Arabia were included in this descriptive, cross-sectional study. A modified version of the celiac disease-specific instrument measuring the QOL was used. Data analyses were done using descriptive statistics, correlation coefficient test and the Fisher’s exact test. Results: The mean QOL score was found to be 65.8 and the median was 64.0. Very few (5.48%) parents perceived their QOL to be good, while majority of them (78.08%) considered it as moderate; and the remaining parents (16.44%) regarded it as poor. Conclusions: We found that small-sized families, with young and educated mothers have a better QOL than others. Most of the emotional and psychosocial elements of QOL were related to the difficulties in availability of GFD in daily life.
Keywords
quality of life, celiac disease, gluten-free diet, caregivers, children
List of Abbreviations
CD: Celiac Disease; GF: Gluten-Free; GFD: Gluten-Free Diet; QOL: Quality of Life; CD-QOL: Celiac Disease-Specific Instrument Measuring QOL; IDDM: Insulin-Dependent Diabetes Mellitus; DFGFD: Difficulties in Finding GFD; WHO: World Health Organization; HRQOL: Health Related Quality of Life; CD-HRQOL: Celiac Disease- Specific Health Related Quality of Life
Introduction
Celiac Disease (CD) is an immune-mediated enteropathy; caused by a permanent sensitivity to gluten in genetically susceptible individuals. It affects children and adolescents; and is characterized by gastrointestinal symptoms; dermatitis herpetiformis; and defects in dental enamel; osteoporosis; short stature; delayed puberty; and persistent deficiency of iron. It may also be present in asymptomatic individuals with type 1 diabetes; turner syndrome; down syndrome; Williams syndrome; first-degree relatives of CD patients; and those with selective Immunoglobulin (IG) A deficiency; as an underlying disease [1].
The prevalence of CD is increasing worldwide; including Europe, China, India, and Mediterranean regions like the Middle East and North Africa [2-5]. In comparison to other countries; the kingdom of Saudi Arabia has reported the highest seroprevalence rate of celiac disease; ranging from 1%-4%; mostly among children less than 18 years of age. The seroprevalence rates reported from different regions include the eastern region (2%); Madinah city (1.8%); and Al Qassim region (3.2%) [6-8].
The only effective standard treatment available for celiac disease is a strict Gluten-Free Diet (GFD) for lifetime. A study by Sansotta et al. demonstrated that pediatric patients following their diet very seriously; not only overcome stomach and intestinal discomfort; but also manage to reduce the risk of developing longterm health complications including cancers and bone deterioration [9]. However; strict adherence to a GFD can lower the Quality of Life (QOL) of celiac disease patients when social and emotional factors are considered [10]. The unavailability or higher cost of GFD; restrictive in participation in social gatherings lacking Gluten-Free (GF) food; and social stigma may be some of the contributing factors for lower QOL in CD patients and their caregivers [11].
The long-term consequences of childhood or adolescent CD can have a negative impact on the health of parents or caregivers who experience greater stress and sense of responsibility than parents of healthy children or adolescents [12]. Conversely; the emotional and social wellbeing of parents or caregivers has a great impact on the QOL of children with CD. However; limited literature is available on the QOL of family members of CD children who have been put on GFD treatment.
This study aims to evaluate the QOL of parents or caregivers of children and adolescents with celiac disease and to identify modifiable factors that negatively affect the QOL; especially those related to GFD availability and cost. The authors also aim to provide recommendations to improve the QOL of these patients to reduce the physical; emotional; and social burden on their parents and caregivers.
Material and Methods
◼ Study design and subjects
A descriptive; cross-sectional study was conducted among the families of children with celiac disease; living in different cities of the Eastern Province of the Kingdom of Saudi Arabia. The study participants were included regardless of their nationality. The data was collected for 78 children over a period of 2 years (2018 to 2019).
CD was diagnosed in children (aged 2-17 years) based on small-bowel biopsy. The caregivers or parents of children with CD on GFD for the past 6 months or more were invited to participate in the study through e-mail; wordof- mouth; or direct communication from Eastern province CD support group; pediatric gastroenterologists; and dieticians. Caregivers or parents were informed about the risks and benefits of the study and a written informed consent was obtained from them prior to the initiation of the study.
◼ Data collection
Parents were interviewed by a research assistant and study questionnaires were filled up. The questionnaires contained three parts:
Demographic data: Demographic data included respondent’s age; marital status; place of residence; family history of CD; consanguineous marriage; number of years since CD was diagnosed and availability of biopsy results to prove diagnosis; GFD interval and compliance; complications; and other comorbidities in both children and parents.
