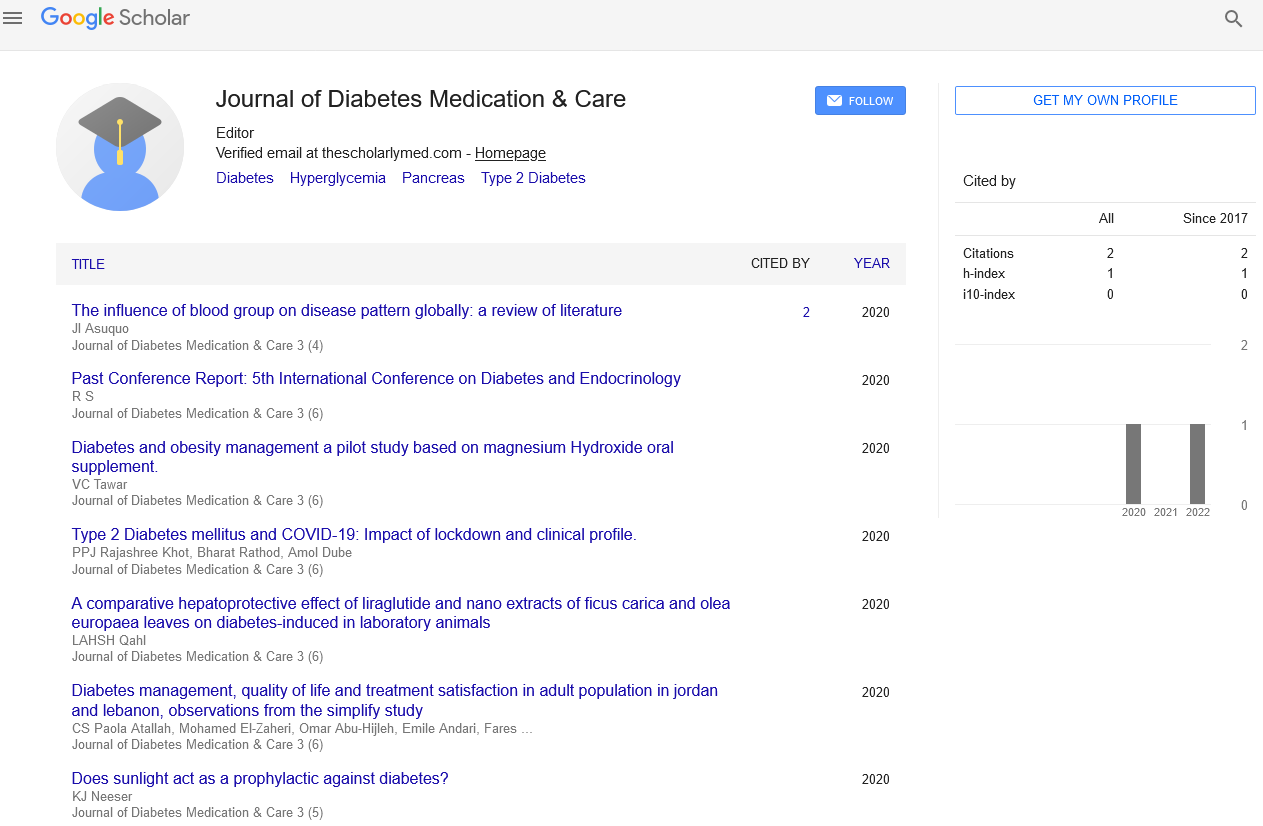
Perspective - Journal of Diabetes Medication & Care (2024) Volume 7, Issue 3
Rethinking Diabetes Management: GLP-1 Receptor Agonists as First-Line Injectable Therapy Over Basal Insulin
- Corresponding Author:
- Hong Cheng
Department of Internal Medicine, Fudan University, Fudan, China
E-mail: hongcheng@caas.cn
Received: 03-May-2024, Manuscript No. JDMC-24-136447; Editor assigned: 06-May-2024, PreQC No. JDMC-24-136447 (PQ); Reviewed: 20-May-2024, QC No. JDMC-24-136447; Revised: 29-May-2024, Manuscript No. JDMC-24-136447 (R); Published: 07-Jun-2024, DOI: 10.37532/JDMC.2024.7(3).210-211
Introduction
In the complex landscape of diabetes management, selecting the most appropriate injectable therapy can significantly impact patient outcomes and quality of life. Traditionally, basal insulin has been the go-to option when oral medications fail to control blood sugar levels adequately. However, emerging evidence suggests that GLP-1 Receptor Agonists (GLP-1RAs) may offer superior benefits as a first-line injectable therapy for certain patients. In this article, we explore the rationale behind this paradigm shift and the potential advantages of prioritizing GLP-1RAs over basal insulin in diabetes treatment.
