Case Series - Interventional Cardiology (2021) Volume 13, Issue 2
Radial Access in CHIP: A Case Series
- Corresponding Author:
- Refai Showkathali
Department of Cardiology, Apollo Main Hospital, Greams Road, Chennai, India,
E-mail: refais@gmail.com
Received date: December 01, 2020 Accepted date: January 07, 2021 Published date: January 14, 2021
Abstract
Complex high-risk and indicated percutaneous coronary intervention (CHIP) offers effective management in high-risk coronary artery disease (CAD). We describe 3 cases of complex CAD successfully treated by CHIP using radial access. Use of 7F Glidesheath Slender® (GSS) offered an added advantage of better sheath to artery ratio and gave enough support to deliver devices in these patients with complex anatomy.
Keywords
Coronary artery disease • Percutaneous coronary intervention •Arteries •Complex anatomy
Abbreviations
CAD: Coronary Artery Disease; CAG: Coronary Angiogram; CHIP: Complex High-risk and Indicated Percutaneous coronary intervention; CTO: Chronic Total Occlusion; Cx: Circumflex; DES: Drug Eluting Stent; GSS: Glide-Sheath Slender; IABP: Intra-Aortic Balloon Pump; LAD: Left Anterior Descending; LCA: Left Coronary Artery; LCX: Left Circumflex; LIMA: Left Internal Mammary Artery; LM: Left Main; LMCA: Left Main Coronary Artery; OCT: Optical Coherence Tomography; OM: Obtuse Marginal; PCI: Per Cutaneous Intervention; RCA: Right Coronary Artery; RRA: Right Radial Artery; SVG: Saphenous Vein Graft
Introduction
Patients with complex Coronary Artery Disease (CAD) and significant comorbidities are challenging to treat and are inoperable or deemed high risk for conventional Percutaneous Coronary Intervention (PCI). Conventional PCI in these patients is often inappropriate due to technical limitations or a perceived lack of benefit [1]. However, high-risk patients frequently respond well to revascularization despite inherent associated risks [2]. Complex high-risk and indicated PCI (CHIP) offers significant improvement in symptoms and improved survival with fewer re-hospitalizations [3]. Considering the complex anatomy, most operators use femoral access as default strategy. Although clinical trials have primarily assessed pharmacological strategies for reducing bleeding risk, there is a mounting body of evidence suggesting that adoption of a transradial rather than a transfemoral approach to PCI may permit greater reductions in bleeding risk than have been achieved with pharmacological strategies alone [4]. However, with newer devices (mother and child catheter, sheathless guiding catheters, low profile radial sheaths etc.) and improved technical skills of operators, more CHIP are performed radially. Here we describe 3 cases of complex CAD successfully managed by CHIP using radial access, with the help of 7F Glidesheath Slender® (Terumo, Tokyo, Japan) referred hereafter as GSS.
Case 1
Transradial CHIP in severe Left Ventricular (LV) dysfunction
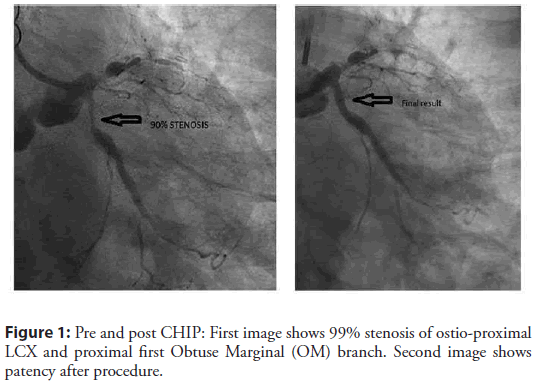
A 69-year-old man with diabetes, hypertension and history of CAD treated with 3 grafts (Left Internal Mammary Artery [LIMA] to second diagonal [D2], saphenous vein graft [SVG] to Left Coronary Artery [LAD] and Right Coronary Artery [RCA] in 2013) was admitted with chest discomfort, breathlessness, and sweating. Electrocardiogram showed left bundle branch block and echocardiogram showed global hypokinesia of LV with accentuated hypokinesia of antero-lateral segments with 40% ejection fraction. Coronary Angiogram (CAG) demonstrated progression of native triple vessel disease with patent grafts (Figure 1). The heart team decided to optimize his medications and avoid further intervention. During hospitalization, he experienced one more episode of chest discomfort with dynamic electrocardiogram changes involving lateral territory. Therefore CHIP to native circumflex (Cx) artery was planned with standby Intra-Aortic Balloon Pump (IABP).
Figure 1: Pre and post CHIP: First image shows 99% stenosis of ostio-proximal LCX and proximal first Obtuse Marginal (OM) branch. Second image shows patency after procedure.
A 7F GSS was inserted through the Right Radial Artery (RRA), and XB 3.0 guide catheter was used to engage the Left Coronary Artery (LCA). BMW guidewire (Balance Middle Weight, Guidant Corporation) was used to cross the Left Circumflex (LCX) lesion. Predilation was performed using 2.0 × 10 mm balloon at 16 atmospheres, following which the patient had bradycardia, hypotension, and sustained cardiac arrest. Return of spontaneous circulation was achieved with 2 cycles of cardiopulmonary resuscitation, but BP remained low at 85/50 mm Hg. An IABP was inserted via right femoral access. The patient was stabilized, and proximal LCX was stented with 3.5 × 22 mm Resolute Onyx™ (Medtronic Inc., Santa Rosa, CA, USA) stent. IABP was removed after 24 hours and he was discharged after 72 hours. A 2-week follow-up revealed good improvement in quality of life with no symptoms.
