Review Article - Interventional Cardiology (2015) Volume 7, Issue 4
Recent advances in invasive coronary treatment strategies for out-ofhospital cardiac arrest: are they working?
Chain of survival in out-of-hospital cardiac arrest is improving and more patients are being admitted. Coronary disease is the leading cause of cardiac arrest. Patients return to consciousness after return of spontaneous circulation follow ESC/AHA guidelines on acute coronary syndrome management, but there is debate on how to approach comatose patients. There is consensus that the STEMI subgroup with shockable rhythm should be brought directly to the catheterization laboratory as they have acute coronary lesion in 90% of cases and expected survival of more than 50%. On the other hand, there is a big debate on whether patients without STEMI benefit from an early invasive approach as acute coronary lesion is found less frequently. Nonshockable first rhythm carries a much worse prognosis, and a less invasive strategy in this subgroup seems reasonable.
- Corresponding Author:
- Peter Radsel
Department of Intensive Internal Medicine,
University Medical Center Ljubljana, Zaloska 7, 1525 Ljubljana, Slovania
Tel: +386 1522 3182
E-mail: peter.radsel@mf.uni-lj.si
Abstract
Chain of survival in out-of-hospital cardiac arrest is improving and more patients are being admitted. Coronary disease is the leading cause of cardiac arrest. Patients return to consciousness after return of spontaneous circulation follow ESC/AHA guidelines on acute coronary syndrome management, but there is debate on how to approach comatose patients. There is consensus that the STEMI subgroup with shockable rhythm should be brought directly to the catheterization laboratory as they have acute coronary lesion in 90% of cases and expected survival of more than 50%. On the other hand, there is a big debate on whether patients without STEMI benefit from an early invasive approach as acute coronary lesion is found less frequently. Nonshockable first rhythm carries a much worse prognosis, and a less invasive strategy in this subgroup seems reasonable.
Keywords
acute coronary syndrome, cardiac arrest, coronary angiography, percutaneous coronary intervention
A case presentation
As an introduction and easier understanding of the topic discussed in the article, a case report is presented.
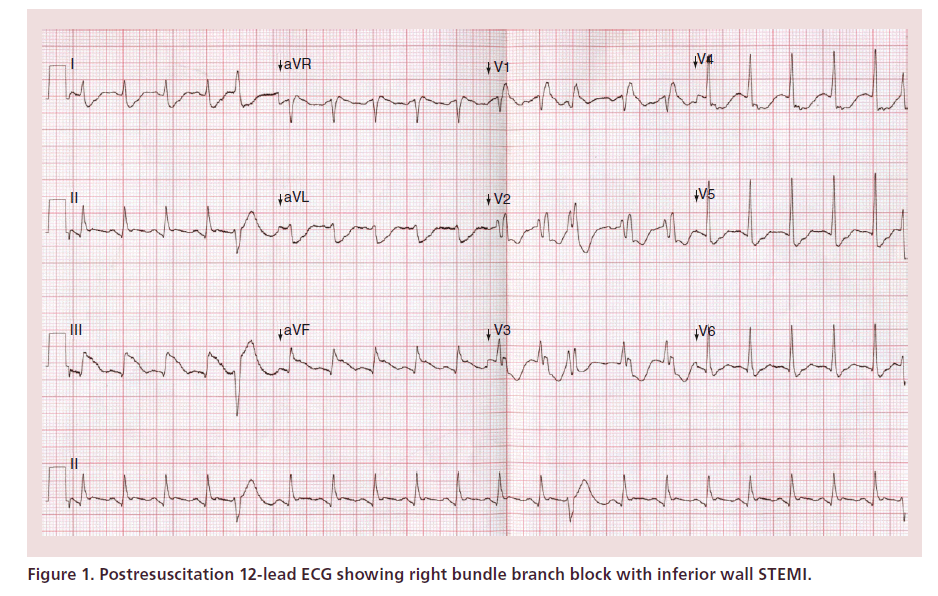
A 65-year-old female with known arterial hypertension and heart failure with preserved left ventricular function started complaining of chest pain and tiredness. She did not seek medical help but went for rest. 5 h later, she suddenly collapsed in front of her daughter without life signs. Basic life support was started. Emergency medical team arrived 7 min after collapse. Ventricular fibrillation was the first rhythm and second defibrillation was successful. First return of spontaneous circulation (ROSC) was achieved after 6 min. She remained comatose and was intubated. 8 min after ROSC polymorphic ventricular tachycardia occurred and synchronized cardioversion was needed. 12-lead ECG showed inferior wall STEMI (Figure 1). During transportation to 24/7 catheterization center, there was another ventricular fibrillation that was successfully terminated with a single shock.