Modified version of Celiac Disease-Quality of Life (CD-QOL): CD-specific Quality of Life (CD-QOL); a 20-item validated survey instrument was modified to be used on the caregivers of CD children [13]. This instrument is divided into four subscales; dysphoria (4 items); limitations (9 items); health concerns (5 items); and inadequate treatment (2 items). Dysphoria subscale measured the extent to which individuals feel depressed; frightened; or overwhelmed by CD. Limitation subscale measured the extent to which individuals feel limited by CD when eating out with others; socializing; and traveling. The subscale on health concerns measured the extent to which individuals feel worried about long-term health outcomes of CD. Inadequate treatment subscale measured the extent to which individuals feel there are enough treatment options for their CD [14].
A 5-point Likert scale was used to record the answers from caregivers. The responses varied between not at all (NEVER-1); slightly (SOMETIMES-2); moderately (MOST OF THE TIME-3); quite a bit (OFTEN-4); and a great deal (ALWAYS-5). Each final score had a possible range from 0-100 with higher scores suggesting poor QOL.
The total scores were divided into 3 categories to facilitate analysis. Scores from 0-40 were classified as good QOL; that from 41-80 as moderate QOL; and scores falling in the range from 81-100 as poor QOL.
The questionnaire (CD-QOL) originally in English language was translated to Arabic language before the instrument was applied to the caregivers of CD patients. Next; the questions in English and Arabic language were reviewed by 5 different experts in CD; and modifications were done based on their feedback and comments. Four families with more than one child affected with CD; answered the questionnaire twice. Once; the mother’s responses were recorded; followed by the father’s responses and both the responses were then matched for any discrepancies. The responses given by mother and father were similar for majority of the questions.
Questions related to difficulties faced with availability of GFD at different places: Five items were added that related to difficulty finding GFD. One reflects general availability of GFD; while the others determined its availability at designated places like school; supermarket; restaurants; and bakeries.
Each item had 5 possible responses on the Likert scale reflecting the degree of difficulty: always was indicated the most difficult (5); often (4); most of the time (3); sometimes (2); and never reflected any difficulties (1). A score of 25 meant maximum difficulties while 5 indicated no difficulties.
◼ Data Analyses
Data was analyzed using the SPSS version 20 (Chicago; IL). Descriptive statistics (median; interquartile range; mean; standard deviation participants and variables according to the type and normality of data distribution. Correlation coefficient test was used to assess the relationship between QOL score and continuous variables (difficulty score; interval; number and percentages) were as used to describe the study participants between diagnosis and study time; and parents’ age). Fisher’s Exact Test was performed to examine the relationship between QOL and categorical variables (parents’ education; monthly income; family size and comorbidities).
Results
A total of 78 children with CD were invited to participate in the study. Out of 78; 5 patients were excluded as 3 did not have endoscopy done while 2 were beyond age limit. Thus; 73 patients were included in the study. All the included patients were diagnosed by serology and small bowel biopsy and were on GFD for more than 6 months. All the patients were residing in the Eastern Province of the Saudi Arabia Kingdom (Dammam-Al Khobar-Jubail - Dhahran-Al Hasa; Khafji-Ibgig Qatif ) and were followed by different health sectors (Ministry of National Guard; Ministry of Defense; Ministry of Health; Armed Forces hospital-Johns Hopkins Aramco Healthcare Specialty; and some private sectors).
Most patients were females (60.3%) with a mean age of 10.4 years; a majority of them were from Saudi (86.3%) and the parents of about 40% of the patients had a consanguineous marriage. 68.5% of the families had less than 6 members. More than 75% of all the included children were diagnosed with CD before their 10th birthday. 35 patients out of 73 (46.7%) had comorbidities and 21 patients of those had Insulin-Dependent Diabetes Mellitus (IDDM). Family history of CD was reported in 34.2% of the families and four families among them had more than one member diagnosed with CD.
More than half of the parents of all the included children had a university degree for both the father and the mother (53.4%; 56.2% respectively). Of all; 68.6% had a family income of 15000 SR or less per month and only 12 families had an income greater than 25000 SR per month (TABLE 1).
