Case Report - Interventional Cardiology (2012) Volume 4, Issue 1
Retention and fracture of a hydrophilic radial artery sheath due to severe spasm
- Corresponding Author:
- Pandula Athauda-Arachchi
Regional Cardiothoracic Centre
University Hospital of Morriston
Swansea, SA6 6LN, UK
Tel: +44 1792 702222
Fax: +44 1792 618889
E-mail: pma29@cantab.net
Abstract
Keywords
percutaneous coronary intervention, radial artery spasm, radial sheath complications, transradial coronary angiography
Case history
A 78 year old female patient, who had 2 years previously undergone left anterior descending artery intervention via the right radial artery, presented with anterior non-ST-elevation myocardial infarction. Following initial medical management and ischemic risk stratification, she was transferred to the catheter laboratory for invasive coronary assessment.
Radial access is the default access within our institution. Following adequate local infiltration with 1% lignocaine, the operator easily gained access to the right radial artery using a hydrophilic Cook Flexor® Check-Flo® introducer set (Cook Medical Inc., IN, USA). Access was obtained with the first puncture, with the 21 G micropuncture access needle (provided in this kit) in a noncomplicated manner. The 0.018” nitinol wire (provided in this kit) was advanced through the micropuncture needle in a noncomplicated manner. After ensuring skin incision was satisfactory, the operators attempted to pass a 13 cm long 6 Fr AQ® hydrophilic coated Cook Flexor Check-Flo sheath over the wire, which proved to be difficult (likely due to the small size of the artery, with possibly early spasm) but a 13 cm long 5 Fr AQ hydrophilic coated Cook Flexor Check-Flo radial artery sheath was inserted in an uncomplicated manner. A radial arterial cocktail of 5000 units of heparin and glyceryl trinitrate (GTN) 200 μg and verapamil 2.5 mg was then administered via the sheath.
Diagnostic coronary angiography was then performed using Cordis (Cordis Corp., FL, USA) 5 Fr Judkins catheters in an uncomplicated fashion and this demonstrated an occluded left anterior descending artery due to stent thrombosis. Due to the late presentation, intervention was deferred, pending assessment of myocardial viability.
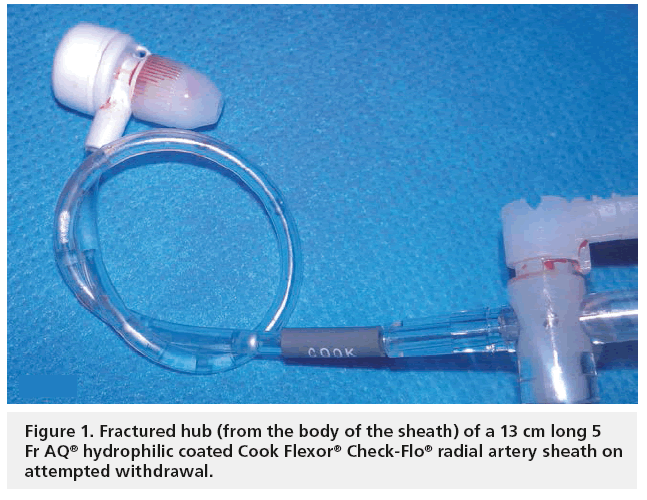
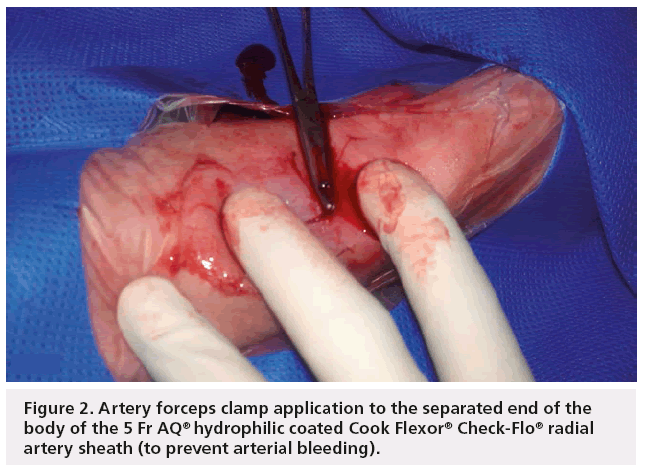