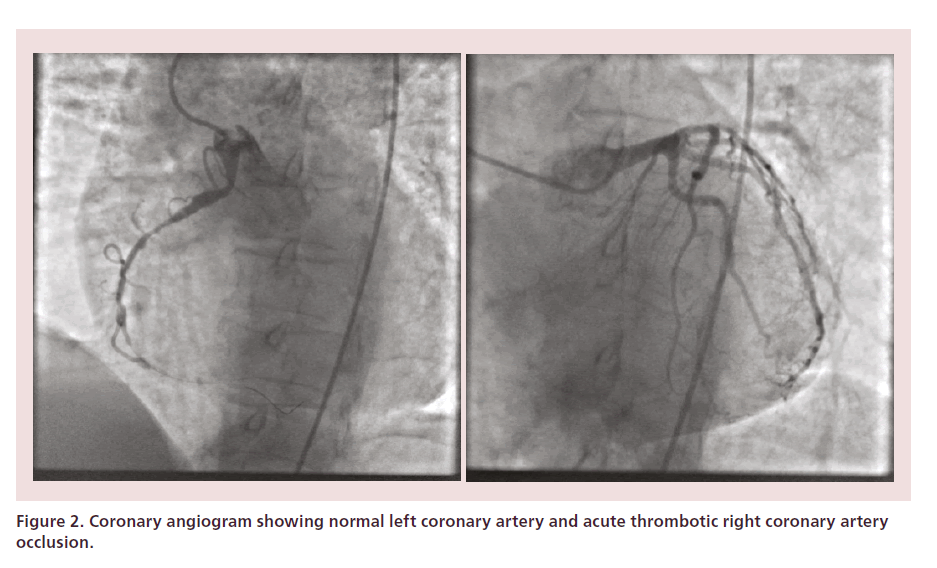
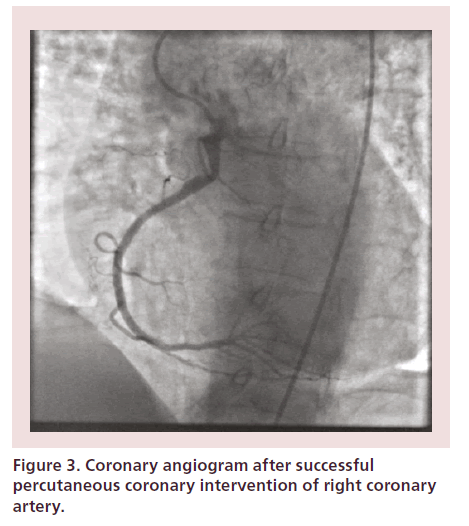
She was brought to emergency department (ER) as it was night time and interventional team was on call. At arrival to emergency department, her blood pressure was within normal limits but after minutes 3rd degree AV block with PEA occurred. ROSC was achieved after 3 min and 1 mg of adrenaline. Mild-induced hypothermia was initiated. After 15 min, she was taken to the catheterization lab. Urgent coronary angiography showed single vessel coronary disease with acute right coronary artery occlusion (Figure 2). Successful percutaneous coronary intervention was done with four drug-eluting stents implanted (Figure 3). After percutaneous coronary intervention, she was in sinus rhythm hemodynamically stable without the need for inotropic or vasopressor support. After completion of hypothermia, sedation was stopped and passive rewarming allowed. She regained consciousness on the 3rd day with cerebral performance category 2 and on the 5th day, her cerebral performance category was 1. She was discharged from the hospital on day 12.
