Review Article - Imaging in Medicine (2009) Volume 1, Issue 1
Recent developments in coronary computed tomography imaging
Sebastian Leschka, Paul Stolzmann and Hatem Alkadhi†
Institute of Diagnostic Radiology, University Hospital Zurich, Raemistrasse 1008091, Zurich, Switzerland
- *Corresponding Author:
- Hatem Alkadhi
Institute of Diagnostic Radiology
University Hospital Zurich, Raemistrasse 1008091 Zurich
Switzerland
Tel: +41 442 551 111
Fax:+41 442 554 443
E-mail: hatem.alkadhi@usz.ch
Abstract
Keywords
computed tomography; coronary angiography; coronary artery disease; diagnostic accuracy; multislice technology; radiation dose; technical improvements; technological requirements
Technical requirements for cardiac computed tomography
Visualization of the heart and the coronary arteries has been of great interest for radiologists even in the early beginning of computed tomography (CT). In his novel prize lecture in 1979, Sir Godfrey N Hounsfield hypothesized on the future of CT for cardiac imaging [1]. Another 30 years of technical developments were required to achieve the current state of modern CT systems that are sufficiently robust and accurate for coronary imaging.
Coronary imaging requires the highest technical demands of any diagnostic modality because of the small size of the coronary arteries and the continuous motion during the cardiac cycle. Three major technical parameters define the capability of a CT system for imaging the coronary arteries: spatial resolution, temporal resolution and coverage speed in z‑axis direction.
Spatial resolution
A high spatial resolution is required for imaging and evaluation of small distal coronary artery segments and side branches. The spatial resolution depends on the physical width of the detector in a longitudinal direction. Ideally, isotropic voxel imaging should be achieved, which means that a voxel has the same size in all dimensions and is mandatory to reconstruct high-quality images in all planes. Current CT systems provide an isotropic spatial resolution of up to 0.4 mm. Further improved resolution at a level of 0.2 mm is desirable for a reliable evaluation of stent patency or severely calcified arteries [2]. However, a higher spatial resolution will require a higher radiation dose to maintain sufficient signal-to-noise ratio [2].
Temporal resolution
The temporal resolution depends on the gantry rotation time. A temporal resolution of less than 100 ms is desirable to allow artifact-free imaging of the coronary arteries even at elevated heart rates [2].
For reducing motion artifacts, the CT data acquisition is synchronized with the ECG signal. The most commonly used approach for synchronization is retrospective ECG gating in which images are acquired throughout the cardiac cycle and those time points depicting the coronary arteries without motion artifacts are retrospectively selected for image reconstruction.
The projection data of a half gantry rotation are than required for image reconstruction (halfscan reconstruction) and the temporal resolution is half of the rotation time. Thus, modern 64‑slice CT systems with a gantry rotation time of 330 ms have a temporal resolution of 165 ms. Further improvements in gantry rotation time are mandatory to achieve a temporal resolution of more than 100 ms when using a half-scan reconstruction method. However, the mechanical forces increase with higher gantry rotation times. Current CT systems with a gantry rotation time of 330 ms are associated with a mechanical force of approximately 28 g. Rotation times of less than 200 ms required for a temporal resolution in a mono-segmental halfscan reconstruction appear to be beyond today’s mechanical limits (i.e., >75 g) [2].
In addition, in order to compensate for motion artifacts at higher heart rates, two- or multisegment reconstruction algorithms are used that merge data from two or more consecutive heart beats for image reconstruction. This approach further improves temporal resolution at specific heart rates. However, its use is limited by artifacts occurring with variable heart rates, with inter-heart beat variability of the coronary artery position, and by the necessity of lower pitch factors prolonging the data acquisition time and increasing the radiation dose delivered to patients [3,4].
Another method to improve the diagnostic quality of CT coronary angiography (CTCA), although not achieved by improvements in CT technology, is demonstrated by heart rate and variability reductions using either an oral or intravenous b‑receptor antagonist [5–7].
Coverage speed in z‑axis
The coverage speed in z‑axis is inversely related to the longitudinal axis covered by the detector array, the gantry rotation speed and the pitch. A higher coverage speed in z‑axis reduces the acquisition time. Shortening of the scan time improves CT imaging of patients who are unable to hold their breath for a longer time. Furthermore, the shorter acquisition time has the advantages of reduced heart rate variability. Commonly, a long breath-hold is accompanied with tachycardia at the end causing a considerable variability in the length of heart cycles [8]. A shorter breath-hold in turn reduces heart rate variability making the study more robust. In addition, the need for a shorter period of coronary opacification allows a smaller volume of contrast to be used.
Chronology of technical improvements for cardiac CT
The evolution of cardiac CT to its current state is closely correlated with several developments in CT technique in the last decade. Equally, the demand for coronary imaging were the most important pacemakers of CT system improvements.
The precursor of modern CT systems: single‑slice CT
The first step on the way to widespread use of CTCA was the introduction of single‑slice helical CT into clinical practice. By providing a gantry rotation time of 0.8 s and using a halfscan reconstruction algorithm, the temporal resolution was 400 ms. Slice thickness was 3–5 mm. Although better scanning parameters had been achieved earlier with a temporal resolution of 50–100 ms with electron-beam CT in the early 1980s, single‑slice helical CT was the first CT system available for coronary imaging with a wide availability among many institutions worldwide. Although at the level of temporal resolution of the early helical CT systems the coronary arteries were displayed frequently as ‘dancing vessels’ or ‘ghosts’, under optimal conditions with very slow heart rates single‑slice CT could establish the diagnosis of coronary artery stenosis in large proximal vessel segments [9], cardiac thrombus [10] and congenital heart disease [11].
On the way to clinical robustness: multislice CT
The development of multislice CT technology coupled with decreased detector element size, faster gantry rotation speed and increased volume coverage substantially improved coronary imaging capabilities.
Four‑slice CT
Four‑slice CT, which was developed in 1998 and became clinically available in 1999, yielded gantry rotation times of 500–800 ms, resulting in a temporal resolution of as high as 250 ms. The spatial resolution in z‑axis was 1.00–1.25 mm and z‑axis coverage was approximately 2 cm. With these multislice CT systems imaging of the entire heart required approximately 40–50 s, which was longer than most patients could hold their breath. Therefore, preoxygenation was frequently essential to reduce breathing artifacts. Under optimal circumstances, imaging and evaluation of the coronary artery tree, particularly of the proximal coronary artery segments, became technically feasible without artifacts [12–20]. However, small size distal segments and side branches could often not be depicted with adequate image quality, and up to 32% of coronary segments had to been excluded from analysis in four‑slice CT studies [18]. Therefore, the four‑slice CT systems lacked the robustness for implementation of CTCA into clinical practice.