During withdrawal of the final diagnostic catheter over the J tipped 0.035” wire, some resistance was noted, most likely due to radial artery spasm. On attempting to remove the radial sheath, there was marked resistance, leading to administration of a further intra-arterial GTN 200 μg, intraarterial verapamil 2.5 mg and intravenous (iv.) midazolam 2 mg. We also performed fluoroscopy with a small volume of contrast through the side port of the sheath, which did not demonstrate any features suggestive of radial artery dissection or perforation, but demonstrated features consistent with diffuse spasm near to the sheath and away from it (fluoroscopy image acquired but unfortunately not archived – we acknowledge the importance of a cine acquisition and storage). After waiting 10 min for the radial artery spasm to settle, a further attempt at sheath removal was made but the sheath would only withdraw back 1 cm further and at this point, the traction on the sheath against intense spasm resulted in fracture of the hub from the main sheath (Figure 1). The end of the sheath was then clamped with artery forceps (Figure 2) and iv. morphine 15 mg given in three aliquots and further sedation with iv. midazolam 2 mg given to the limit of conscious sedation (with anesthetic support). Two aliquots of papaverine 30 mg were also administered via the radial sheath using a fine needle, as this has previously been reported to help in cases of severe vasospasm. After 15 min, a further attempt at sheath removal was undertaken. Although the spasm was reduced to a degree, the sheath could still only be withdrawn by 1 cm and the recurrence of spasm against the traction resulted in a further fracture of the 1 cm of the sheath, visibly weakened by the whole process.
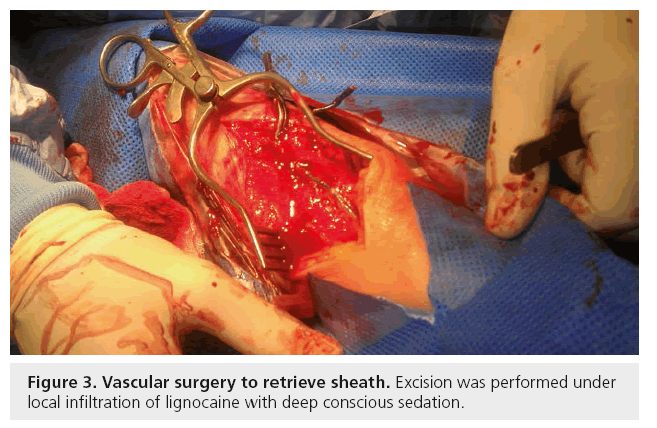
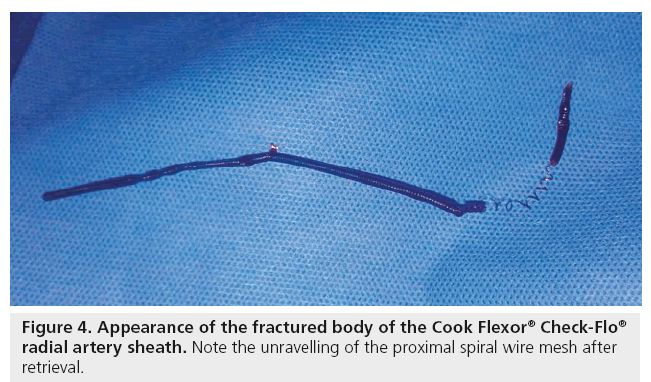
Vascular surgical consultation was then requested. Sheath excision was performed under local infiltration of lignocaine, with deep conscious sedation (Figure 3) under the cover of peri-operative antibiotics. Intraoperatively, manual unraveling of the proximal spiral wire mesh of the radial sheath and complete excision of the radial sheath with ligation proximally and distally of the radial artery, was needed (Figure 4). No clinical vascular compromise of the right hand perfusion resulted from this, due to the presence of a good ulnar arterial supply. The patient made a full recovery after the procedure, with no evidence of hand ischemia and was discharged home two days later with a plan for outpatient viability assessment.