TABLE 1. Demographics of the study participants.
| Item | Mean (SD) | N (%) |
|---|---|---|
| Patient’s age | 10.14 (3.326) | |
| Patient’s age at diagnosis | 6.96 (3.066) | |
| Duration of illness | 3.27 (2.36) | |
| Father’s age | 44.82 (6.441) | |
| Mother’s age | 38.42 (5.997) | |
| Patient Gender | ||
| Males | 29 (39.7%) | |
| Females | 44 (60.3%) | |
| Comorbidities | 36 (49.3%) | |
| Mother’s Education | ||
| Less than University Degree | 12 (16.4%) | |
| University degree or above | 61 (83.6%) | |
| Father’s Education | ||
| Less than University Degree | 8 (11%) | |
| University Degree or above | 65 (89%) | |
| Family Monthly Income | ||
| Less than 15000 SR/month | 50 (68.5%) | |
| More than 15000 SR/month | 23 (31.5%) | |
| Family size | ||
| Less than 6 members | 50 (68.5%) | |
| More than 6 members | 23 (31.5%) | |
◼ Quality of Life
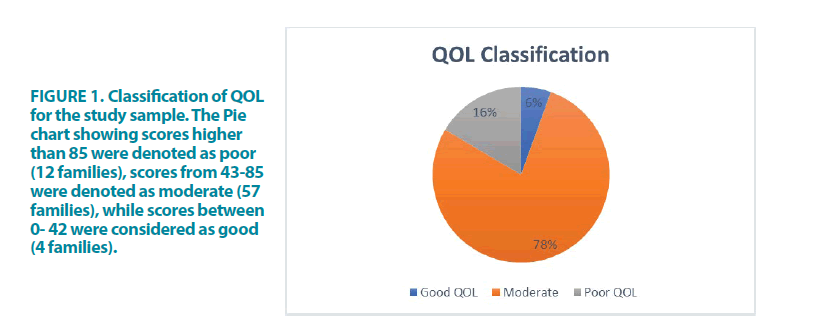
The mean QOL score was found to be 65.8 and the median was 64.0. Very few (5.48%) parents perceived their QOL to be good; while majority (78.08%) considered their QOL to be moderate; the rest of the parents (16.44%) regarded their QOL to be poor (FIGURE 1).
◼ Difficulties in Finding GFD (DFGFD)
Most of the parents expressed difficulty in finding appropriate GF food in supermarkets; restaurants; bakery shops; or making it available for the child at school. The mean of difficulty score was obtained to be 22.2 ± 2.9 out of 25; while the median was 92 with an Interquartile Range (IQR) of 16 out of 100; which indicates high difficulty level.
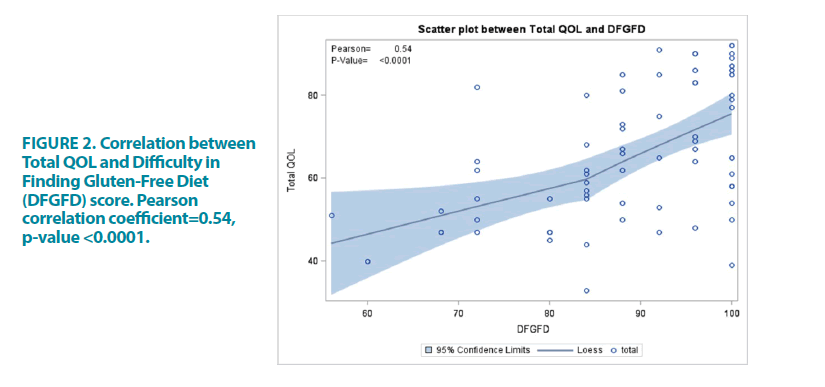
Correlation analysis showed a strong negative correlation between the total QOL score and the difficulty in finding GF food score as the higher the difficulty; the lower was the QOL (r=0.543; p=<0.0001) (FIGURE 2).
◼ Correlation of QOL with demographical data of study participants
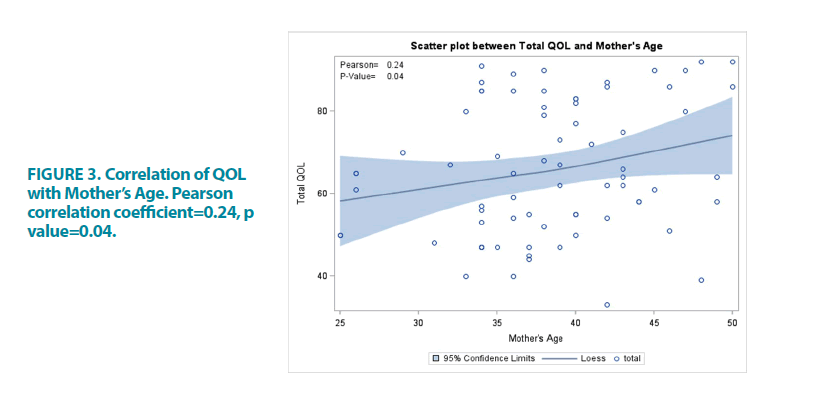
Parent’s age: Younger mothers reported better QOL. The mothers’ age was significantly correlated to the QOL score (r=0.240; p=0.040) (FIGURE 3).
