Case Report - Clinical Practice (2022) Volume 19, Issue 4
Recurrent Cerebral Venous Sinus Thromboses (CVSTââ?‰?¢s) and Livedo Reticularis Rash ââ?‰?? A Case of Sneddon Syndrome
- Corresponding Author:
- V Shukla
Paediatric Department, Eric Williams Medical Sciences Complex, Trinidad & Tobago
E-mail:Paediatric Department, Eric Williams Medical Sciences Complex, Trinidad & Tobago
Abstract
Sneddon Syndrome (SS) is a rare, progressive small and medium-vessel vasculopathy characterized by livedo racemosa and ischaemic cerebrovascular events. An 18-year-old female of East Indian descent presented with recurrent Cerebral Venous Sinus Thromboses and a livedo reticularis rash. She was treated for a CNS vasculitis/Catastrophic Antiphospholipid Syndrome when she presented with refractory status epilepticus and raised intracranial pressure. Her neurological state gradually improved (coma ->vegetative state ->minimally conscious ->conscious). Skin biopsy was suggestive of an obstructive vasculopathy. There are few case reports describing SS. We aim to highlight the clinical course and treatment of this rare diagnostic entity.
Keywords
case report, sneddon syndrome, cerebral venous sinus thrombosis, livedo reticularis rash.
Introduction and case description
Our patient first presented at 8 years old with a new-onset squint, ataxia, and fever and was treated as culture-negative meningitis (CSF white cells 1238 neutrophils, CSF protein 110 mg/dL). She eventually recovered back to baseline within 6 months. At 15 years old, she presented with expressive aphasia, headache, fever, and left earache, and was treated as acute mastoiditis. However, two years later, on review of the CT head done during this admission, left transverse sinus thrombosis was noted.
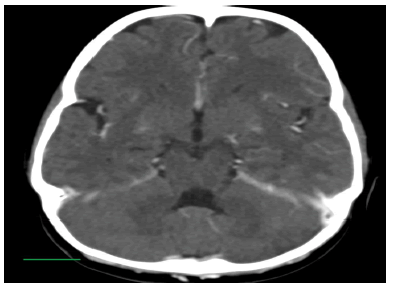
At the age 17-years-old, she presented with headache and vomiting, and a CT head revealed right transverse sinus thrombosis. Extension into the sigmoid sinus and straight and posterior superior sagittal sinus occurred despite anticoagulation with oral warfarin. A distinctive rash was noted over her trunk and limbs during these admissions, with a brownishpurple reticulated pattern of irregular broken circles that worsened when she was unwell. She was also assessed as being cognitively delayed.
Due to her clinical presentation (recurrent CVSTs and livedo reticularis rash), CVST’s refractory to anticoagulation treatment, and evidence of systemic inflammation (elevated ESR 72-80, C3 168, C4 46), an autoimmune workup was done (including pANCA studies) and she was started on oral steroids. Her clinical status and inflammatory markers improved (ESR 33, C3 143, C4 36) and she was subsequently discharged on high-dose oral prednisolone and Low-Molecular-Weight Heparin (LMWH).
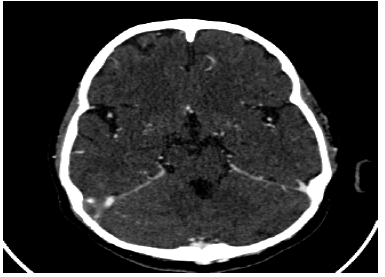
However, after being non-compliant with LMWH and steroids for 1 week, she presented with progressive focal right-sided weakness, expressive aphasia, and within 24 hours, encephalopathic with decerebrate posturing in subclinical status epilepticus. Neuroimaging revealed a venous infarct with surrounding edema. She was managed in PICU for refractory status epilepticus and raised intracranial pressure.
Her inflammatory markers continued to increase despite antibiotic coverage at meningitic doses and she was treated for a CNS vasculitis/Catastrophic Antiphospholipid syndrome with IV anticoagulation (UFH), and high-dose steroids and IVIG. Her neurological state gradually improved (coma ->vegetative state ->minimally conscious ->conscious). This was supported electro clinically (Comparative EEGs showed improvement in background slowing (from 2 Hz-3 Hz to 4 Hz-5 Hz) post methylprednisolone and IVIG). This was followed by Rituximab therapy 375 mg/m2 weekly X4. Her neurological function recovered as she was able to verbally communicate and developed anti-gravity movement on the right side, 2-months post-presentation (Modified Rankin Scale (MRS) Score 5 to 3; Rehabilitation Complexity Scale 15/15 {C3 N3 TD3 TI3 M3} to 6/15 {C1 N1 TD2 TI1 M1}). Hypertension and fever also settled, and inflammatory markers steadily decreased post-treatment. Oral prednisolone was gradually weaned, and she continued anticoagulation (LMWH), antiplatelet therapy (low-dose Aspirin), an antiseizure treatment with phenytoin maintenance.
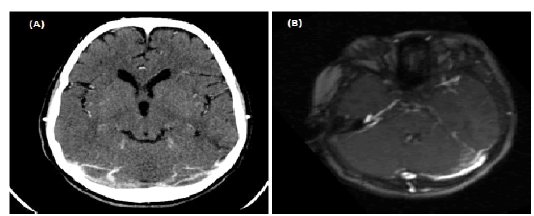
There is a family history of early stroke (maternal cousin with CVST at 8 yo on longterm anticoagulation). Skin biopsy report revealed neutrophils, and lymphocytes of leukocytoclastic seen in the vessels of the dermis. Thrombosis, fibrinoid necrosis of vessel walls, and extravasated red blood cells are also seen Obstructive vasculopathy for clinical correlation; Possible Sneddon syndrome/Antiphospholipid Syndrome (FIGURES 1-4).