Case 2
Radial Chronic Total Occlusion (CTO) PCI
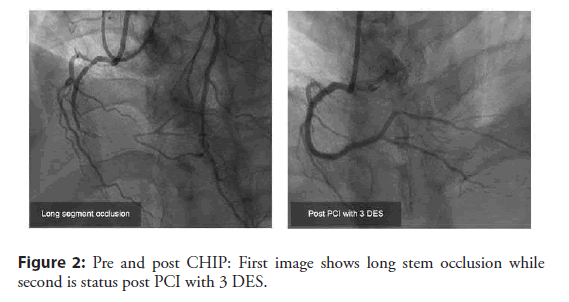
A 34-year-old man with exertional chest pain underwent treadmill test that was positive with ST depression at stage III. CAG at another hospital showed CTO of distal RCA. There was retrograde collateral from the left system up to the crux of RCA. He was referred to our Institute after an unsuccessful attempt to open CTO in the same hospital. PCI to RCA CTO via radial approach was planned. A 7F GSS was inserted via RRA, and a 6F sheath was inserted in the left radial artery. A 7F JR 3.5 guiding catheter was used to intubate RCA, and a 6F EBU 3.5 guide catheter was used to intubate left main coronary artery (LMCA) for retrograde injection. Bilateral injection showed a long CTO segment (>20 mm) with a JCTO (the Japanese-CTO) score of 2. Antegrade wire escalation technique was used with corsair microcatheter support. Gaia I wire crossed the occlusion and was parked in the distal vessel. After pre-dilation with a 2.5 × 15 mm balloon, 2 long stents (2 × 30 mm Resolute Onyx™ and 2.5 × 38 mm Resolute Onyx™ ) were deployed from distal to proximal segment, and a 3.5 × 15 mm Xience Xpedition™ (Abbott Vascular, Santa Clara, CA, USA) DES was deployed at the proximal RCA with good final result (Figure 2). The patient was discharged in 24 hours and recovered well during 1-month follow-up.
Case 3
Transradial rotablation (Optical Coherence Tomography [OCT] guided)
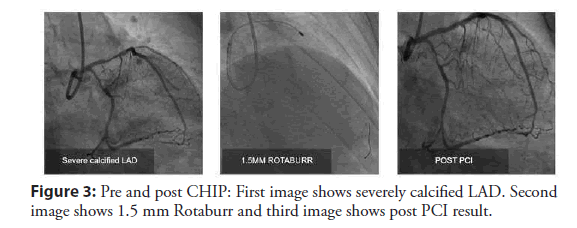
A 64-year-old man with diabetes and hypertension presented with chronic stable angina. Echo showed normal LV function, while CAG revealed calcified coronaries with severe LAD, borderline LCX, and RCA disease. A 7F GSS was inserted in RRA and the left Main (LM) was intubated with EBU 3.5 guide catheter. Run through® NS wire (Terumo, Tokyo, Japan) was used to cross the lesion. OCT pullback showed concentric calcification of proximal LAD. Rotablation was performed using a 1.5 mm burr at 1,75,000 rpm, pre-dilated with 2.5 × 12 mm balloon and deployed 2.75 × 28 mm Xience Xpedition™ DES at 10 atm (Figure 3). Post dilation was performed with a 2.75 × 8 mm balloon.
Results and Discussion
Use of GSS offered an added advantage of better sheath to artery ratio and gave enough support to deliver devices in these patients with complex anatomy. 7F GSS has remarkably changed the practice of CHIP, including CTO PCI, and has shown high procedural success (~97%) in complex coronary interventions such as LM disease, complex bifurcation stenting, CTO and rotational atherectomy [5]. This sheath has the outer diameter smaller than the other sheaths but can accommodate large catheters and, hence, is a preferred choice for PCI through radial access. 7Fr GSS shows low rates of vascular access-site complications, including radial artery occlusion and can be used in small radial arteries without the risk of severe spasm. To summarize, patients with complex CAD can be successfully treated with an appropriate choice of procedure and equipment using radial access [6].
Conclusion
Radial access in CHIP gives successful results even in patients with complex anatomy. Femoral access widely used as a default technique in such cases can be modulated to radial approach using the newer available devices. Transradial access has become an interesting approach for percutaneous coronary intervention, mainly because of reduced rates of bleeding complications compared to the transfemoral approach. The use of radial artery access and the TR Band Compression Device makes the practice of same day discharge feasible as well in clinical practice.
Conflict of Interest
Author declares no conflict of interest.
Acknowledgement
The authors express their appreciation to CBCC Global Research for manuscript writing and editorial assistance which was funded by Terumo, India.
References
- Iftikhar SF, Hu P. Complex Coronary Artery Lesions. (2019).
- Baumann S, Werner N, Ibrahim K, et al. Indication and short-term clinical outcomes of high-risk percutaneous coronary intervention with microaxial Impella® pump: Results from the German Impella® registry. Clin Res Cardiol. 107(8): 653-657 (2018).
- Kübler P, Zimoch W, Kosowski M, et al. The use of rotational atherectomy in high-risk patients: results from a high- volume centre. Kardiol Pol. 76(9): 1360-1368 (2018).
- Rao SV, Cohen MG, Kandzari DE, et al. "The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions." J Am Coll Cardiol. 55(20): 2187-2195 (2010).
- Aminian A, Iglesias JF, Van Mieghem C, et al. First prospective multicenter experience with the 7 French Glidesheath slender for complex transradial coronary interventions. Catheter Cardiovasc Interv. 89(6): 1014- 1020 (2017).
- Tomassini, Francesco, et al. "Is percutaneous coronary intervention of unprotected left main coronary artery via transradial approach feasible for skilled transfemoral operators? Initial experience in an unselected population." Cardiovasc Revasc Med. 14(4): 193-196 (2013).