Case Report - Interventional Cardiology (2015) Volume 7, Issue 3
Retrograde approach to successfully treat antegrade failure due to subintimal hematoma of a right coronary artery chronic total occlusion
- Corresponding Author:
- Faisal Latif
1Department of Medicine
Cardiovascular Section
University of Oklahoma Health Sciences Center
OK, USA
E-mail: faisal-latif@ouhsc.edu
Abstract
Use of antegrade dissection re-entry techniques for crossing coronary chronic total occlusions may occasionally fail due to subintimal hematoma formation. We describe use of the retrograde approach to successfully complete a right coronary artery chronic total occlusion intervention, in which re-entry was not possible after subintimal guidewire crossing due to extensive subintimal hematoma formation that compressed the distal true lumen.
Use of antegrade dissection re-entry techniques for crossing coronary chronic total occlusions may occasionally fail due to subintimal hematoma formation. We describe use of the retrograde approach to successfully complete a right coronary artery chronic total occlusion intervention, in which re-entry was not possible after subintimal guidewire crossing due to extensive subintimal hematoma formation that compressed the distal true lumen.
Keywords
chronic total occlusion, percutaneous coronary intervention, retrograde technique
Antegrade dissection re-entry is an increasingly utilized crossing strategy for crossing coronary chronic total occlusions (CTOs), especially long occlusions as part of the ‘hybrid’ CTO crossing algorithm [1], and its use has been associated with high procedural success rates [2–5]. Re-entry into the distal true lumen after subintimal crossing can be challenging in some cases usually due to subintimal hematoma formation [6]. Several maneuvers have been developed to facilitate re-entry, such as the ‘stick and swap’ technique, use of a different re-entry zone (‘bobsled’) and subintimal hematoma aspiration using the subintimal transcatheter withdrawal (STRAW) technique [6]. We report a case of right coronary artery (RCA) CTO percutaneous coronary intervention (PCI) that was complicated by formation of a large subintimal hematoma and was successfully treated using the retrograde approach. Verbal informed consent was obtained from the patient.
Case description
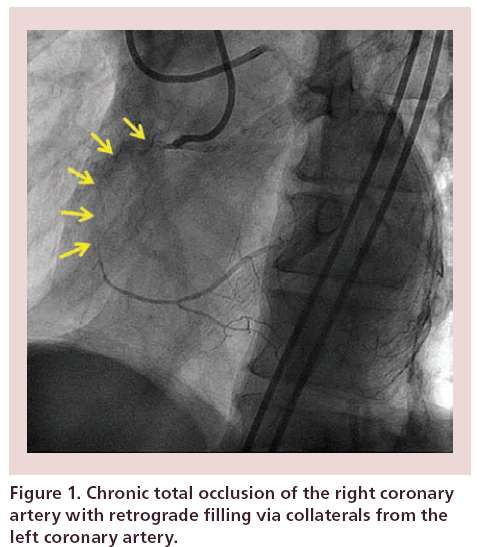
A 62-year-old man with oxygen-dependent severe chronic obstructive pulmonary disease, hypertension and dyslipidemia presented with non-ST-segment elevation acute myocardial infarction. Coronary angiography revealed a 70% stenosis in proximal left anterior descending artery (LAD) and a CTO of the RCA, with the right posterolateral branch filling via epicardial collaterals from the circumflex, and the posterior descending artery via septal collaterals from the LAD (Figure 1). The circumflex artery had a separate ostium and was normal. The patient had Canadian Cardiovascular Society class 3 anginal symptoms despite maximally tolerated guideline-directed medical therapy. He was not deemed a surgical candidate and was referred for RCA CTO and LAD PCI. Bifemoral access was obtained and unfractionated heparin was used for anticoagulation. An 8-French AL-1 guide was used to engage the RCA, while an 8-French EBU-4 guide catheter was used to engage the LAD.