Figure 3: Vascular surgery to retrieve sheath. Excision was performed under local infiltration of lignocaine with deep conscious sedation.
Conclusion
Clinically significant radial access-site complications are extremely uncommon compared with femoral access [1]. This is due to the favorable anatomical relations of the radial artery with its superficial course, allowing easy compression and hemostasis. The collateral ulnar blood supply protects the hand in the event of traumatic or thrombotic radial artery occlusion and the absence of major veins or nerves minimizes the risk of neurovascular injury. Nevertheless, radial artery access-site complications do occur. Radial spasm is a troublesome but consistent feature of transradial (TR) practice and studies show it occurs in approximately 20% of cases if a radial cocktail is not used. The rate of spasm has been shown to be significantly reduced with the use of an intra-arterial vasodilating cocktail [2]. The exact components of the cocktail are debated, but typically 2.5–5 mg verapamil, with or without GTN is injected directly into the radial artery. Some studies have suggested that short radial sheaths may in fact reduce spasm more than long sheaths but others have refuted this fact [3]. Refractory spasm is very rare, but papaverine [4] as well as general anesthesia [5] and occasionally warm compresses [6] have all been reported to help. In our case, standard arterial vasodilator therapy combined with conscious sedation and administration of intra-arterial papaverine, was unsuccessful in relieving refractory spasm. The requirement for open surgical sheath removal could have been particularly problematic had it been in the setting of ST-elevation myocardial infarction or a complicated coronary intervention, where iv. heparin and glycoprotein IIb/IIIa inhibitors had both been used.
We have noted that several cases of malfunction of Cook Flexor Check-Flo sheaths had been previously reported to the US FDA and corrective action by the manufacturer to increase tensile strength had been implemented from 27 June 2008. Therefore, we searched the FDA database [101] from this date onwards using search terms ‘Flexor Check,’ ‘Cook’ and ‘malfunction.’ This revealed 11 cases of malfunction (some of which were not used in radial applications, some caused by malfunction due to fracture of parts other than the hub–sheath junction, e.g., the hydrophilic coating) but, to our knowledge, the retention/fracture at hub–body junction of this short (13 cm) hydrophilic radial artery sheath, in a radial artery, mechanistically due to refractory spasm, has not been reported after the said date, apart from our case report.
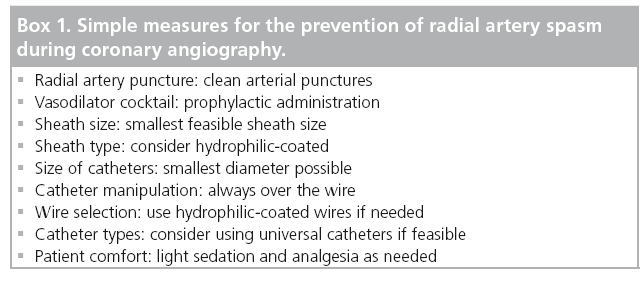
It is, therefore, a salient reminder, even for experienced radial operators, of the importance of following best practice in order to minimize the risks of radial artery spasm (Box 1), the importance of avoiding excessive traction force in cases of refractory spasm and to be aware of reviewing and reporting rare adverse events as described.
Future perspective
The focus and achievements in TR coronary angiography have drastically changed over the last 20 years as a consequence of improvement of technological and procedural skill levels. Most diagnostic and coronary interventions can safely and efficiently be performed without requiring access to the femoral artery. The availability of TR-designated devices, including hydrophilic sheaths, universal catheters and nonocclusive hemostatic devices, along with an understanding of the need for heparin and a spasmolytic cocktail, have drastically improved safety since the early 1990s. The focus at present is not only in achieving procedural success but also avoiding bleeding/vascular access complications, which can largely determine the patient comfort and length of hospital stay, an important consideration in the health economics surrounding coronary intervention. By reducing the time and effort required for sheath removal and vascular compression in the catheterization laboratory and in the wards, TR approach helps to reduce nurse workload in coronary interventions [7]. There is also evidence to suggest that accesssite bleeding and complications are associated with mortality [1,8,9]. Therefore, given the low rates of complications observed in a TR access [1,10], an increasing uptake of the TR approach for coronary angiography is likely to be observed throughout the world.