Duration of illness: No correlation was found between QOL score; and the period between diagnosis and the participation in the study (the duration of illness) (r=0.109; p=0.356).
Family education and family size: Fisher’s exact test showed that a moderate QOL is more likely to be found among more educated mothers and fathers (Fisher’s exact test for mothers and fathers; respectively; p<0.033; p=0.005); and small size family (Fisher’s exact test; p<0.0799).
Family income and co-morbidities: No relationship was found between CD-QOL and family income (fisher’s exact test; p=0.4522) or co-morbidities (Fisher’s exact test; p=0.7494).
QOL domain scores: The QOL scale included four domains: (1) Limitations; (2) Dysphoria; (3) Health Concerns; and (4) Inadequate treatment. A significant correlation was observed between most QOL subscales and GFD Difficulty Score; mother’s age; and Fathers’ age (TABLE 2).
Table 2: Correlation Analysis of QOL Subscales.
| Limitation | Dysphoria | Inadequate Treatment | Health Concern | |
| 30.38 ± 7.65 | 12.41 ± 3.94 | 7.78 ± 1.83 | 15.26 ± 5.21 | |
| GFD Difficulty Score | ||||
| r | -0.515** | 0.465** | -0.178 | -0.493** |
| p | 0 | 0 | 0.131 | 0 |
| Mothers’ Age | ||||
| r | -0.158 | -0.192 | -0.339** | -0.249* |
| p | 0.181 | 103 | 0.003 | 0.033 |
| Fathers’ Age | ||||
| r | -0.126 | -0.242* | -0.161 | -0.233* |
| p | 0.289 | 0.039 | 0.174 | 0.047 |
*Significance level ≤ 0.05, **Significance level ≤ 0.01
Discussion
Health is defined by the World Health Organization (WHO) as a state of complete physical; mental; and social well-being of an individual and not only the absence of a disease [15]. Quality of Life (QOL); has been defined by WHO; as “an individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals; expectations; standards and concerns” [16]. Patrick and Erickson define Health Related Quality of Life (HRQOL) as “the value assigned to duration of life as modified by the impairments; functional states; perceptions and social opportunities that are influenced by disease; injury; treatment or policy” [17].
Over the past two decades; there has been growing interest in assessing the HRQOL of patients with chronic diseases including gastrointestinal illnesses [18-20]. Several studies concerning the HRQOL of adults with CD have been published [21-26]; yet pediatric and adolescent studies are still limited in numbers [27-29].
It is quite challenging to find a valid and reliable QOL tool that could be applied to different pediatric age groups. HRQOL can be assessed either by interview or questionnaire. Interview methods use open ended questions; useful for the creation of items to be used subsequently in questionnaires. Questionnaires are of two types: generic and disease specific. The generic questionnaire is used to evaluate HRQOL in different populations; it is insensitive and unresponsive to changes over time. Disease specific questionnaire is more sensitive to the issues that have affected patients with the disease. In CD; these issues may include the social; emotional; and financial burden because of a GFD [30].
HRQOL in patients with CD can be assessed by generic as well as disease-specific measures. Disease-specific questionnaires; however; provide more explicit information on diseaserelevant areas of functioning. A disease specific HRQOL instrument for CD would allow the health care providers to monitor their patients for such constrains; thereby enabling appropriate referrals to address these issues [31].
Van Doorn et al. found a discrepancy in the HRQOL when reviewing results from a pediatric population using a generic instrument and a CD-specific instrument [32]. While using the CD-specific instrument; the children reported a negative or neutral HRQOL; whereas the generic instrument showed the same children to have a positive HRQOL [32]. van Koppen et al. also found a discrepancy in outcomes on applying a generic instrument and a disease-specific instrument to the same study population; the children reported a good general HRQOL; but a neutral or low specific HRQOL [33]. In 2006; Hauser et al. developed a specific Celiac Diseasespecific Health Related Quality of Life (CDHRQOL) instrument for adult patients with CD. It covered 4 domains of health: emotion; social; worries; and gastrointestinal symptoms. It is suitable for patients above 18 years of age; however; it cannot be applied to children [34].