Figure 2. Coronary angiogram showing normal left coronary artery and acute thrombotic right coronary artery occlusion.
Figure 3. Coronary angiogram after successful percutaneous coronary intervention of right coronary artery.
Dilemmas discussed in the article
Was there an indication for urgent coronary angiography, although the patient was comatose after ROSC?
Were recurrent cardiac arrests stopped due to immediate percutaneous intervention?
Was hospital treatment less complicated and shorter due to invasive approach?
Did invasive approach improve patient’s quality of life and prognosis?
Introduction
For almost two decades, data from autopsies and immediate coronary angiography (CAG) show that significant coronary artery disease (CAD) is present in more than 70% of patients suffering from out-of-hospital cardiac arrest (OHCA) [1,2]. Traditionally, the outcome of these patients was bad with the majority dying from postresuscitation brain injury and multiorgan failure [3]. Due to poor prognosis, treatment in intensive care units was usually conservative as invasive therapies seemed futile in a population with very high mortality. There were also no guidelines on invasive cardiac treatment as patients after OHCA were systematically excluded from all studies showing benefit of urgent CAG and percutaneous coronary intervention (PCI).
Gradually, approach known as ‘chain of survival’ grew stronger. Public education on cardiopulmonary resuscitation (CPR), use of automated external defibrillators and better postresuscitation care caused more patients not only to be admitted to hospitals but also surviving without major neurological deficit. Slowly more and more patients underwent early CAG and cardiac arrest-PCI (CA-PCI), which was found not only feasible [4,5] but also highly successful [6,7]. At first, those were patients with STEMI in 12-lead postresuscitation ECG followed later by patients without STEMI and no obvious noncoronary cause of cardiac arrest.
Immediate CAG
Despite the lack of randomized control trials showing benefit of immediate CAG and PCI in patients with resuscitated OHCA, the number of patients undergoing immediate invasive coronary approach slowly increased in time. Although patients after CA were excluded from studies showing superiority of PCI over thrombolysis knowledge derived from them was used in an attempt to improve prognosis [8]. At first, patients with STEMI in postresuscitation ECG were taken directly to the catheterization labs. Encouraging data from single center experiences [4,9–14] showing acute coronary syndrome (ACS) lesions in around 90% of STEMI patients and efficacy of PCI similar to ACS population without preceding OHCA resulted in decision to offer urgent CAG also to patients without STEMI but no noncoronary cause of cardiac arrest. Even in this population of patients, obstructive coronary artery disease is found in majority of them [1,15–17] and surprisingly ACS lesion in 25–58% [1,15–17]. Postresuscitation ECG can be difficult to interpret. Global ischemia, reperfusion injury, electrolyte and acid–base disturbances after OHCA can cause diffuse ECG changes that can hide regional ischemia seen in ACS. Predicting regional ischemia from post-ROSC ECG is not reliable as already Spaulding et al. in 1997 showed [1]. Post- ROSC ECG has a high-positive predictive value for acute coronary lesions (ACS lesion) but unfortunately low-negative predictive value [1,16].
Furthermore, studies have shown that urgent invasive strategy can be effectively combined with implementation of temperature control – mild-induced hypothermia, which is essential in preventing reperfusion brain injury in comatose survivors [5,18].
At present, there are almost 50 cohort studies published in the literature showing encouraging results of early invasive approach not only on survival but also on better neurological outcome [15,19–21]. Recent analysis which included almost 4000 patients from the USA showed early CAG and CA-PCI to be independently associated with survival and favorable neurological outcome [22].
At the moment, it seems unethical to perform a randomized control trial on OHCA victims with STEMI, but there is still ongoing debate whether to use invasive strategy in all non-STEMI patients. Due to higher heterogeneity of causes of OHCA, some centers postpone invasive diagnostics and perform CAG only in cases of neurological recovery. Others argue that urgent CAG can find acute culprit coronary lesions and by performing CA-PCI, we can further stabilize the patient and improve left ventricular systolic function. Normal coronary angiogram in their view should not be viewed as a negative invasive test but an additional stimulation in search of a noncoronary cause of cardiac arrest.