In this context, it should be remembered that the TR approach is not without rare complications, such as that described in the case report we have presented, even in the hands of skilled operators. To our knowledge, we could not find any published reports of fracture of a hydrophilic radial artery sheaths in contemporary literature. The demonstration that this can occur, raises issues related to improving patient safety. We suggest that more data should be systematically collected on the tensile strength of radial sheaths, preferably under challenging physiological/pathological conditions, as part of technological considerations. Methods of improving the strength of stress points in the sheaths should also be reviewed. It may be possible to reduce such sheath related complications, if systems based on smaller sheathless coronary catheters are widely used in future [11]. However, complications related to the fracture of long catheters via radial approach have also been reported [12]. At present, we encourage clinicians to report and record such rare adverse events related to sheaths, so that the true frequency of such events can be evaluated and the underlying pathophysiological/technological mechanisms understood. This will help determine the best possible course(s) of action for prevention and management, which in turn will further improve safety of TR coronary angiography.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪▪ Achieving procedural success in transradial coronary angiography/intervention and prevention of complications related to access-site, can depend on the successful management of radial artery spasm.
▪▪ Refractory radial artery spasm can lead to radial sheath retention, but the extreme possibility of retention and fracture of a hydrophilic sheath as reported by us, raises the issue of the need to assess the tensile strength of stress points of radial sheaths and systematic reporting of such rare complications. Additionally, radial operators, particularly those who are early in the learning curve, should be alerted to the means of managing such complications.
References
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomized, parallel group, multicenter trial. Lancet 377(9775), 1409–1420 (2011).
- Kiemeneij F, Vajifdar BU, Eccleshall SC, Laarman G, Slagboom T, van der Wieken R. Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheter. Cardiovasc. Interv. 58(3), 281–284 (2003).
- Rathore S, Stables RH, Pauriah M et al. Impact of length and hydrophilic coating of the introducer sheath on radial artery spasm during transradial coronary intervention: a randomized study. J. Am. Coll. Cardiol. Intv. 3, 475–483 (2010).
- Osman F, Buller N, Steeds R. Use of intra-arterial papaverine for severe arterial spasm during radial cardiac catheterization. J. Invasive Cardiol. 20(10), 551–552 (2008).
- Pullakhandam NS, Yang ZJ, Thomas S, Wasenko J. Unusual complication of transradial catheterization. Anesth. Analg. 103(3), 794–795 (2006).
- Barçin C, Kursaklioglu H, Köse S, Amasyali B, Isik E. Resistant radial artery spasm during coronary angiography via radial approach responded to local warm compress. Anadolu Kardiyol. Derg. 10, 90–91 (2010).
- Amoroso G, Sarti M, Bellucci R et al. Clinical and procedural predictors of nurse workload during and after invasive coronary procedures. Eur. J. Cardiovasc. Nurs. 4, 234–241 (2005).
- Doyle BJ, Rihal CS, Gastineau DA, Holmes DR Jr. Bleeding, blood transfusion and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J. Am. Coll. Cardiol. 53, 2019–2027 (2009).
- Yatskar L, Selzer F, Feit F et al. Access site hematoma requiring blood transfusion predicts mortality in patients undergoing percutaneous coronary intervention: data from the National Heart, Lung and Blood Institute Dynamic Registry. Catheter. Cardiovasc. Interv. 69, 961–966 (2007).
- Jolly SS, Amlani S, Hamon M et al. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
- Mizuno S, Takeshita S, Taketani Y, Saito S. Percutaneous coronary intervention using a virtual 3-F guiding catheter. Catheter. Cardiovasc. Interv. 75, 983–988 (2010).
- Lee Y, Tan HC, Lee C-H. Complete fracture of an Ikari guiding catheter in the axillary artery during transradial coronary intervention. Int. J. Angiol. 17(1), 40–42 (2008).
▪ Website
101 US FDA MAUDE database. www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMAUDE/search.CFM (Accessed 25 October 2011)