Few years later; Dorn SD et al.; through a series of focus groups; expert reviews; cognitive debriefing with patients and pilot testing; developed another CD-QOL scale with 20 items across four subscales (Limitations; Dysphoria; Health Concerns; and Inadequate Treatment). It was refined and administered on 387 Caucasian; highly educated females with CD on a GFD [13]. It was found to be a reliable and a valid measure of QOL in adult CD patients. The 20 items can be answered by adolescents and adults; but not by young children. Deepak C et al. from India used the CD-QOL in conjunction with generic scale SF-12 for patients above 12 years of age [35] and used 2 other scales: generic PSC and CD specific scale adapted from Chauhan JC et al. for patients below 12 years of age [36,37]. Al Nofaie et al. has recently used this adult CD-QOL for pediatric Saudi patients aged 9-18 years without mentioning the proxy and concluded that HRQOL for Saudi CD children on GFD is generally comparable to the healthy controls with the exception of the general health domain tested using the simultaneous generic SF-36 questionnaire [38].
When parents were asked to evaluate the QOL of their children using the CDDUX proxy version; they appraised their QOL to be more significantly negative than that reported by the children themselves [32]. A systematic review conducted by Eiser C et al. to determine the relationship between the ratings of children’s HRQOL made by parents and the children themselves. They concluded that though there is agreement for observable functioning; for example; physical HRQOL but no agreement for non-observable functioning (for example; emotional or social HRQOL) [39].
The study cohort in this research included children in whom CD had been diagnosed before their 10th birthday. Thus; the use of disease specific instruments and application of caregivers’ proxy version was not suitable. It is known that parental assessment of a child’s condition may overestimate the child’s actual QOL [40]. Bystrom et al. conducted a study on HRQOL in celiac patients from the perspectives of diseased children and their caregivers and found a significant discrepancy in reporting QOL. The parents scored significantly lower than the children when they were asked to evaluate their child’s HRQOL [12].
Despite the fact that psychological and emotional stress of the caregivers of children with chronic illness is considered a major factor affecting compliance to therapy and QOL of families and patients; studies evaluating the caregivers’ QOL are rarely reported [41]. In clinical practice; the caregivers’ well-being is not routinely assessed. Very few studies have adopted the caregivers’ perspective; mainly drawing the attention to their effect on patients’ QOL and treatment adherence [12,32]. Therefore; identifying QOL of families of CD children by analyzing the caregivers’ concerns and factors predicting caregivers’ burden can be relevant not only for their role in GFD adherence but also to determine a patient-centered care plan.
In the present study; the authors focused on parental psychosocial well-being through 4 domains: dysphoria; limitation; health concern; and treatment options. The CD-QOL questionnaire developed by Dorn SD et al. in 2010 was adopted. It has been applied on adults [13]; pediatric patients [38]; and recently Paiva A et al. have also applied it on caregivers [11]. In the present study; the questions were translated to Arabic language; the language spoken by Saudi citizens. The English version was also retained in the same questionnaire to include all families living in the eastern province regardless of their nationality. Of all families included only 6 were non-Saudi.
Studies fail to reach consensus on the impact of GFD on an individual’s QOL. Some studies reported an improved QOL for both; patients with symptom-detected CD and patients with screen-detected CD after one year of GFD [25]. Others reported similar QOL for those who were non-adherent to GFD [26]. Skjerning H et al. in 2014 conducted a qualitative study on the emotional impact of GFD on CD children. They investigated 76 celiac patients aged 2-18 years by using the Critical Incident Technique (CIT). Written answers to open-ended questions from children (older than 8 years) and parents (for children younger than 8 years) were analyzed qualitatively. It was concluded that both social situations and food were the most challenging factors affecting the daily life of CD children [42].
The present study aimed to explore the QOL of families of CD children and adolescents in relation to the difficulties in obtaining GFD regardless of the level of adherence to GFD. The degree of GFD difficulty is associated with reduction in patient’s wellbeing and psychological distress [43]. Sarkhy A et al. 2015 reported that the compliance to GFD among Saudi children is relatively poor (62%) compared to that in other parts of the world [44].
They found significant negative socio-economic impact; mostly related to the availability of GF food and its cost; in another study on the same cohort [44].
Some countries like Italy considered CD as a social disease and provided GF food to all CD patients for free [45]. Saudi government provides monthly financial support estimated at 200$ and GF food free of charge at military and National Guard hospitals for all families with CD patients [46]. Recently; at the time of the present study; the Ministry of Health in eastern province distributed GF food to all CD patients. However; children are not satisfied with varieties; taste; and availability of the GF food provided.
