Research Article - Interventional Cardiology (2018) Volume 10, Issue 3
Radiation exposure in a group of interventional cardiologists in a high volume PCIcenter
- Corresponding Author:
- Julio Cesar Rodriguez Goyes
Clínica Las Americas Medellín, Colombia
Tel: +57(4) 3421010
E-mail: Julliusc@yahoo.com.mx
Abstract
Aims: To demonstrate differences in radiation doses between radial/femoral approach during cardiac catheterization. To increase awareness about ionizing radiation risks in the cath lab. Methods: We measured radiation exposure in a group of interventional cardiologists between July and August 2017 in a high volume PCI-center during 89 procedures. Four calibrated crystals (TLD 100) 3 × 3 × 0.89 mm were used to measure radiation: one in the middle of each ciliary region (crystalline exposition), thyroid (external to leaded protector) and chest (internal to the leaded apron). They were stored and transported in leaded containers to avoid contamination. They were analyzed daily with stimulated thermo-luminescence. Results: Median fluoroscopy time was 4.24 minutes (IR 5.62) for radial access versus 6.02 minutes (IR 9.15) for femoral access (P=0.137). The median mSv in the entire body was 0.060 mSv when access was radial vs. 0.054 msV when access was femoral (p=0.949). Conclusions: Femoral access was related with less radiation exposure in the past. Nowadays, radial access procedures are faster resulting on similar radiation exposure. Radial route could be more appropriate since it entails fewer complications for patients. This study measures crystalline dosimetry in front rather than laterally as most studies do, which undermines the real dose.
Keywords
Radiation exposure; Interventional cardiology; Coronary Artery and Grafting
Abbreviations
USA: United States of America; mSv: Milisievert; ACC: American College of Cardiology; SOLACI: Sociedad Latinoamericana de Cardiología Intervencionista – Latin-American Society of Interventional Cardiology; CABG: Coronary Artery Bypasses Grafting
Introduction
Interventional cardiology is the medical field in which operators are exposed to the highest ionizing radiation doses, compared with interventional radiologists or neuroradiologists [1]. In the USA, cardiologists represent 45% of the total cumulative effective dose of 3.0 mSV per person per year (equivalent to the radiation from 150 chest X-rays) from all sources except radiotherapy [2].
Ionizing radiation may cause lesions in humans and animals such as dermatitis, alopecia, cataracts, retinal damage, burns and cancer. The most frequent malignant tumors related to ionizing radiation are brain, thyroid and skin cancer [3]. There is a concerning lack of adherence by interventional cardiologists to the use of protective equipment to reduce the effects of ionizing radiation. One study in Lithuania [4] showed that the lead thyroid collar, protective screen and leaded glasses were used in 93.5%, 83.9% and 35.5% of the cases, respectively. Many developing countries do not provide training on radioprotection topics at universities and health institutions where trainees rotate, and there is a lack of control and legislation from political parties, regulatory institutions and health centers to obligate these professionals to use the adequate radiological protection. In some cath labs a lead head protector has never been used.
Radiological protective equipment may be underused due to a lack of knowledge on this topic and/or the discomfort of wearing the equipment. Also, the average elapsed time before developing a neoplasia in professionals exposed to ionizing radiation may be too long, thus inducing a sense of calm and comfort. In their article, Roguin et al. [5] showed that a period of 12 to 32 years (average of 22 years) is needed to develop brain cancer in people occupationally exposed to ionizing radiation.
Industrialized countries have led the way in regulating topics regarding ionizing radiation such as occupational exposure doses and exposure monitoring and regulation for workers, among others. Examples of the above are: The Euratom Law from Europe, the referral guidelines for medical imaging from the European Commission, the American National Academy of Biological Sciences with its committee on biological studies on ionizing radiation (2006), the International Commission on Radiological Protection (2007), and the United Nations Scientific Committee on the Effects of Atomic Radiation (2008) [2].