16‑slice CT
The 16‑slice CT systems introduced in 2001 featured gantry rotation times of 380–500 ms, resulting in a temporal resolution of 190–250 ms, a slice thickness of 0.5–0.75 mm and a z‑axis coverage of 24 mm. With these advances, heart imaging within a single breath-hold became feasible, therefore avoiding the need for preoxygenation. Even small coronary segments and side branches could be reliably evaluated with 16‑slice CT [8,21–30], however, up to 21% of coronary segments remained not evaluative in some studies. In a large multicenter trial, 29% of coronary artery segments had nondiagnostic image quality caused by insufficient contrast attenuation (52%), coronary motion artifacts (45%), small vessel caliber (31%), breathing artifacts (19%) and severe calcifications (5%) [31]. These results indicate that the 16‑slice CT technique is still not robust enough for coronary imaging even in patients with low heart rate.
64‑slice CT
The 64‑slice CT systems introduced in 2004 further improved the technical parameters to a gantry rotation time of 330–400 ms (i.e., a temporal resolution of 165–200 ms), a spatial resolution of 0.4–0.625 mm and a detector coverage of 19.2–40 mm. This allowed imaging of the heart in less than 10 s. Improvements in temporal and spatial resolution allowed for detailed evaluation of the coronary arteries and even of small-sized side branches of a diameter of 1 mm and below. Because of the low rate of coronary segments with nondiagnostic image quality and the high diagnostic accuracy, the 64‑slice CT could be considered the first truly feasible CT system capable of coronary artery evaluation in clinical practice [5–7,32–37]. The 64‑slice CT also allowed for more precise characterization of morphology and function of the aortic [38–42] and mitral valve [42,43]. However, the temporal resolution of 64‑slice CT still requires optimal conditions of imaging, in particular a low and stable heart rate [44]. Therefore, premedication with b-blockers prior to CTCA is frequently required when using 64‑slice CT.
Latest improvements in CT technology: more slices, more x‑ray sources
Remaining challenges of temporal resolution and detector coverage have led to the development of the latest CT systems: 256-/320‑slice CT and dual-source CT.
256‑slice/320‑slice CT
To overcome limitations of CTCA in patients with irregular heart beats, large-detector CT systems were developed to allow coverage of the entire heart within a single heart beat. The first CT system capable of single-heart beat CTCA was introduced in 2006 by Toshiba and features a 256‑slice detector array and a spatial resolution of 0.5 mm, resulting in a z‑axis coverage of 128 mm, which permits coverage of the heart in a single gantry rotation. One limitation of this system is the low gantry rotation speed of 500 ms per rotation. However, preliminary results of the ability of 256‑slice CT to assess coronary artery stenosis performed in small patient cohorts are promising [45,46]. Further development has led to the recently introduced 320‑slice CT with a detector coverage of 160 mm and a lower gantry rotation time of 350 ms. First results indicate promising results for imaging the coronary arteries within a single heart beat [47]. Another 256‑slice CT system was introduced by Philips in 2007 that yielded a lower gantry rotation time of 270 ms.
Large volume coverage CT might open the field for new cardiac imaging applications including observation of evolving processes, such as coronary contrast flow and whole heart perfusion.
Dual-source CT
The dual-source CT scanner introduced by Siemens in 2005 is characterized by two x‑ray tubes and two corresponding detectors mounted onto the rotating gantry with an angular offset of 90° [48]. Therefore, a quarter rotation of each tube rather than a half rotation required with single-source CT is sufficient to acquire the required projection data for image reconstruction. The first generation of dual-source CT (Definition) provides two detector arrays each capable of acquiring 64 slices and a gantry rotation time of 330 ms, thus the first-generation dual-source CT system offers a temporal resolution of 83 ms in a mono-segment reconstruction mode that is consistent throughout various heart rates owing to individual adaptation of the table pitch. Consequently, dual-source CT provides a sufficient temporal resolution for coronary imaging even at high heart rates [48–50] and provides a high diagnostic accuracy with a low rate of not-evaluative coronary segments [51–58].
Recently, a second-generation dual-source CT (Definition Flash) has been introduced featuring 2 × 128 slices and a gantry rotation time of 280 ms, providing a temporal resolution of 75 ms. While a low pitch is needed for overlapping data acquisition in 64‑slice CT, the second-generation dual-source CT can achieve gapless z‑sampling even with a pitch of up to 3.2. Therefore, it enables complete coverage of the heart in a single heart beat.