The GF food is expensive and mostly imported from western countries. In the present study; no relationship was found between CD-QOL and family income (fisher’s exact test=0.352; p=0.0001). This is consistent with a German study that failed to detect an association between lower social class and reduced HRQOL [34]. Yet; it is contradictory to the results of Paiva A et al. who reported that higher family income led to a higher QOL [11].The easy access to different varieties of good quality of GFD is more important to most caregivers than the ability to provide expensive food to their CD siblings. Non-availability of GFD at schools; restaurants; social gatherings; and lack of labelling on commercially available food at supermarkets are the common problems faced by families of children and adolescents suffering from CD [35].
The authors recommend that government owned food and drug organizations should be committed to make GFF available at restaurants; coffee shops; in schools with snacks suitable for different age group; in supermarkets with reasonable price and proper labelling of commercially available food products; and in local bakeries.
Consistent with other studies; most of the participants in this study were females [44;46]. Deepak C et al. reported more males (68.2%) than females in their pediatric study population varying between 2 and 12 years of age [35].
Chauhan JC et al. assessed dietary compliance to GFD in 64 CD children and reported a higher dietary compliance in younger children (>80%) as compared to the adolescents (44%); children with higher maternal education; parents having a better knowledge and understanding of the disease; small families; patients having fewer siblings; and families with a higher per capita income [37]. Another study found that primary education and unemployment were related to a higher degree of stress; suggesting that a lesser knowledge of CD and its benign course could play a role and affect the QOL [47]. Small sized families with less than 6 members showed a higher QOL than the large-sized families [the fisher’s exact test=0.0799 and p=0.0123]. The higher QOL in smaller families may be attributed to the fact that small-sized families are able to focus more on the sick child and provide better care. Also; smaller-sized families are more capable in providing the expensive GFD.
Early detection of CD; prior to 4 years of age might help in complying with GFD [47]. However; the impact of early diagnosis of CD and the duration of illness on QOL is not consistent. Some studies found that children who were diagnosed before the age of five years scored better than those who were five years or older [12]. In contrast; the present study did not show any correlation between QOL score and the period between diagnosis and the participation in the study [the duration of illness] (r=0.109; p=0.356). This study finding is consistent with that of Paiva A et al. 2019 [11].
Poor QOL is expected in families with patients affected by multiple diseases other than CD. However; in the present study35 out of 73 patients (46.7 %) who reported other comorbidities including IDDM (60% of 35 patients) showed no correlation between QOL and co- morbidities (Fisher’s Exact Test=0.74; p=0.067).
Conclusion
During the present study; it was observed that the QOL of pediatric CD patients might vary from one country to another and is affected by factors like the QOL-instrument used (generic or CD specific); time of study in relation to diagnosis i.e.; prior to diagnosis; or after confirming the diagnosis; after initiation of GFD; and the variables investigated.
Our study found that QOL of caregivers in pediatric medicine is important and observed to be good. Small-sized families and young and educated mothers have a better QOL than others. Most of the emotional and psychosocial elements of QOL are related to the difficulties in availability of GFD in daily life.
Recommendation
Governmental Food and Drug Organizations should be committed to make GFF available at restaurants; coffee shops; in schools with snacks suitable for different age group; in supermarkets with reasonable price and proper labeling of commercially available food products; and in local bakeries.
Source of Funding
This research did not receive any specific grant from funding agencies in the public; commercial; or not for- profit sectors.
Conflict of interest
The Authors declare that there is no conflict of interest in conducting this research.
Ethics approval
Ethical approval obtained from KAIMRC (King Abdullah International Medical Research Centre)
IRB NCBE registration #H-01-R-005 Study #RA 17/018/A Date 11-January-2018
Acknowledgement
The authors would like to acknowledge Dr. Thilagavathy Ganapathy; Assistant professor in Nursing for her work in the proposal and Dr. Falah Al shammeri; paediatric resident for his co-operation in questionnaire distribution. The authors would also like to thank Mrs. Seham Khashwayn; for her statistical review.
Author’s contributions
All authors testify that they are qualified for authorship and have checked the article for plagiarism.
Samia Saud Al Furaikh (1st author) conceived and designed the study; written the proposal and the initial draft of manuscript; provided research materials and logistics support.
Amel Abouelfettoh (2nd author & corresponding author) validated survey tool; conducted statistics review; analysed; interpreted data and reviewed initial draft.