There is no clear answer in the literature which subgroups of patients after OHCA without STEMI will clearly benefit from PCI. Troponin is usually positive at admission due do global ischemia and gives no added value in predicting acute coronary lesion. There is not much data on urgent echocardiography in this setting.
In 2014, a consensus statement from European Association for Percutaneous Cardiovascular Interventions (EAPCI)/Stent for Life (SFL) groups on invasive coronary treatment strategies for OHCA was published [23]. It proposes a unified approach with recommendation for urgent CAG in all patients after OHCA. The only difference between STEMI and non-STEMI group is in an ‘emergency department stop’ where obvious noncoronary causes can be identified in no-STEMI population. ED stop is also advisable in patients who suffered head trauma during collapse to rule out intracranial pathology before possible use of anticoagulant and antiplatelet therapy during CA-PCI.
As already mentioned, coma cannot be a contraindication for immediate CAG as there is no reliable tool to select patients who will recover neurologically. Nevertheless, there are patients in whom aggressive treatment seems irrational. This includes patients with unwitnessed OHCA, with no BLS, initial nonshockable rhythm, long (>30 min) advanced life support and severe prearrest co-morbidities. A study was recently published showing benefit of aggressive strategy on survival only in patients with initial shockable rhythm [24].
Reperfusion strategy
Survival of patients who regain consciousness immediately after ROSC is even higher compared with STEMI population without preceding OHCA [4,16,21].
This can be partly explained by shorter ischemic times possibly due to shorter patient delay. Most clinicians agree treatment of these patients should follow general ACS guidelines with complete myocardial revascularization either percutaneous or surgical [25,26].
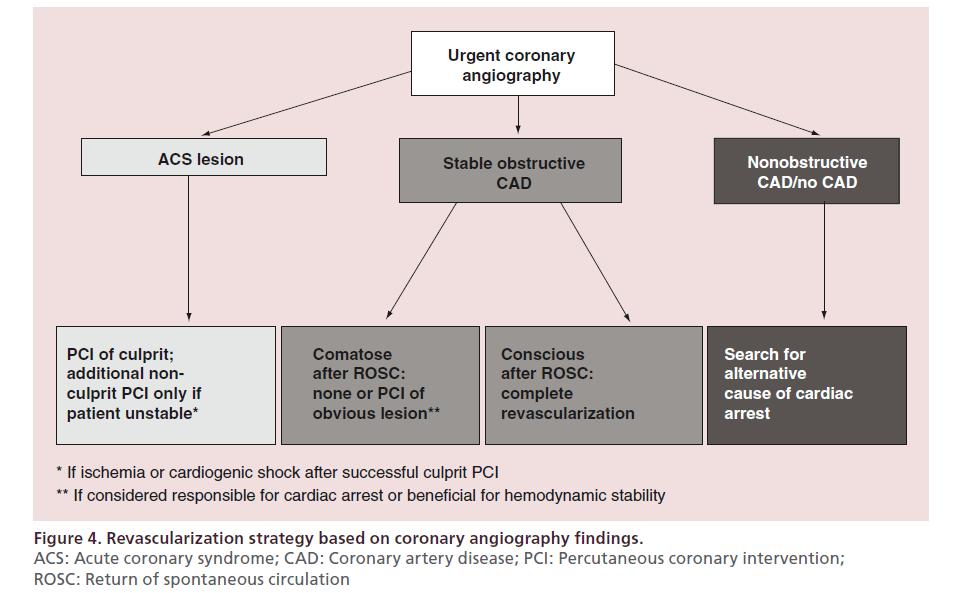
On the contrary in the comatose group, decision on revascularization strategy should depend on CAG findings (Figure 4). Basic rationale behind urgent invasive approach is revascularization of obvious culprit lesions that are not only triggers for OHCA but can cause further arrhythmias, hemodynamic instability and bigger myocardial infarction size if left untreated.
Figure 4. Revascularization strategy based on coronary angiography findings.