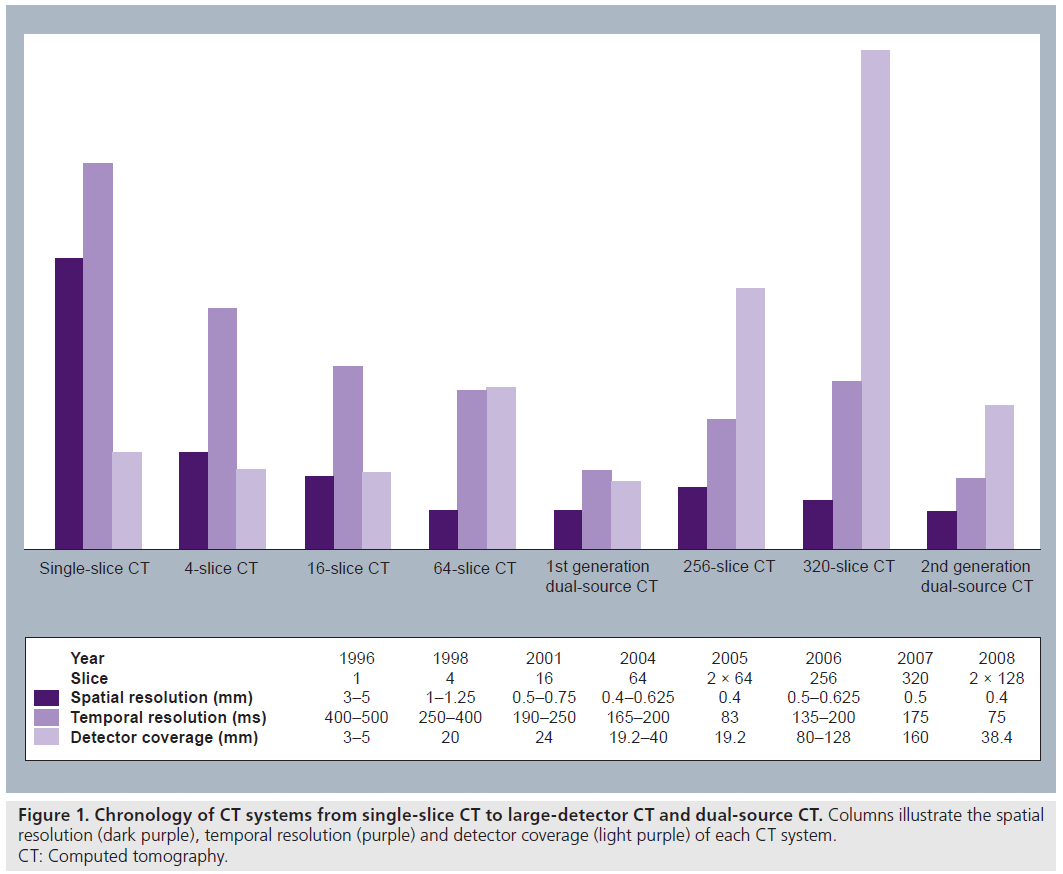
Development of technical parameters
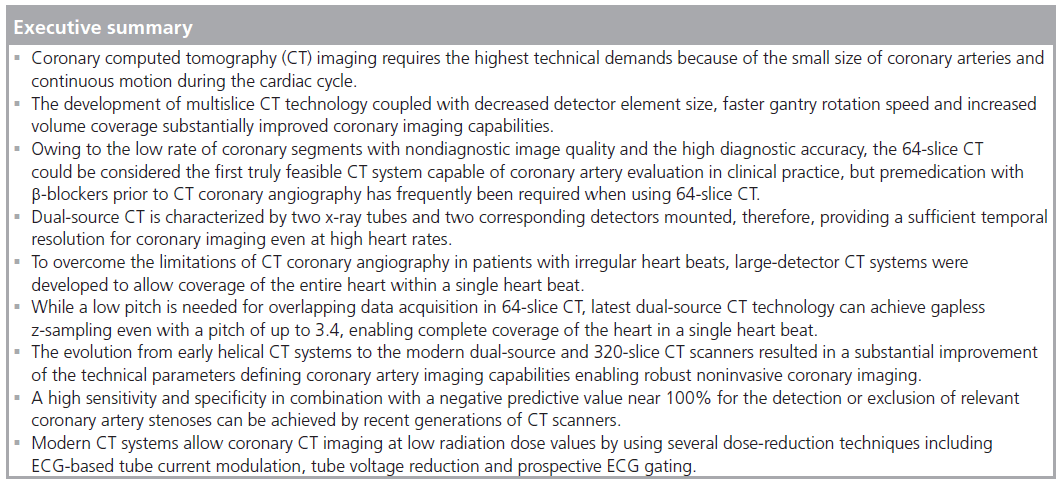
The evolution from early helical CT systems to the modern dual-source and 320‑slice CT scanners resulted in a substantial improvement in the technical parameters defining coronary artery imaging capabilities (Figure 1).
Development of spatial resolution
The spatial resolution has not substantially improved with dual-source CT or 256‑ and 320‑slice CT systems compared with those achieved with 64‑slice CT. However, it has been reported that blooming artifacts of severely calcified deposits are less pronounced in dualsource CTCA than in 64‑slice CTCA [51]. The authors concluded that, considering the fact that the spatial resolution of dual-source CT is the same as that of a single source 64‑slice CT scanner, this apparent difference in calcification dependency could indicate that the blooming artifact of severely calcified vessel walls may be sometimes superimposed by additional motion artifacts [51]. In 2008, one vendor introduced a CT system with gemstone detectors (VCT Discovery 750 HD, General Electric Healthcare), which improved photon detection by shortening the afterglow period and thereby improving spatial resolution. However, it is unclear whether this new detector material will substantially improve spatial resolution and improve assessability of stent patency or coronary artery stenosis caused by severely calcified atherosclerotic plaques.
Development of temporal resolution
In order to achieve a temporal resolution better than the 100 ms at present gantry rotation times, which is considered necessary to overcome the challenge of motion artifacts at higher heart rates, two different concepts have been developed: the multisegment reconstruction algorithm and the dual-source concept.
With the multisegment reconstruction approach, small portions of projection data are selected from two or more heart cycles and all projections are combined to obtain sufficient data for image reconstruction. The maximal achievable temporal resolution could than be the gantry rotation time divided by two (halfscan reconstruction) and divided by the number of heart cycles averaged for image reconstruction. Despite effectively improving the temporal resolution, additional motion artifacts might be introduced in the images by multisegment reconstruction. Even at a steady heart rate, the cardiac position in the thoracic cage is not absolutely fixed and changes depending on the actual ventricular filling and function. Merging of data from two or more consecutive cycles results in image data that do not exactly match together and results in motion artifacts that are more pronounced in patients with variable heart rate [3,4,44]. The disadvantage of multisegment reconstruction algorithms in patients with variable heart rate has even been shown with modern CT systems [59].
The other method introduced for improving temporal resolution is the dual-source CT concept. This approach has shown improved image quality by reducing motion artifacts without administration of b-blockers for heart-rate control [51–53,57].
Development of z‑axis coverage
The z‑axis coverage speed has increased tremendously with recent CT developments. Scan time for covering the entire heart is more than 40 s with four‑slice CT, 16–20 s with 16‑slice CT and less than 10 s with current 64‑slice CT systems. Modern 320‑slice CT and second-generation dual-source CT systems permit imaging of the entire heart in a single heart beat, allowing sub-second cardiac imaging. In addition, the developments in z‑axis coverage resulted in a decrease in the amount of contrast media required for CTCA. While up to 160 ml of contrast media was needed when CTCA was first used [60], this amount has been reduced to 50–80 ml with dualsource and 320‑slice CT [47,50,51,53,57,61].