Manal Al Shehri (3rd author) conducted the survey; provided literatures review; supervised the research assistance in collecting data and taking consent and written the introduction of the article. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
References
- Hill ID; Dirks MH; Liptak GS; et al. Guideline for the diagnosis and treatment of celiac disease in children: recommendations of the North American society for pediatric gastroenterology; hepatology and nutrition. J Pediatr Gastroenterol Nutr. 40: 1-19 (2005).
- Mustalahti K; Catassi C; Reunanen A; et al. The prevalence of celiac disease in Europe: results of a centralized; international mass screening project. Ann Med. 42: 587-595 (2010).
- Wu J; Xia B; von Blomberg BME; et al. Coeliac disease: emerging in China? Gut. 59: 418-419 (2010).
- Makharia GK; Verma AK; Amarchand R; et al. Prevalence of celiac disease in the northern part of India: a community based study. J Gastroenterol Hepatol. 26: 894-900 (2011).
- Greco L; Timpone L; Abkari A; et al. Burden of celiac disease in the Mediterranean area. World J Gastroenterol. 17: 4971-4978 (2011).
- Attas RAA. How common is celiac disease in Eastern Saudi Arabia? Ann Saudi Med. 22: 315-319 (2002).
- Khayyat Y. Serologic markers of gluten sensitivity in a healthy population from the western region of Saudi Arabia. Saudi J Gastroenterol. 18: 23-25 (2012).
- Aljebreen AM; Almadi MA; Alhammad A; et al. Seroprevalence of celiac disease among healthy adolescents in Saudi Arabia. World J Gastroenterol. 19: 2374-2378 (2013).
- Sansotta N; Amirikian K; Guandalini S; et al. Celiac disease symptom resolution: effectiveness of the gluten-free diet. J Pediatr Gastroenterol Nutr. 66: 48-52 (2018).
- Samasca G; Sur G; Lupan I; et al. Gluten-free diet and quality of life in celiac disease. Gastroenterol Hepatol Bed Bench. 7: 139-143 (2014).
- Abreu Paiva LM; Gandolfi L; Pratesi R; et al. Measuring quality of life in parents or caregivers of children and adolescents with celiac disease: development and content validation of the questionnaire. Nutrients. 11: 2302 (2019).
- Bystrom IM; Hollen E; Falth-Magnusson K; et al. Health-related quality of life in children and adolescents with celiac disease: from the perspectives of children and parents. Gastroenterol Res Pract. 2012: 1-6 (2012).
- Dorn SD; Hernandez L; Minaya MT; et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment Pharmacol Ther. 31: 666-675 (2010).
- Wolf RL; Lebwohl B; Lee AR; et al. Hypervigilance to a gluten-free diet and decreased quality of life in teenagers and adults with celiac disease. Dig Dis Sci. 63: 1438-1448 (2018).
- World Health Organization. The first ten years of the world health organization. Geneva: World Health Organization: (1958).
- World Health Organization. Division of mental H. programme on mental health. Geneva: World Health Organization: (1996).
- Patrick DLaE; Pennifer. Health status and health policy: quality of life in health care evaluation and resource allocation. New York Oxford University Press: (1993).
- Takahashi A; Moriya K; Ohira H; et al. Health-related quality of life in patients with autoimmune hepatitis: A questionnaire survey. PLoS One. 13: e0204772 (2018).
- Knowles SR; Graff LA; Wilding H; et al. Quality of life in inflammatory bowel disease: A systematic review and meta-analyses-part I. Inflamm Bowel Dis. 24: 742-751 (2018).
- Varni JW; Shulman RJ; Self MM; et al. Gastrointestinal symptoms predictors of health-related quality of life in pediatric patients with functional gastrointestinal disorders. Qual Life Res. 26: 1015-1025 (2017).
- Harnett JE; Myers SP. Quality of life in people with ongoing symptoms of coeliac disease despite adherence to a strict gluten-free diet. Sci Rep. 10: 1144 (2020).
- Casellas F; Rodrigo L; Vivancos JL; et al. Factors that impact health-related quality of life in adults with celiac disease: a multicenter study. World J Gastroenterol. 14: 46-52 (2008).
- Violato M; Gray A. The impact of diagnosis on health-related quality of life in people with coeliac disease: A UK population-based longitudinal perspective. BMC Gastroenterol. 19: 68 (2019).
- Nachman F; Maurino E; Vazquez H; et al. Quality of life in celiac disease patients: prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment. Dig Liver Dis. 41: 15-25 (2009).