ACS: Acute coronary syndrome; CAD: Coronary artery disease; PCI: Percutaneous coronary intervention;
ROSC: Return of spontaneous circulation
PCI of stable obstructive lesions in comatose survivors should be postponed and done only in patients who neurologically recover. Especially in no-STEMI subgroup, CA-PCI of stable CAD may worsen patient’s condition as stable CAD may only be a ‘bystander’ in OHCA and the use of anticoagulant and antiplatelet therapy during and after CA-PCI can negatively influence other conditions responsible for OHCA (e.g., intracranial bleeding).
It seems that only patients with cardiogenic shock after ROSC benefit multivessel PCI as was showed in a study by Mylotte et al. in 2013 [27]. Early reperfusion results in smaller infarct size, less systemic inflammatory response and full revascularization can improve left ventricular systolic function. All these helps the patients to survive postresuscitation syndrome (sepsis- like syndrome) complicated by cardiogenic shock.
Routine use of intraaortic balloon pump in cardiogenic is not recommended [28] and there are also no data to prove survival benefit of other hemodynamically more potent devices.
PCI in no-ROSC
Sometimes we are faced with younger patients with recurrent cardiac arrest and/or even situations with unsuccessful resuscitation attempt. With the use of mechanical chest compression devices, these patients can be brought to PCI centers where attempts of further diagnostics and treatment can occur. In cases of proximal coronary occlusion or massive pulmonary embolism, mechanical interventions during CPR can lead to ROSC. Past data show relatively good survival, although we must appreciate that usually only successful cases are presented in the literature [29], therefore this approach cannot be recommended routinely. Nowadays, urgent insertion of venous–arterial ECMO or other mechanical ventricular support devices looks promising allowing us more time for urgent procedures without further increase in ischemic injury [30–32]. Optimal place for such demanding procedures is catheterization laboratory where x-ray guidance for cannula placement is helpful and immediate further therapy is possible.
Pre- & peri-procedural medical treatment
In cases where ACS is the trigger of OHCA, there is a need for CA-PCI with stenting and anticoagulation and antiplatelet therapy is needed. Again, it seems reasonable to use ACS guidelines for conscious patients [25,26]. For the comatose patient, there are no data from the literature. Expert opinion is that acetylsalicylic acid unfractionated heparin should generally be given after coronary artery assessment but can be also given prior to CAG in patients with STEMI [23]. This is based on the fact that patients after OHCA are at increased risk for bleeding due to chest compression and postcardiac arrest syndrome. P2Y12 inhibitors can only be given in crushed form via nasogastric tube after the decision for stenting is made. There are data that P2Y12 effect is significantly delayed not only for clopidogrel but also for prasugrel and ticagrelor [33,34]. Whether this causes more stent thrombosis is not known as studies show conflicting results [35,36]. There is evidence that GPIIb/ IIIa effectively suppresses platelet aggregation [33], but it is unknown if they should be routinely used to bridge delayed onset of P2Y12 effect.
Conclusion
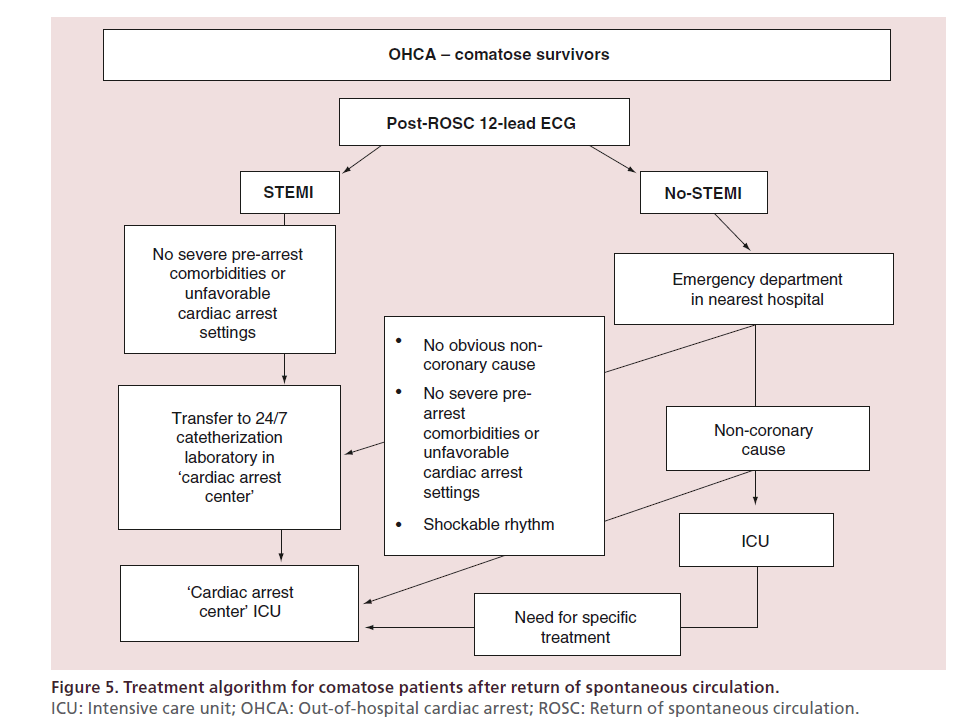