Diagnostic performance of CTCA
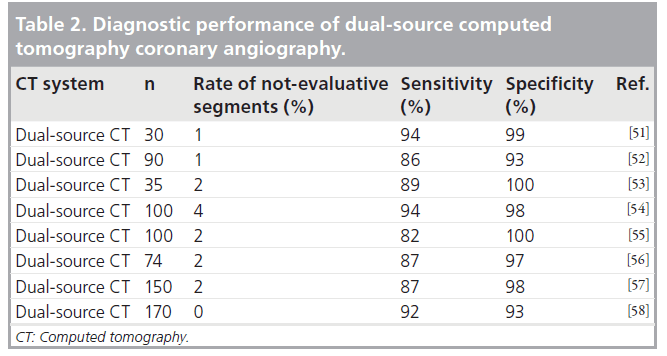
Development of diagnostic performance of CTCA
Numerous studies have evaluated the diagnostic ability of CTCA for the assessment of coronary artery stenosis in correlation with catheter angiography for different generations of CT systems (Tables 1 & 2). The effect of improvement in CT technology on the diagnostic accuracy can be summarized in the following bullet points [62]:
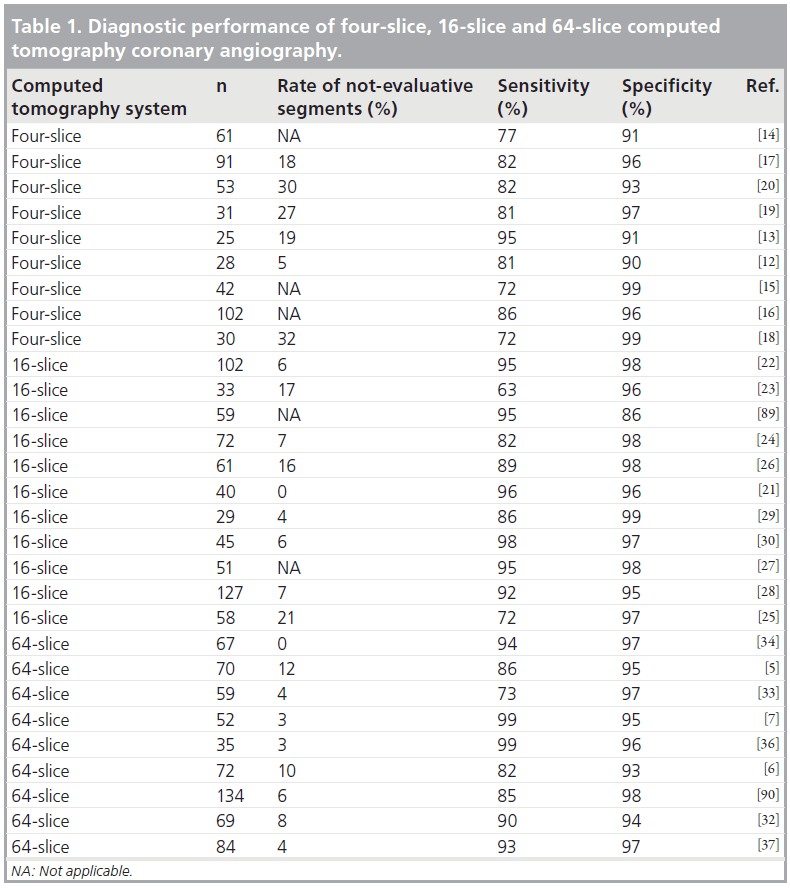
• Patients with significant stenosis (>50% luminal diameter narrowing) were detected with 95% or higher sensitivity with four‑slice, 16‑slice and 64‑slice CT;
• The negative predictive value for CTCA is near 100%;
• Average specificity for patients with significant stenosis has increased with modern CT technology;
• The number of nonevaluable segments decreased significantly with modern CT technology;
• Stenosis in proximal and mid-segments were shown with a higher sensitivity than distal segments.
Several studies have demonstrated that dualsource CT has a high diagnostic accuracy for the assessment of coronary artery stenosis coupled with a low rate of not-evaluative coronary segments [51–58]. A recently published study by Alkadhi and colleagues investigating diagnostic performance of dual-source CTCA in 150 patients reported no significant decrease in diagnostic accuracy in patients with high heart rates or overweight patients [57]. However, severe coronary calcifications increase the rate of falsepositive classifications and therefore decrease the specificity and positive predictive value.
Comparison with alternative noninvasive coronary imaging modalities
In comparison with magnetic resonance coronary angiography (MRCA), CTCA has a superior spatial resolution, image acquisition time and signal-to-noise ratio [63]. Although MRCA has the great advantage that it does not apply either x‑ray radiation or iodinated contrast media, the diagnostic performance and robustness of MRCA is not currently sufficient for use in clinical practice. In a recent meta‑analysis including 39 studies comparing MRCA with catheter coronary angiography (CCA) as the standard of reference, the sensitivity was 73% and the specificity was 86% [64]. Compared with MRCA, CTCA currently has a significantly higher diagnostic accuracy for the assessment of coronary artery disease (CAD) [65].
Noninvasive coronary CT imaging: recent indications
The introduction of 64‑slice CT has allowed the implementation of noninvasive CTCA into daily clinical practice. This was fascilitated by the higher temporal and spatial isotropic resolution. Thereby, 64‑slice CT provides a high diagnostic accuracy for the assessment of the coronaries, and, in particular, its high negative predictive value allows for the exclusion of significant coronary stenoses [5–7,34].
Thus, the Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology has recently recommended in their guidelines the performance of CTCA in patients that have stable angina, a low pretest probability of CAD and a nonconclusive exercise ECG or stress imaging test [66]. Similarly, the American Heart Association states that, particularly if the symptoms, age and gender of a patient suggests a low-to-intermediate pretest probability of hemodynamically relevant stenoses, ruling out these stenoses by CTCA may be clinically useful and may help to avoid invasive catheter angiography [67].
Recently, the use of ECG-gated CTCA in the emergency department has been shown to improve the triage of patients with acute chest pain by decreasing the delay in diagnosis and treatment and, thus, morbidity and mortality [68]. In addition, appropriateness criteria for cardiac CT demonstrate the role of coronary angiography for patients with acute chest pain, but no ECG changes and negative cardiac enzymes [69]. In addition, CTCA is very well established as the imaging modality of choice in patients with suspected coronary anomalies [70].
Regarding patients after bypass graft surgery, CTCA may be useful in selected patients (e.g., failed visualization of a graft in invasive angiography), however, the inability to reliably visualize the native coronary arteries poses severe restrictions to the general use of CTCA in these patients [70].
Limitations of CTCA
Coronary imaging in difficult conditions
Elevated heart rates and irregular heart rates in particular have posed a challenge when using previous CT systems [4,44,71]. Single extrasystoles during CT acquisition do not commonly substantially degrade image quality when ECG editing techniques are used [72]. With the improved temporal resolution of modern CT systems, the application of CTCA has been extended to patients with atrial fibrillation, but at the price of a higher dose [61,73–75]. However, the combination of high and irregular heart rates is associated with a decrease in image quality when using CT [49].