Figure 3: Left transverse sinus thrombosis-noted on reviewing scan in late October 2020 (treated as left mastoiditis). CT brain C+ 29/05/2018-filling defect distal left transverse sinus.
■ Other investigations
1. ANA, dsDNA, ENA negative.
2. pANCA borderline positive but MPO,PR3 Antibodies negative.
3. Anticardiolipin antibodies negative (on warfarin).
4. Infectious screen (HIV, Hepatitis, COVID-19 serology, Mantoux test, CSF Acid-fast bacilli)-negative.
5. Repeat CSF cell count -33 white cells (neutrophils); CSF protein 183 mg/dL; CSF M/C/S negative.
6. Blood film-microcytic, hypochromic RBC (Hb~7), Normal WBC, platelet morphology; DCT-Negative.
7. TFT-TSH 1.22, T4 22.4 (Normal).
8. HbA1c-5.2%.
9. Urine spot protein/creatinine ratio-normal; Urine microscopy-normal (no significant red cell casts).
■ Multisystem involvement
1. Eyes: Bilateral optic nerves atrophy.
2. CVS: mild to moderate LAD dilation.(during the most severe presentation), previously normal one-month prior.
3. MS: Right knee joint synovitis; polyarticular arthritis.
Discussion
Sneddon Syndrome (SS) is a rare clinical entity that preferentially involves the cerebral and cutaneous vascular beds. The histological proof of occlusion of arterioles by intimal proliferation cinches the diagnosis.
Three forms of the syndrome were described by Schellong et al [1].
1. Primary, where no causative factor could be identified.
2. Autoimmune with Antiphospholipid antibodies (aPL) or coexisting Systemic Lupus Erythematosus (SLE) or lupus-like disease.
3. Thrombophilic.
It has been estimated that the incidence of SS is 4 per 1 million per annum in the general population and generally occurs in women between the ages of 20 and 42 years [2]. Although the disorder mainly occurs sporadically, a few familial cases have been reported [3]. A genetic autoinflammatory condition was also considered in this case due to her age of first presentation, family history of early stroke, and multi-system involvement. Studies have identified novel mutations in CECR1 (cat eye syndrome chromosome region, candidate 1), encoding Adenosine Deaminase Type 2 (ADA2), as the cause of a syndrome including systemic vasculopathy and inflammation [4]. Bras et al extend the phenotypic spectrum of ADA2 deficiency to include a familial form of SS [5,6].
Deficiency of ADA2 (DADA2) was initially recognized in 2014 as a syndrome that manifests with fevers, polyarteritis nodosa, livedo racemosa, early-onset stroke, and mild immunodeficiency [4,6]. The onset of the disease is usually in childhood with 77% presenting before the age of 10 years.
Treatment of SS is not well documented. Before the histopathological diagnosis, we aggressively managed our patient as a probable Secondary CNS vasculitis/Catastrophic Antiphospholipid Syndrome with high-dose steroids, IV immunoglobulin, and Rituximab. These treatments subsequently improved her neurological outcome.
Based on the presumed pathogenesis of SS, some researchers have recommended long-term anticoagulation for cerebral ischemic events [7,8]. The importance of compliance with anticoagulation and antiplatelet therapy was stressed with the patient and her family.
Conclusion
This is the first documented case of Sneddon Syndrome described in Trinidad and Tobago. The lack of case descriptions alludes to the possibility of unfamiliarity with this rare condition. In the era of more affordable targeted genetic panels and the recent subspecialty service provisions, especially in our pediatric population, we anticipate a greater understanding of the recognition and management of these rare clinical entities.
Acknowledgment
Professor A V C Rao, Department of Pathology, EWMSC, NCRHA.
References
- Schellong SM, Weissenborn K, Niedermeyer J, et al. Classification of Sneddon's syndrome. Vasa. 3, 215-221 (1997).
- Zelger B, Sepp N, Stockhammer G, et al. Review Sneddon's syndrome: A long-term follow-up of 21 patients. Arch Dermatol .4 ,437-447 (1993).
- Szmyrka-Kaczmarek M, Daikeler T, Benz D, et al. Familial inflammatory Sneddon’s syndrome-case report and review of the literature. Clin Rheumatol. 24, 79-82 (2005).
[Google Scholar] [Crossref].
- Zhou Q, Yang D, Ombrello AK, et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med. 10, 911-920 (2014).
- Bras J, Guerreiro R, Santo GC. Mutant ADA2 in vasculopathies. N Engl J Med. 371, 478-480 (2014).
- Navon EP, Pierce SB, Segel R, et al. Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N Engl J Med. 10, 921-931 (2014).
- Khamashta MA, Cuadrado MJ, Mujic F, et al. The management of thrombosis in the antiphospholipid-antibody syndrome. N Engl J Med. 332, 993-997 (1995).
- Rosove MH, Brewer PM. Antiphospholipid thrombosis: clinical course after the first thrombotic event in 70 patients. Ann Intern Med. 117, 303-308 (1992).