In 2005, the American College of Cardiology (ACC) issued its interventional cardiology guidelines and emphasized the responsibility of all doctors to minimize procedural radiation-induced damages for their patients, their coworkers and themselves [6]. In 2009, the science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and the Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention issued the recommended doses for common exams in cardiology [7]. In 2010, the ACC disclosed the need for a proper and optimal use of radiological techniques in cardiology [8]. The Food and Drug Administration (FDA), in 2010, launched the initiative for reducing unnecessary radiation during medical tests [9].
One interesting Latin American publication is the article by Dr. Ariel Durán, who conducted a very innovative study evaluating 117 professionals during the 2011 SOLACI Congress. He took 99 exposed individuals and compared them against 18 nonexposed controls [10]. He found radiation-induced ocular pathology in 47% of the exposed population compared with 17% of those not exposed. Another study with a similar methodology analyzed doctors from Colombia, Uruguay and Malaysia and studied the risk of developing cataracts after occupational radiation exposure [11].
Methods
We measured the radiation exposure in a group of interventional cardiologists (three in total) who were well trained in radial access, between July and August 2017, at a high volume PCI-center (Clínica Las Américas, Medellín, Antioquia, Colombia) with standardized use of radiation protection methods, for a total of 89 procedures (both diagnostic and therapeutic). They were evaluated consecutively, based on patient assignation, and they performed various procedures (diagnostic, therapeutic, right sided, coronary intervention, and CABG evaluation) using diverse routes of access (radial, femoral, brachial, and conversion of radial to brachial or radial to femoral). There were neither TAVR procedures nor endovascular treatment of aortic aneurysms in this study.
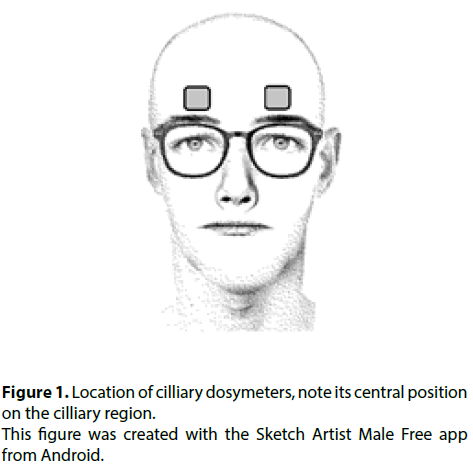
Four 3 × 3 × 0.89 mm crystals (TLD 100 LiF:MgTi) were used to measure radiation, calibrated before each measurement with metrological traceability. One was placed in the middle of each ciliary region (Figure 1), for indirect measurement of lens exposure, one on the thyroid (external to the leaded protector) and one on the chest (internal to the leaded apron). They were analyzed daily with stimulated thermoluminescence and afterwards underwent thermal treatment and were transported in leaded containers to avoid alteration in the measurements.
The angiography equipment was a Phillips ALLURA X-ray system. Quality control determined that its operation was correct, with satisfactory quality images (evaluated with the TOR CDR tool).
The radiological protection at the cath lab consisted of a lead protective screen suspended in the air and a table curtain. All professionals always used the leaded apron and thyroid collar. Two cardiologists used protective eyewear all the time and one of them did not use lead glasses because he deemed them uncomfortable.
The crystals had a measurement range of 10 pGy- 100Gy and a HARSHAW 3500 reader was used. The crystals were calibrated with metrological traceability. The TLD crystals were distributed in all cases in groups of three (packages).
Placing the dosimeters on the ciliary region (rather than the lateral orbital edge, external to the lateral canthus) provides a more reliable measurement because it is not influenced by the use of protective eyewear.
The crystals were thermally annealed with a maximum temperature of 400° C before using them for each measurement procedure. With this strategy, any residual information on the crystals was eliminated. The crystals were transported and stored in a leaded container, thus diminishing background radiation. After using the crystals for each procedure, they were stored again in the leaded container to diminish the “measurement fading” phenomenon. The crystals were read within a two-day span, including the dosimeters used for natural background. After each reading, the crystals underwent thermal annealing again.