High-density material such as calcified deposits in the arterial wall or coronary stents may cause several image artifacts that may limit accurate assessment of the coronary lumen. In particular, severe coronary calcifications may hinder inspection of the coronary lumen, and may cause overestimation of the severity of the stenosis. However, one has to bear in mind that a high coronary calcium score commonly indicates that a patient has a higher risk of CAD, and, therefore, does not constitute a proper indication for CTCA. Similarly, the evaluation of in-stent restenosis is not a recommended indication for performing CTCA according to current guidelines [66,67,69]. Therefore, both limitations are usually not encountered in clinical practice when adequate indications for performing CTCA are applied.
Another shortcoming of CTCA compared with CCA is its inability to produce timeresolved imaging. The speed and the direction of blood flow in a coronary artery and across a coronary stenosis are not obtainable on CTCA. However, large-detector CT and second-generation dual-source CT capable of cardiac imaging within a single heart beat might allow assessment of flow characteristics by acquisition of data during various heart cycles. Future research using these CT systems needs to reveal whether the clinical benefit of coronary flow assessment will outweigh the risk of the additional radiation exposure.
Radiation dose issues
One of the greatest barriers for CTCA becoming a standard tool in the cardiac imaging armamentarium had been the high radiation exposure of CTCA compared with that of CCA. The radiation dose from 16‑slice CTCA has been estimated at approximately 9 mSv [76]. However, this radiation dose substantially increased in 64‑slice CTCA to approximately 15 mSv for men and 20 mSv for women [36]. These radiation doses are significantly higher compared with that usually applied in CCA where the dose is between 2.1 and 7 mSv [7,77]. The radiation dose estimates of CTCA were achieved when using common retrospective ECG triggering for phase synchronization. Improvements in CT techniques also permit application of potential radiation dose-reduction methods. Current CT systems are capable of modulating the tube current during different phases of the cardiac cycle (ECG-based tube current modulation); the maximal tube output is applied during predefined phases likely used for image reconstruction and tube current output is reduced during the remaining phases of the cardiac cycle [50]. Using this technique, radiation doses of 6.4 mSv for 16‑slice CT [78], 9.4 mSv for 64‑slice CT [78] and 8.8 mSv for dual-source CT [79] have been reported. Another method to reduce the radiation dose is to reduce the tube voltage. Abara et al. used a 80 kVp tube voltage in slim patients with a bodyweight under 60 kg and reported a dosesaving potential of 88% [80]. Tube voltages of 100 kVp have been successfully used for 16‑slice CT [78], 64‑slice CT [78] and dual-source CT [81,82], with a dose-saving potential of up to 40% reported. This benefit is independent and incremental to radiation dose savings by using ECG pulsing.
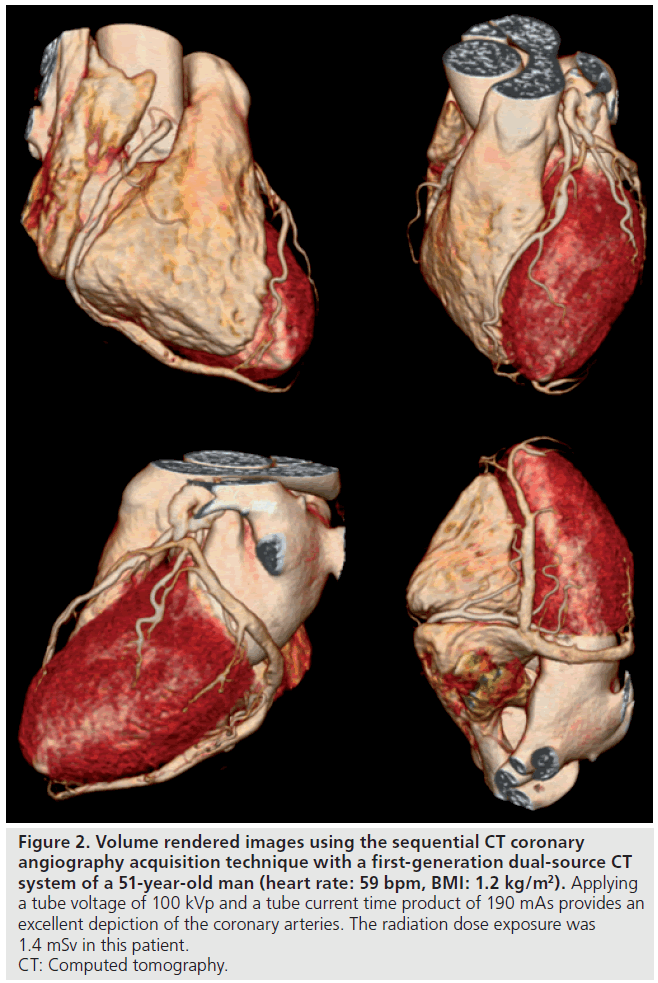
One of the most effective methods for radiation dose reduction in CTCA is the use of prospective ECG gating, also known as sequential cardiac scanning. This technique was first used in electron beam CTCA in 1995 and has been used for calcium scoring by CT since 1998 [83]. Despite irradiating during the entire cardiac cycle, x‑ray is turned on during a short exposure period and turned off during the rest of the cardiac cycle. Sequential cardiac scanning is recommended for patients with heart rates below 70 bpm. Several studies have reported excellent image quality [84–86] and diagnostic accuracy [87,88] of prospectively ECG-gated CTCA at radiation doses of between 1 and 3 mSv (Figure 2) [84–88].
Figure 2. Volume rendered images using the sequential CT coronary angiography acquisition technique with a first-generation dual-source CT system of a 51-year-old man (heart rate: 59 bpm, BMI: 1.2 kg/m2). Applying a tube voltage of 100 kVp and a tube current time product of 190 mAs provides an excellent depiction of the coronary arteries. The radiation dose exposure was 1.4 mSv in this patient. CT: Computed tomography.
Conclusion
Owing to rapid technical developments over the last 10 years, CTCA has progressively advanced from a new imaging modality applied only for research purposes to that of an increasingly used diagnostic tool in clinical practice. Although 64‑slice CT is considered the first truly feasible CT system capable of coronary artery evaluation, even with 64‑slice CT physical limitations still exist in cardiac imaging. Key issues in cardiac CT are spatial and, in particular, include temporal resolution as well as radiation dose and volume coverage. The current state-of-the art CT systems, including dual-source CT and 256-/320‑slice CT, provide solutions for the remaining challenges encountered with previous scanner types at reduced radiation dose levels by improved spatiotemporal resolutions. These CT systems also open the field for potential new cardiac applications, such as assessment of coronary contrast flow, whole heart perfusion and dualenergy cardiac imaging. In the future, it is likely that technical developments will combine the benefits of extended z‑axis coverage with temporal resolution gains of dual-source CT. This future CT system might allow the combination of a perfusion study with precise coronary artery evaluation in a single heart beat that would likely be a valuable mode for the evaluation of CAD by providing both anatomic and physiologic data in one study.