Description
Understanding GLP-1 receptor agonists
GLP-1 receptor agonists are a class of injectable medications that mimic the action of Glucagon-Like Peptide-1 (GLP-1), a hormone produced by the intestine in response to food intake. GLP-1 plays a crucial role in regulating blood sugar levels by stimulating insulin secretion, inhibiting glucagon release, slowing gastric emptying, and promoting satiety. By activating GLP-1 receptors, GLP-1RAs enhance these physiological effects, leading to improved glycemic control and other metabolic benefits.
GLP-1RAs are available in various formulations, including short-acting and long-acting preparations, allowing for flexible dosing regimens to accommodate individual patient needs. These medications are typically administered via subcutaneous injection once daily or once weekly, depending on the specific agent and formulation. Commonly prescribed GLP-1RAs include exenatide, liraglutide, dulaglutide, semaglutide, and lixisenatide.
Rationale for prioritizing GLP-1RAs over basal insulin
Traditionally, basal insulin has been recommended as the first injectable therapy for patients with type 2 diabetes who fail to achieve glycemic targets with oral medications alone. However, several factors support reconsidering this approach in favor of prioritizing GLP-1RAs:
Weight management: Unlike basal insulin, which is associated with weight gain in many patients, GLP-1RAs have been shown to promote weight loss or weight neutrality. This is particularly beneficial for individuals with diabetes who are overweight or obese, as weight loss can improve insulin sensitivity, cardiovascular risk factors, and overall metabolic health.
Hypoglycaemia risk: GLP-1RAs have a lower risk of hypoglycaemia compared to insulin, especially when used as monotherapy or in combination with oral antidiabetic medications. By reducing the risk of hypoglycaemia, GLP-1RAs offer a safer and more predictable option for glycemic control, particularly in elderly patients or those with comorbidities.
Cardiovascular benefits: Several large-scale cardiovascular outcomes trials have demonstrated that certain GLP-1RAs provide significant cardiovascular benefits beyond glycemic control. These medications have been shown to reduce the risk of major adverse cardiovascular events, including heart attack, stroke, and cardiovascular death, making them an attractive option for patients with established cardiovascular disease or high cardiovascular risk.
Patient preference and adherence: GLP-1RAs are administered via subcutaneous injection, similar to insulin, but with less frequent dosing and a smaller needle size. This may be more appealing to patients who are reluctant to initiate insulin therapy due to fear of injections or concerns about regimen complexity. Improved adherence to treatment regimens can lead to better glycemic control and long-term health outcomes.
Clinical guidelines and recommendations
Recent updates to clinical guidelines and consensus statements reflect the growing recognition of the benefits of GLP-1RAs and their potential role as first-line injectable therapy in diabetes management. The American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) recommend considering GLP-1RAs as the preferred injectable option over basal insulin in patients with type 2 diabetes who have not achieved glycemic targets with oral medications alone.
Furthermore, the ADA/EASD consensus report on management of hyperglycemia in type 2 diabetes highlights the importance of individualizing treatment decisions based on patient preferences, comorbidities, and cardiovascular risk factors. For patients with atherosclerotic cardiovascular disease or heart failure, GLP-1RAs with proven cardiovascular benefits are recommended as part of the treatment regimen, regardless of baseline A1C levels.
Conclusion
The landscape of diabetes management is evolving rapidly, with a growing emphasis on personalized, evidence-based approaches to treatment. While basal insulin has long been considered the standard injectable therapy for patients with type 2 diabetes, emerging evidence suggests that GLP-1RAs offer distinct advantages in terms of weight management, hypoglycemia risk, cardiovascular benefits, and patient preference.
By prioritizing GLP-1RAs over basal insulin as the first-line injectable therapy in appropriate patients, healthcare providers can optimize glycemic control, minimize treatment-related complications, and improve patient adherence and satisfaction. As our understanding of diabetes pathophysiology and treatment options continues to advance, it is imperative to embrace novel therapeutic strategies that prioritize both efficacy and patient-centered care in the management of this complex chronic condition.