From nonrandomized cohort data, it seems that early coronary invasive approach works in majority of patients suffering from OHCA. There is no dilemma in diagnostic and treatment algorithms in conscious survivors. Different centers use different approach in comatose patients. In Figure 5, algorithm used in Ljubljana University Medical Center (tertiary 24/7 PCI center) is presented. We decide for immediate invasive coronary approach in majority of patients using well-established ‘STEMI fast track’ network.
Definitely not all comatose no-STEMI patients benefit from immediate CAG and CA-PCI. But at the moment, we do not have a reliable tool that would at patient’s presentation tell us neither whether there is definitely a coronary cause of OHCA nor whether neurological outcome will be good. Therefore, we do support immediate diagnostics in all patients without obvious noncoronary cause as we cannot deprive cause-related diagnostics and treatment in those patients who can benefit from CA-PCI and have chances of recovery. However, much more conservative is our decision making in revascularization strategy. We decide for CA-PCI only in clear culprit lesions and avoid ad hoc stable coronary artery revascularization.
There is tendency for centralization of treatment for OHCA victims as there are data showing better survival for patients treated in ‘cardiac arrest centers’ with the possibility of interventional procedures and extracorporeal circulation 24/7 [37,38]. However, there are cases where initial stabilization is needed in regional hospital’s ICU. After stabilization, transfer to PCI-capable hospital should not be delayed in patients with high likelihood of ACS. As already mentioned, acute thrombotic coronary occlusions are present even in patients with no- STEMI patients. This is quite common with LCX being culprit artery. Any unnecessary delay results in bigger infarction size and higher complication rate.
Future perspective
At present, many questions remain unsolved. We definitely need more data on patient selection for immediate CAG – not only quick noninvasive test to define probability of CAD, but also early neuroprognostication tools. Optimal reperfusion strategy remains unknown as there are no data on nonculprit obstructive lesions revascularization. Furthermore, we need more data on antiplatelet drug selection.
One of the most important unsolved dilemmas is patient selection for extracorporeal CPR, timing and devices to use.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
• Cohort studies show cardiac arrest-percutaneous coronary intervention to be not only successful in terms of good vessel patency but also as independent predictor of survival regardless of post-return of spontaneous circulation (ROSC) ECG.
• STEMI in post-ROSC ECG is highly specific for coronary artery occlusion and ‘STEMI networks’ can be used to bring the patients directly to catheterization laboratories.
• Patients without STEMI in post-ROSC ECG are a diverse group, therefore we should not rush with them directly to catheterization labs without stopping at emergency departments for basic investigation. But immediately after exclusion of major noncoronary causes of out-of-hospital cardiac arrest, we should perform coronary angiography and cardiac arrest-percutaneous coronary intervention if needed, especially in patients with shockable rhythm.
• Basic rationale behind urgent invasive approach is revascularization of obvious culprit lesions.
• Venous–arterial-ECMO can be used with no-ROSC patients if reversible cause is suspected.
References
Papers of special note have been highlighted as: • of interest
- Spaulding CM, Joly LM, Rosenberg A et al. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N. Engl. J. Med. 336, 1629–1633 (1997).