Future perspective
Although cardiac CT has evolved into a robust and accurate tool for diagnosis of CAD in clinical practice, new technologies and applications are likely to be developed that may allow more certain and rapid analysis and further cardiac pathologies to be diagnosed with CT. Advantages of the 320‑slice CT (large-detector coverage) and that of dual-source CT (high temporal resolution, dual-energy information) might be combined in future CT systems. Variations of this design with even more slices and more than two x‑ray tubes might permit imaging of the entire heart within one heart beat irrespective of the heart rate and without any detectable motion artifacts. Further applications to be refined for cardiac CT might include myocardial perfusion kinetics as well as precise analysis of coronary atherosclerotic plaque morphology by the means of dual-energy material decomposition. Future CT systems may combine all currently used modalities in the cardiological armamentarium into one cardiac CT acquisition that provides comprehensive evaluation of the heart and thoracic structures.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Papers of special note have been highlighted as:
* of interest
* of considerable interest.
References
- Lindsten J: Nobel Lectures, Physiology or Medicine 1971–1980. World Scientific Publishing Co., Singapore 568–586 (1992).
- Flohr TG, Schoepf UJ, Ohnesorge BM: Chasing the heart: new developments for cardiac CT. J. Thorac. Imaging 22, 4–16 (2007). & Overview on recent development in cardiac computed tomography (CT).
- Flohr T, Ohnesorge B: Heart rate adaptive optimization of spatial and temporal resolution for electrocardiogram-gated multislice spiral CT of the heart. J. Comput. Assist. Tomogr. 25, 907–923 (2001).
- Wintersperger BJ, Nikolaou K, von Ziegler F et al.: Image quality, motion artifacts, and reconstruction timing of 64-slice coronary computed tomography angiography with 0.33-second rotation speed. Invest. Radiol. 41, 436–442 (2006).
- Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA: Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J. Am. Coll. Cardiol. 46, 552–557 (2005).
- Nikolaou K, Knez A, Rist C et al.: Accuracy of 64-MDCT in the diagnosis of ischemic heart disease. AJR Am. J. Roentgenol. 187, 111–117 (2006).
- Mollet NR, Cademartiri F, van Mieghem CA et al.: High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112, 2318–2323 (2005).
- Nieman K, Rensing BJ, van Geuns RJ et al.: Non-invasive coronary angiography with multislice spiral computed tomography: impact of heart rate. Heart 88, 470–474 (2002).
- Mochizuki T, Murase K, Koyama Y, Higashino H, Ikezoe J: LAD stenosis detected by subsecond spiral CT. Circulation 99, 1523 (1999).
- Mochizuki T, Koyama Y, Tanaka H et al.: Images in cardiovascular medicine. Left ventricular thrombus detected by two- and three-dimensional computed tomographic ventriculography: a new application of helical CT. Circulation 98, 933–934 (1998).
- Mochizuki T, Murase K, Higashino H et al.: Images in cardiovascular medicine. Demonstration of acute myocardial infarction by subsecond spiral computed tomography: early defect and delayed enhancement. Circulation 99, 2058–2059 (1999).
- Becker CR, Knez A, Leber A et al.: Detection of coronary artery stenoses with multislice helical CT angiography. J. Comput. Assist. Tomogr. 26, 750–755 (2002).
- Dirksen MS, Jukema JW, Bax JJ et al.: Cardiac multidetector-row computed tomography in patients with unstable angina. Am. J. Cardiol. 95, 457–461 (2005).
- Gaudio C, Mirabelli F, Alessandra L et al.: Noninvasive assessment of coronary artery stenoses by multidetector-row spiral computed tomography: comparison with conventional angiography. Eur. Rev. Med. Pharmacol. Sci. 9, 13–21 (2005).
- Herzog C, Ay M, Engelmann K et al.: Visualization techniques in multislice CT-coronary angiography of the heart. Correlations of axial, multiplanar, threedimensional and virtual endoscopic imaging with the invasive diagnosis. Rofo 173, 341–349 (2001).
- Kopp AF, Schroeder S, Kuettner A et al.: Non-invasive coronary angiography with high resolution multidetector-row computed tomography. Results in 102 patients. Eur. Heart J. 23, 1714–1725 (2002).
- Leber AW, Knez A, Becker C et al.: Non-invasive intravenous coronary angiography using electron beam tomography and multislice computed tomography. Heart 89, 633–639 (2003).
- Morgan-Hughes GJ, Marshall AJ, Roobottom CA: Multislice computed tomographic coronary angiography: experience in a UK centre. Clin. Radiol. 58, 378–383 (2003).
- Nieman K, Oudkerk M, Rensing BJ et al.: Coronary angiography with multi-slice computed tomography. Lancet 357, 599–603 (2001).
- Nieman K, Rensing BJ, van Geuns RJ et al.: Usefulness of multislice computed tomography for detecting obstructive coronary artery disease. Am. J. Cardiol. 89, 913–918 (2002).
- Cademartiri F, Runza G, Marano R et al.: Diagnostic accuracy of 16-row multislice CT angiography in the evaluation of coronary segments. Radiol. Med. 109, 91–97 (2005).
- Hoffmann MH, Shi H, Schmitz BL et al.: Noninvasive coronary angiography with multislice computed tomography. JAMA 293, 2471–2478 (2005).
- Hoffmann U, Moselewski F, Cury RC et al.: Predictive value of 16-slice multidetector spiral computed tomography to detect significant obstructive coronary artery disease in patients at high risk for coronary artery disease: patient-versus segment-based analysis. Circulation 110, 2638–2643 (2004).
- Kuettner A, Beck T, Drosch T et al.: Diagnostic accuracy of noninvasive coronary imaging using 16-detector slice spiral computed tomography with 188 ms temporal resolution. J. Am. Coll. Cardiol. 45, 123–127 (2005).
- Kuettner A, Trabold T, Schroeder S et al.: Noninvasive detection of coronary lesions using 16-detector multislice spiral computed tomography technology: initial clinical results. J. Am. Coll. Cardiol. 44, 1230–1237 (2004).