Error propagation was calculated for all the dosimeters used in each measurement (three for the present study), reader sensitivity and the propagation of the calibration curve of the dosimeter-reading system.
Statistical methods
Continuous variables are expressed as mean (SD) or median (IQR). Categorical variables are expressed as percentages (%) and numerics. Distribution of continuous variables was tested by Shapiro wilk test. Continuous variables for two independent groups were compared by Student’s t test or Mann–Whitney U test depending on distribution pattern. All statistical tests were two-tailed, and p<0.05 was considered statistically significant. All analyses were carried out in SPSS (version 21).
Results
Eighty-nine measurements on three interventional cardiologists were included in the present study. Each measurement represented a patient procedure varying from diagnostic to therapeutic interventions, and also classified by access route (radial, brachial, femoral or a mixture).
The interventional cardiologists performing the procedures had significant experience in the field. The median length of experience was 20 years and their average age was 56 years (Table 1).
| Professional | Age (years) | Experience (years) as Interventional Cardiologist | Use of lead apron, thyroid collar | Use of eyewear | History of benign disease induced by radiation | History of malign disease induced by radiation |
|---|---|---|---|---|---|---|
| 1 | 61 | 22 | Always | No | No | No |
| 2 | 53 | 20 | Always | Always | Yes* | No |
| 3 | 56 | 19 | Always | Always | Yes* | No |
| Median | 56 | 20 | ||||
*Both professionals are affected by alopecia on their legs.
Table 1. Characteristics of the interventional cardiologists included in the study.
Table 2 depicts the frequency of the procedures based on the route of access; it also shows the mean fluoroscopy time (8.7 min) and the average radiation dose (0.054 mSv).
| Route | Number of procedures | Mean fluoroscopy time (min) | Average HP10 (mSv) |
|---|---|---|---|
| Brachial | 5 | 7.59 | 0.04 |
| Radial | 50 | 5.11 | 0.06 |
| Femoral | 30 | 7.3 | 0.07 |
| Radial to femoral | 3 | 12.19 | 0.04 |
| Radial to brachial | 1 | 11.35 | 0.06 |
| Total / Mean | 89 | 8.708 | 0.054 |
*Both professionals are affected by alopecia on their legs.
Table 2. Frequency of the different routes of access
Table 3 compares the radial vs. femoral approach, and also subclassifies each route according to whether the procedure was diagnostic, therapeutic or both. Median fluoroscopy time was 4.24 minutes (IR 5.62) for radial access versus 6.02 minutes (IR 9.15) for femoral access (p=0.137). The median mSv in the entire body was 0.06 mSv with radial access vs. 0.054 mSc with femoral access (p=0.949).
| Type of procedure | |||||
|---|---|---|---|---|---|
| Diagnostic | Therapeutic | Both | |||
| Medium | Medium | Medium | |||
| Route of access | Radial | Fluoroscopy time (min) | 4.99 | 4.73 | 6.84 |
| Kerma – Area Product (mGy*cm2) | 44045 | 37294 | 59815 | ||
| Right mean (HP(3)) (mSv) | 0.117 | 0.124 | 0.135 | ||
| Left mean (HP(3)) (mSv) | 0.153 | 0.150 | 0.165 | ||
| Average (HP(10)) (mSv) | 0.061 | 0.065 | 0.061 | ||
| Thyroid | 0.143 | 0.146 | 0.115 | ||
| HP (10) | 0.059 | 0.062 | 0.057 | ||
| Femoral | Fluoroscopy time (min) | 7.03 | 10.40 | 8.01 | |
| Kerma – Area Product (mGy*cm2) | 57379 | 43304 | 46546 | ||
| Right mean (HP(3)) (mSv) | 0.142 | 0.135 | 0.128 | ||
| Left mean (HP(3)) (mSv) | 0.156 | 0.150 | 0.162 | ||
| Average (HP(10)) (mSv) | 0.080 | 0.048 | 0.054 | ||
| Thyroid | 0.136 | 0.105 | 0.119 | ||
| HP (10) | 0.074 | 0.046 | 0.052 | ||
Table 3. Detailed comparison of radiation exposure and procedure length when radial vs femoral approach used.