- Mustalahti K; Lohiniemi S; Collin P; et al. Gluten-free diet and quality of life in patients with screen-detected celiac disease. Eff Clin Pract. 5: 105-113 (2002).
- Hopman EG; Koopman HM; Wit JM; et al. Dietary compliance and health-related quality of life in patients with coeliac disease. Eur J Gastroenterol Hepatol. 21: 1056-1061 (2009).
- de Lorenzo CM; Xikota JC; Wayhs MC; et al. Evaluation of the quality of life of children with celiac disease and their parents: a case-control study. Qual Life Res. 21: 77-85 (2012).
- Kolsteren MM; Koopman HM; Schalekamp G; et al. Health-related quality of life in children with celiac disease. J Pediatr. 138: 593-595 (2001).
- Ljungman G; Myrdal U. Compliance in teenagers with coeliac disease-A Swedish follow-up study. Acta Paediatr. 82: 235-238 (1993).
- Burger JPW; van Middendorp H; Drenth JPH; et al. How to best measure quality of life in coeliac disease? A validation and comparison of disease-specific and generic quality of life measures. Eur J Gastroenterol Hepatol. 31: 941-947 (2019).
- Jordan NE; Li Y; Magrini D; et al. Development and validation of a celiac disease quality of life instrument for North American children. J Pediatr Gastroenterol Nutr. 57: 477-486 (2013).
- van Doorn RK; Winkler LM; Zwinderman KH; et al. CDDUX: A disease specific health-related quality-of-life questionnaire for children with celiac disease. J Pediatr Gastroenterol Nutr. 47: 147-152 (2008).
- van Koppen EJ; Schweizer JJ; Csizmadia CG; et al. Long-term health and quality-of-life consequences of mass screening for childhood celiac disease: a 10-year follow-up study. Pediatrics. 123: e582-588 (2009).
- Hauser W; Gold J; Stein J; et al. Health-related quality of life in adult coeliac disease in Germany: results of a national survey. Eur J Gastroenterol Hepatol. 18: 747-754 (2006).
- Deepak C; Berry N; Vaiphei K; et al. Quality of life in celiac disease and the effect of gluten-free diet. JGH Open. 2: 124-128 (2018).
- Chellan D; Muktesh G; Vaiphei K; et al. Effect of gluten-free diet and compliance on quality of life in pediatric celiac disease patients. JGH open. 3: 388-393 (2019).
- Chauhan JC; Kumar P; Dutta AK; et al. Assessment of dietary compliance to gluten free diet and psychosocial problems in Indian children with celiac disease. Indian J Pediatr. 77: 649-654 (2010).
- Al Nofaie ND; Al Ahmadi JR; Saadah OI. Health related quality of life among Saudi children and adolescents with celiac disease. Saudi J Gastroenterol. 26: 26-31 (2020).
- Eiser C; Morse R. Can parents rate their child's health-related quality of life? Results of a systematic review. Qual Life Res. 10: 347-357 (2001).
- Theunissen NC; Vogels TG; Koopman HM; et al. The proxy problem: child report versus parent report in health-related quality of life research. Qual Life Res. 7: 387-397 (1998).
- Collins LG; Swartz K. Caregiver care. Am Fam Physician. 83: 1309-1317 (2011).
- Skjerning H; Mahony RO; Husby S; et al. Health-related quality of life in children and adolescents with celiac disease: patient-driven data from focus group interviews. Qual Life Res. 23: 1883-1894 (2014).
- Barratt SM; Leeds JS; Sanders DS. Quality of life in Coeliac Disease is determined by perceived degree of difficulty adhering to a gluten-free diet; not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis. 20: 241-245 (2011).
- Sarkhy AA; El Mouzan MI; Saeed E; et al. Clinical characteristics of celiac disease and dietary adherence to gluten-free diet among saudi children. Pediatr Gastroenterol Hepatol Nutr. 18: 23-29 (2015).
- Altobelli E; Paduano R; Gentile T; et al. Health-related quality of life in children and adolescents with celiac disease: survey of a population from central Italy. Health Qual Life Outcomes. 11: 204 (2013).
- Ferretti F; Federica B; Dell Osso B; et al. Coping with celiac disease: how heavy is the burden for caregivers? Spanish J Dig Dis. 109: 250-255 (2017).
- Hogberg L; Grodzinsky E; Stenhammar L. Better dietary compliance in patients with coeliac disease diagnosed in early childhood. Scand J Gastroenterol. 38: 751-754 (2003).