- Martuscelli E, Romagnoli A, D’Eliseo A et al.: Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur. Heart J. 25, 1043–1048 (2004).
- Mollet NR, Cademartiri F, Krestin GP et al.: Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J. Am. Coll. Cardiol. 45, 128–132 (2005).
- Mollet NR, Cademartiri F, Nieman K et al.: Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J. Am. Coll. Cardiol. 43, 2265–2270 (2004).
- Paul JF, Ohanessian A, Caussin C et al.: Visualization of coronary tree and detection of coronary artery stenosis using 16-slice, sub-millimeter computed tomography: preliminary experience. Arch. Mal. Coeur Vaiss. 97, 31–36 (2004).
- Schuijf JD, Bax JJ, Salm LP et al.: Noninvasive coronary imaging and assessment of left ventricular function using 16-slice computed tomography. Am. J. Cardiol. 95, 571–574 (2005).
- Garcia MJ, Lessick J, Hoffmann MH: Accuracy of 16-row multidetector computed tomography for the assessment of coronary artery stenosis. JAMA 296, 403–411 (2006).
- Ehara M, Surmely JF, Kawai M et al.: Diagnostic accuracy of 64-slice computed tomography for detecting angiographically significant coronary artery stenosis in an unselected consecutive patient population: comparison with conventional invasive angiography. Circ. J. 70, 564–571 (2006).
- Leber AW, Knez A, von Ziegler F et al.: Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J. Am. Coll. Cardiol. 46, 147–154 (2005).
- Leschka S, Alkadhi H, Plass A et al.: Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur. Heart J. 26, 1482–1487 (2005).
- Ong AT, Serruys PW, Mohr FW et al.: The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am. Heart J. 151, 1194–1204 (2006).
- Pugliese F, Mollet NR, Runza G et al.: Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur. Radiol. 16, 575–582 (2006).
- Ropers D, Rixe J, Anders K et al.: Usefulness of multidetector row spiral computed tomography with 64- × 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenoses. Am. J. Cardiol. 97, 343–348 (2006).
- Stolzmann P, Knight J, Desbiolles L et al.: Remodelling of the aortic root in severe tricuspid aortic stenosis: implications for transcatheter aortic valve implantation. Eur. Radiol. 19, 1316–1323 (2009).
- Halpern EJ, Mallya R, Sewell M, Shulman M, Zwas DR: Differences in aortic valve area measured with CT planimetry and echocardiography (continuity equation) are related to divergent estimates of left ventricular outflow tract area. AJR Am. J. Roentgenol. 192, 1668–1673 (2009).
- Shah RG, Novaro GM, Blandon RJ et al.: Aortic valve area: meta-analysis of diagnostic performance of multi-detector computed tomography for aortic valve area measurements as compared with transthoracic echocardiography. Int. J. Cardiovasc. Imaging 25(6), 601–609 (2009).
- Alkadhi H, Desbiolles L, Husmann L et al.: Aortic regurgitation: assessment with 64-section CT. Radiology 245, 111–121 (2007).
- Boehm T, Husmann L, Leschka S et al.: Image quality of the aortic and mitral valve with CT: relative versus absolute delay reconstruction. Acad. Radiol. 14, 613–624 (2007).
- Alkadhi H, Desbiolles L, Stolzmann P et al.: Mitral annular shape, size, and motion in normals and in patients with cardiomyopathy: evaluation with computed tomography. Invest. Radiol. 44, 218–225 (2009).
- Leschka S, Wildermuth S, Boehm T et al.: Noninvasive coronary angiography with 64-section CT: effect of average heart rate and heart rate variability on image quality. Radiology 241, 378–385 (2006).
- Kido T, Kurata A, Higashino H et al.: Cardiac imaging using 256-detector row four-dimensional CT: preliminary clinical report. Radiat. Med. 25, 38–44 (2007).
- Motoyama S, Anno H, Sarai M et al.: Noninvasive coronary angiography with a prototype 256-row area detector computed tomography system: comparison with conventional invasive coronary angiography. J. Am. Coll. Cardiol. 51, 773–775 (2008).
- Rybicki FJ, Otero HJ, Steigner ML et al.: Initial evaluation of coronary images from 320-detector row computed tomography. Int. J. Cardiovasc. Imaging 24, 535–546 (2008).
- Flohr TG, McCollough CH, Bruder H et al.: First performance evaluation of a dual-source CT (DSCT) system. Eur. Radiol. 16, 256–268 (2006). & Technical concepts of dual-source CT.
- Matt D, Scheffel H, Leschka S et al.: Dual-source CT coronary angiography: image quality, mean heart rate, and heart rate variability. AJR Am. J. Roentgenol. 189, 567–573 (2007).
- Leschka S, Scheffel H, Desbiolles L et al.: Image quality and reconstruction intervals of dual-source CT coronary angiography: recommendations for ECG-pulsing windowing. Invest. Radiol. 42, 543–549 (2007).
- Scheffel H, Alkadhi H, Plass A et al.: Accuracy of dual-source CT coronary angiography: first experience in a high pre-test probability population without heart rate control. Eur. Radiol. 16, 2739–2747 (2006).
- Leber AW, Johnson T, Becker A et al.: Diagnostic accuracy of dual-source multi-slice CT-coronary angiography in patients with an intermediate pretest likelihood for coronary artery disease. Eur. Heart J. 28, 2354–2360 (2007).
- Johnson TR, Nikolaou K, Busch S et al.: Diagnostic accuracy of dual-source computed tomography in the diagnosis of coronary artery disease. Invest. Radiol. 42, 684–691 (2007).
- Ropers U, Ropers D, Pflederer T et al.: Influence of heart rate on the diagnostic accuracy of dual-source computed tomography coronary angiography. J. Am. Coll. Cardiol. 50, 2393–2398 (2007).
- Brodoefel H, Burgstahler C, Tsiflikas I et al.: Dual-source CT: effect of heart rate, heart rate variability, and calcification on image quality and diagnostic accuracy. Radiology 247, 346–355 (2008).
- Leschka S, Scheffel H, Desbiolles L et al.: Combining dual-source computed tomography coronary angiography and calcium scoring: added value for the assessment of coronary artery disease. Heart 94, 1154–1161 (2008).
- Alkadhi H, Scheffel H, Desbiolles L et al.: Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur. Heart J. 29, 766–776 (2008).
- Tsiflikas I, Brodoefel H, Reimann AJ et al.: Coronary CT angiography with dual source computed tomography in 170 patients. Eur. J. Radiol. (2009) (Epub ahead of print).