Discussion
The current study is justified by the importance of radiation exposure in interventional cardiology laboratories. This topic is getting more importance nowadays but there is still low awareness about it. It promotes unsafe practices by workers in the cath lab affecting both of them and to the patients.
There is low concern regarding protection and exposure to ionizing radiation, it may explain the low amount of research about this topic. In Latin America there are scarce number of publications and studies in this valuable field.
Recently the International Commission on Radiological Protection (ICRP) recommended a reduction in the annual dose limit for occupational exposure for the lens of the eye from 150 to 20 mSv, averaged over a period of 5 years, with the dose in a single year not exceeding 50 mSv.
The personal dose equivalent Hp [10] is now the internationally recommended operational quantity in the field of radiation protection by individual monitoring. It is the dose received by tissue (effective dose) at a 10 mm depth from the skin surface and is considered to be the dose to the whole body. The dose limit for workers proposed by the ICRP was established as an annual effective dose. An effective dose limit of 20 mSv each year has been set for persons employed in radiation work.
The interventional cardiologists participating in this study and the radiation protection department of Clínica Las Américas (Medellín, Antioquia, Colombia) proposed an evaluation of the radiation dose both in crystalline and in total body. The aim was to objectively measure the radiation dose in these professionals and to check whether it was under the international standard limits.
89 interventional procedures from different categories and routes of access where included in the study. Fluoroscopy time and radiation dose where measured in each procedure and specially there was a comparison between radial and femoral access. This is the first time that a study of this type is done in Clínica Las Américas.
In interventional cardiology procedures, is widely known that femoral access is related with a higher rate of complications such as: hematomas, arteriovenous fistulae, pseudoaneurysms and bleeding in the site of access. Femoral route is also associated with a longer postoperative recovery, more immobility while deccanulation is done and with longer transit of patients in the interventional cardiology department (especially in ambulatory procedures). For the entire above, radial access is preferred over femoral route, unless there is a contraindication to be used.
In the group of interventional cardiologists evaluated there is no an agreement about the radiation protection tools nor its mandatory use. One of them does not use eyewear protection due to uncomfort. Two of the three professionals routinely perform the procedures through radial access and the other one prefers the femoral route.
This study showed no significant difference on radiation dose or length of procedures among three interventional cardiologists when comparing radial vs. femoral access. This could let to suggest routine using of radial access supported also by many other advantages of this route discussed above. Increasing adherence to radiation protection tools, especially eyewear protection is critical. Professionals working in the cath lab must standardize the routine use of a protective screen to diminish cranial radiation and they may be advised to use a leaded protective cap.
Strengths and Limitations
This study shows that there is no significant difference in median fluoroscopy time (p 0.137) or radiation dose (p 0.949) between radial and femoral approaches in the cath lab.
The strengths of this study include a homogeneous group of interventional cardiologists with a similar length of experience in the field. They had good radial access skills which allowed them to perform the procedures in a reasonable amount of time, compared with femoral access. In the past there was evidence that the radial approach was linked to higher radiation exposure, but this could have been a consequence of the increased length of these procedures when radial access first began to be used worldwide. Over the past 20 years, the difference in fluoroscopy time between radial and femoral access has dropped significantly by almost 75% from 2 minutes in 1996 to 30 seconds in 2014 (p<0.0001) [12].