- Davies MJ. Anatomic features in victims of sudden coronary death: coronary artery pathology. Circulation 85(Suppl. I), I-19–I-24 (1992).
- Edgren E, Hedstrand U, Kelse YS, Sutton-Tyrrell K, Safar P. Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I study group. Lancet 30, 343(8905), 1055–1059 (1994).
- Gorjup V, Radsel P, Kocjancic ST, Ersen D, Noc M. Acute ST-elevation myocardial infarction after successful cardiopulmonary resuscitation. Resuscitation 72, 379–385 (2007).
- Knafelj R, Radsel P, Ploj T, Noc M. Primary percutaneous coronary intervention and mild induced hypothermia in comatose survivors of ventricular fibrillation with ST-elevation acute myocardial infarction. Resuscitation 74, 227–234 (2007).
- Sunde K, Pytte M, Jacobsen D et al. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation 73(1), 29–39 (2007).
- Garot P, Lefevre T, Eltchaninoff H et al. Six-month outcome of emergency percutaneous coronary intervention in resuscitated patients after cardiac arrest complicating ST-elevation myocardial infarction. Circulation 115, 1354–1362 (2007).
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet 361, 13–20 (2003).
- McCullough PA, Prakash R, Tobin KJ, O’Neil WW, Thompson RJ. Application of a cardiac arrest score in patients with sudden death and ST segment elevation for triage to angiography and intervention. J. Interven. Cardiol. 15, 257–261 (2002).
- Keelan PC, Bunch TJ, White RD, Packer DL, Holmes DR. Early direct coronary angioplasty in survivors of out-of-hospital cardiac arrest. Am. J. Cardiol. 91, 1461–1463 (2003).
- Marcusohn E, Roguin A, Sebbag A et al. Primary percutaneous coronary intervention after out-of-hospital cardiac arrest: patients and outcomes. Isr. Med. Assoc. J. 9, 257–259 (2007).
- Richling N, Herkner H, Holzer M, Riedmueller E, Sterz F, Schreiber W. Thrombolytic therapy vs primary percutaneous intervention after ventricular fibrillation cardiac arrest due to acute ST-segment elevation myocardial infarction and its effect on outcome. Am. J. Emerg. Med. 25, 545–550 (2007).
- Valente S, Lazzeri C, Saletti E, Chiostri M, Gensini GF. Primary percutaneous coronary intervention in comatose survivors of cardiac arrest with ST-elevation acute myocardial infarction: a single-center experience in Florence. J. Cardiovasc. Med. 9(11), 1083–1087 (2008).
- Mager A, Kornowski R, Murninkas D et al. Outcome of emergency percutaneous coronary intervention for acute ST-elevation myocardial infarction complicated by cardiac arrest. Coron. Artery Dis. 19(8), 615–618 (2008).
- Dumas F, Cariou A, Manzo-Silberman S et al. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest. Insights from the PROCAT registry. Circ. Cardiovasc. Interv. 3, 200–247 (2010).
- Radsel P, Knafelj R, Kocjancic S, Noc M. Angiographic characteristics of coronary disease and postresuscitation electrocardiograms in patients with aborted cardiac arrest outside a hospital. Am. J. Cardiol. 108, 634–638 (2011).
- Anyfantakis ZA, Baron G, Aubry P et al. Acute coronary angiographic findings in survivors of out-of-hospital cardiac arrest. Am. Heart J. 157, 312–318 (2009).
- Stub D, Hengel C, Chan W et al. Usefulness of cooling and coronary catheterization to improve survival in out-of-hospital cardiac arrest. Am. J. Cardiol. 107, 522–527 (2011).
- Reynolds JC, Callaway CW, El Khoudary SR, Moore CG, Alvarez RJ, Rittenberger JC. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. J. Intensive Care Med. 24(3), 179–186 (2009).
- Hosmane VR, Mustafa NG, Reddy VK et al. Survival and neurologic recovery in patients with ST-segment elevation myocardial infarction resuscitated from cardiac arrest. J. Am. Coll. Cardiol. 53, 409–415 (2009).
- Larsen JM, Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation 83, 1427–1433 (2012).