- Leschka S, Alkadhi H, Stolzmann P et al.: Mono- versus bisegment reconstruction algorithms for dual-source computed tomography coronary angiography. Invest. Radiol. 43, 703–711 (2008).
- Achenbach S, Ulzheimer S, Baum U et al.: Noninvasive coronary angiography by retrospectively ECG-gated multislice spiral CT. Circulation 102, 2823–2828 (2000).
- Rist C, Johnson TR, Muller-Starck J et al.: Noninvasive coronary angiography using dual-source computed tomography in patients with atrial fibrillation. Invest. Radiol. (2009) (Epub ahead of print).
- Stein PD, Beemath A, Kayali F et al.: Multidetector computed tomography for the diagnosis of coronary artery disease: a systematic review. Am. J. Med. 119, 203–216 (2006). & Meta-analysis of diagnostic accuracy progress from four-slice to 64-slice coronary CT angiography.
- Peebles CR: Non-invasive coronary imaging: computed tomography or magnetic resonance imaging? Heart 89, 591–594 (2003).
- Danias PG, Roussakis A, Ioannidis JP: Diagnostic performance of coronary magnetic resonance angiography as compared against conventional x-ray angiography: a metaanalysis. J. Am. Coll. Cardiol. 44, 1867–1876 (2004).
- Schuijf JD, Bax JJ, Shaw LJ et al.: Meta-analysis of comparative diagnostic performance of magnetic resonance imaging and multislice computed tomography for noninvasive coronary angiography. Am. Heart J. 151, 404–411 (2006).
- Fox K, Garcia MA, Ardissino D et al.: Guidelines on the management of stable angina pectoris: executive summary: the Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur. Heart J. 27, 1341–1381 (2006).
- Budoff MJ, Achenbach S, Blumenthal RS et al.: Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 114, 1761–1791 (2006).
- Hoffmann U, Nagurney JT, Moselewski F et al.: Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation 114, 2251–2260 (2006).
- Hendel RC, Patel MR, Kramer CM et al.: ACCF/ACR/SCCT/SCMR/ASNC/NASCI/ SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J. Am. Coll. Cardiol. 48, 1475–1497 (2006). & Appropriateness criteria for the use of cardiac CT.
- Schroeder S, Achenbach S, Bengel F et al.: Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur. Heart J. 29, 531–556 (2008).
- Herzog C, Arning-Erb M, Zangos S et al.: Multi-detector row CT coronary angiography: influence of reconstruction technique and heart rate on image quality. Radiology 238, 75–86 (2006).
- Cademartiri F, Mollet NR, Runza G et al.: Improving diagnostic accuracy of MDCT coronary angiography in patients with mild heart rhythm irregularities using ECG editing. AJR Am. J. Roentgenol. 186, 634–638 (2006).
- Tsiflikas I, Drosch T, Brodoefel H et al.: Diagnostic accuracy and image quality of cardiac dual-source computed tomography in patients with arrhythmia. Int. J. Cardiol. (2009) (Epub ahead of print).
- Wolak A, Gutstein A, Cheng VY et al.: Dual-source coronary computed tomography angiography in patients with atrial fibrillation: initial experience. J. Cardiovasc. Comput. Tomogr. 2, 172–180 (2008).
- Oncel D, Oncel G, Tastan A: Effectiveness of dual-source CT coronary angiography for the evaluation of coronary artery disease in patients with atrial fibrillation: initial experience. Radiology 245, 703–711 (2007).
- Bae KT, Hong C, Whiting BR: Radiation dose in multidetector row computed tomography cardiac imaging. J. Magn. Reson. Imaging 19, 859–863 (2004).
- Kocinaj D, Cioppa A, Ambrosini G et al.: Radiation dose exposure during cardiac and peripheral arteries catheterisation. Int. J. Cardiol. 113, 283–284 (2006).
- Hausleiter J, Meyer T, Hadamitzky M et al.: Radiation dose estimates from cardiac multislice computed tomography in daily practice: impact of different scanning protocols on effective dose estimates. Circulation 113, 1305–1310 (2006).
- Stolzmann P, Scheffel H, Schertler T et al.: Radiation dose estimates in dual-source computed tomography coronary angiography. Eur. Radiol. 18, 592–599 (2008).
- Abada HT, Larchez C, Daoud B, Sigal-Cinqualbre A, Paul JF: MDCT of the coronary arteries: feasibility of low-dose CT with ECG-pulsed tube current modulation to reduce radiation dose. AJR Am. J. Roentgenol. 186, S387–S390 (2006).
- Leschka S, Stolzmann P, Schmid FT et al.: Low kilovoltage cardiac dual-source CT: attenuation, noise, and radiation dose. Eur. Radiol. 18, 1809–1817 (2008).
- Alkadhi H, Stolzmann P, Scheffel H et al.: Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur. J. Radiol. 68, 385–391 (2008). & Practical approach for using radiation dose-reduction strategies in daily clinical practice.
- Budoff MJ: Maximizing dose reductions with cardiac CT. Int. J. Cardiovasc. Imaging 25(Suppl. 2), 279–287 (2009). nn Comprehensive review on radiation dose-reduction strategies.
- Gopal A, Mao SS, Karlsberg D et al.: Radiation reduction with prospective ECG-triggering acquisition using 64-multidetector computed tomographic angiography. Int. J. Cardiovasc. Imaging 25, 405–416 (2009).
- Stolzmann P, Leschka S, Scheffel H et al.: Dual-source CT in step-and-shoot mode: noninvasive coronary angiography with low radiation dose. Radiology 249, 71–80 (2008).
- Earls JP, Schrack EC: Prospectively gated low-dose CCTA: 24 months experience in more than 2,000 clinical cases. Int. J. Cardiovasc. Imaging 25(Suppl. 2), 177–187 (2009).
- Stolzmann P, Scheffel H, Leschka S et al.: Influence of calcifications on diagnostic accuracy of coronary CT angiography using prospective ECG triggering. AJR Am. J. Roentgenol. 191, 1684–1689 (2008).
- Scheffel H, Alkadhi H, Leschka S et al.: Low-dose CT coronary angiography in the step-and-shoot mode: diagnostic performance. Heart 94, 1132–1137 (2008).
- Nieman K, Cademartiri F, Lemos PA et al.: Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106, 2051–2054 (2002).
- Ong TK, Chin SP, Liew CK et al.: Accuracy of 64-row multidetector computed tomography in detecting coronary artery disease in 134 symptomatic patients: influence of calcification. Am. Heart J. 151, e1321-e1326 (2006).