The study is limited by being observational, without randomization or control. One of the interventional cardiologists never used protective eyewear due to comfort issues, as was his usual practice. This may not have influenced the validity of the study because the medium and supra ciliary crystals were located in an area outside the range of the lead glasses. One interventional cardiologist usually preferred to perform the procedures through the femoral access, which may undermine the validity of these results. The data obtained could conceivably persuade him to use the radial access as his preferred route, given that there are fewer complications for the patient with this access (principally the length of time the patient spends in the cath lab, decannulation time and bleeding complications).
Conclusions
We found a similar fluoroscopy time and radiation dose after comparing radial vs femoral access during conventional procedures in the cath lab. These findings may be applied to those interventional cardiologists with good experience in radial access. Non-expert professionals may have a higher radiation dose due to a more lengthy procedure via the radial approach. The data obtained in this study may be used to favor the generalized use of radial access since this route is linked to a lower frequency and severity of patient complications, early patient mobilization and a faster transit time through the cath lab.
Impact on Daily Practice
The use of radial access instead of femoral access, when possible, may help to increase the economical productivity of cath labs due to a speedy rotation of patients and fewer patient complications related to the procedure. Patients may benefit because they are able to be mobilized early after a radial access procedure, they can be discharged faster, and they would be expected to have a shorter immobilization time, which is associated with fewer thromboembolic complications. Radial access is also linked to fewer bleeding complications.
Funding
No one
Conflict of interest statement
The authors have no conflict of interests to declare.
References
- Vaño E, González L, Guibelalde E, et al. Radiation exposure to medical staff in interventional and cardiac radiology. Br. J. Radiol. 71(849): 954-60 (1998).
- Picano E, Vano E. The Radiation Issue in Cardiology: the time for action is now. Cardiovasc Ultrasound. 9: 35 (2011).
- Ron E. Cancer risks from medical radiation. Health Phys. 85: 47–59 (2003).
- Zivile V, Martynas J, Inga C. Ionizing radiation exposure in interventional cardiology: current radiation protection practice of invasive cardiology operators in Lithuania. J Radiol Prot. 36: 695–708 (2016).
- Roguin A, Goldstein J, Bar O, et al. interventional procedures. Am J Cardiol.
- Brain and neck tumors among physicians performing 111:1368-1372 (2013).
- Hirshfeld JW, Balter S, Brinker JA, et al. ACCF/AHA/HRS/SCAI Clinical competence statement on physician knowledge to optimize patient safety and image quality in fluoroscopically guided invasive cardiovascular procedures: a report of the american college of cardiology foundation/american heart association/american college of physicians task force on clinical competence and training. Circulation. 111: 511-532 (2005).
- Gerber TC, Carr JJ, Arai AE, et al. Ionizing radiation in cardiac imaging: a science advisory from the American Heart Association Committee on Cardiac Imaging of the Council on Clinical Cardiology and Committee on Cardiovascular Imaging and Intervention of the Council on Cardiovascular Radiology and Intervention. Circulation. 119: 1056-65 (2009).
- Brindis R, Douglas PS: President’s page: The ACC encourages multipronged approach to radiation safety. J Am Coll Cardiol. 56: 522-4 (2010).
- Food and Drug Administration White Paper: Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging. Initiative to reduce unnecessary radiation exposure. [http://www.fda.gov/Radiation-EmittingProducts/RadiationSafety/RadiationDoseReduction/ucm199994.htm].
- Solaci. Nearly half of interventional cardiologists may have pre-cataract lesions | SOLACI. [online] Available at: http://solaci.org/en/2017/05/30/nearly-half-of-interventional-cardiologists-may-have-pre-cataract-lesions/ (2017)
- Kleiman N, Vano E, Duran A, et al. Risk for radiation cataract in Interventional Cardiology personnel. Invest Ophtalmol Vis Sci. 51: 4553 (2010).
- Plourde G, Pancholy S, Nolan J, et al. Radiation exposure in relation to the arterial access site used for diagnostic coronary angiography and percutaneous coronary intervention: a systematic review of the literature and meta-analysis. Lancet. 386(10009): 2192-203 (2015).