- Callaway CW, Schmicker RH, Brown SP et al. Early coronary angiography and induced hypothermia are associated with survival and functional recovery after out-of-hospital cardiac arrest. Resuscitation 85, 657–663 (2014).
- Noc M, Fajadet J, Lassen JF et al. Invasive coronary treatment strategies for out-of-hospital cardiac arrest: a consensus statement from the European association for percutaneous cardiovascular interventions (EAPCI)/stent for life (SFL) groups. EuroIntervention 10(1), 31–37 (2014).
- Kocjancic ST, Jazbec A, Noc M. Impact of intensified postresuscitation treatment on outcome of comatose survivors of out-of-hospital cardiac arrest according to initial rhythm. Resuscitation 85(10), 1364–1369 (2014).
- Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 33, 2569–2619 (2012).
- Hamm CW, Bassand JP, Agewall S et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 32, 2999–3054 (2011).
- Mylotte D, Morice MC, Eltchaninoff H et al. Primary percutaneous coronary intervention in patients with acute myocardial infarction, resuscitated cardiac arrest, and cardiogenic shock: the role of primary multivessel revascularization. JACC Cardiovasc. Interv. 6(2), 115–125 (2013).
- Thiele H, Zeymer U, Neumann FJ et al. Intra-aortic balloon support for myocardial infarction with cardiogenic shock. N. Engl. J. Med. 367, 1287–1296 (2012).
- Wagner H, Terkelsen CJ, Friberg H et al. Cardiac arrest in the catheterisation laboratory: a 5-year experience of using mechanical chest compressions to facilitate PCI during prolonged resuscitation efforts. Resuscitation 81(4), 383–387 (2010).
- Nagao K, Kikushima K, Watanabe K et al. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of-hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ. J. 74, 77–85 (2010).
- Kagawa E, Dote K, Kato M et al. Should we emergently revascularize occluded coronaries for cardiac arrest? Rapid response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation 126, 1605–1163 (2012).
- Mukku VK, Cai Q, Gilani S, Fujise K, Barbagelata A. Use of impella ventricular assist device in patients with severe coronary artery disease presenting with cardiac arrest. Int. J. Angiol. 21, 163–166 (2012).
- Steblovnik K, Blinc A, Bozic-Mijovski M, Kranjec I, Melkic E, Noc M. Platelet reactivity in comatose survivors of cardiac arrest undergoing percutaneous coronary intervention and hypothermia. EuroIntervention 7, pii:20131224–02 (2014).
- Ibrahim K, Christoph M, Schmeinck S et al. High rates of prasugrel and ticagrelor non-responder in patients treated with therapeutic hypothermia after cardiac arrest. Resuscitation 85, 649–656 (2014).
- Rosillo SO, Lopez-de-Sa E, Iniesta AM et al. Is therapeutic hypothermia a risk factor for stent thrombosis? J. Am. Coll. Cardiol. 63, 939–940 (2014).
- Joffre J, Varenne O, Bougouin W, Rosencher J, Mira JP, Cariou A. Stent thrombosis: an increased adverse event after angioplasty following resuscitated cardiac arrest. Resuscitation 85(6), 769–773 (2014).
- SØholm H, Wachtell K, Nielsen SL et al. Tertiary centres have improved survival compared with other hospitals in the Copenhagen area after out-of-hospital cardiac arrest. Resuscitation 84, 162–167 (2013).
- Sunde K. SOPs and the right hospitals to improve outcome after cardiac arrest. Best Pract. Res. Clin. Anaesthesiol. 27, 373–381 (2013).
• First report showing feasibility of coronary angiography (CAG) in victims of sudden cardiac arrest.
• This study reports feasibility of mild-induced hypothermia and urgent CAG combination in comatose survivors.
• Over 400 patients included and show positive effect of percutaneous coronary intervention (PCI) on survival in STEMI and no-STEMI population.
• Expert consensus that gives exact advices on indications and timing of CAG and PCI. Includes topics not included in resuscitation and ACS guidelines.
• Prospective study showing no benefit of intraaortic balloon pump in patients with cardiogenic shock.