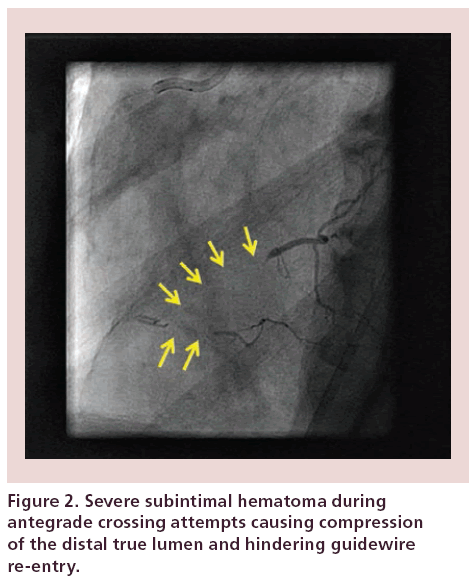
Antegrade crossing was challenging because the proximal RCA segment was very short. Support improved using a side branch anchor balloon in the conus branch with a 1.5-mm balloon inflated at low pressure. A Confianza Pro 12 guidewire (Asahi Intecc, Nagoya, Japan) entered the subintimal space, but could not advance further. After high-pressure inflation of a 3.0 × 20 mm balloon, a knuckled Fiedler XT guidewire (Asahi Intecc) followed by a CrossBoss catheter (Boston Scientific, MA, USA) subintimally crossed to the distal RCA. Attempts to re-enter using a Stingray system (Boston Scientific) failed, as did use of the ‘stick and swap’ technique (re-entry with a Pilot 200 guidewire after initial puncture with the Stingray guidewire) due to subintimal hematoma formation and distal true lumen compression (Figure 2). Attempts to re-enter more distally in the vessel also failed. A second guidewire was advanced into the subintimal space and a 2.0 × 15 mm over-the-wire balloon was used to aspirate approximately 10 cc of frank blood (STRAW) technique. However, repeat attempts to re-enter failed.
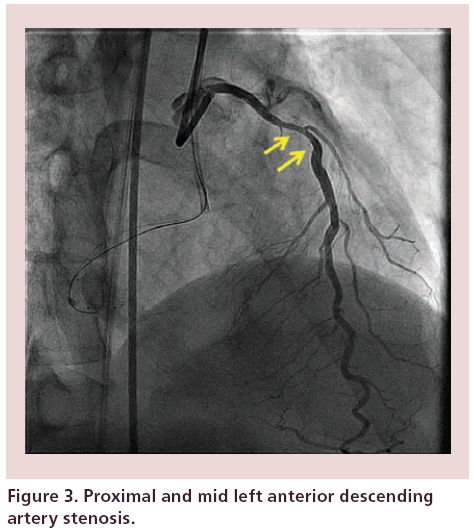
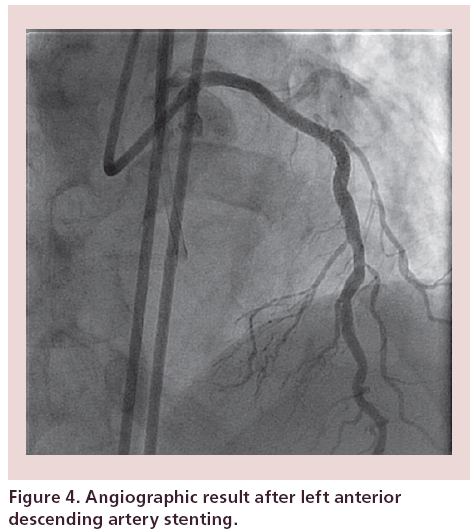
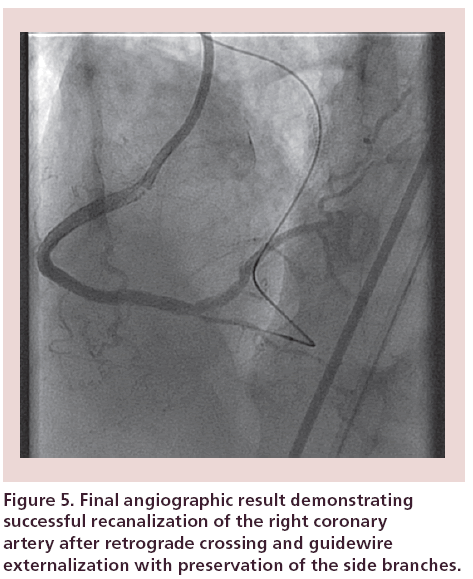
The retrograde approach was subsequently attempted after stenting the mid LAD lesion (Figure 3) with a 3.5 × 24 mm Promus Premier (Boston Scientific, Natick, MA) stent, yielding excellent results (Figure 4). The procedure was performed at a single stage because we had used 180 cc of contrast in a patient with normal renal function and patient air kerma radiation dose was <2 Gy. The first septal branch was successfully crossed with a Sion guidewire (Asahi Intecc), followed by advancement of a Corsair catheter (Asahi Intecc) into the distal RCA. The wire was exchanged for a Pilot 200 guidewire (Abbott Vascular) that was advanced subintimally into mid-RCA. Because of the short patent proximal RCA segment, we used the Guideliner-assisted reverse controlled antegrade and retrograde dissection technique for retrograde crossing [7], using an 8-French Guideliner (Vascular Solutions, MN, USA) advanced to the mid RCA. A retrograde Pilot 200 guidewire was advanced into the Guideliner catheter (Vascular Solutions), followed by externalization of an R350 guidewire (Vascular Solutions). Then, proximal to distal RCA was dilated using a 3.0 × 20 mm balloon and three drugeluting stents were deployed in a distal to proximal fashion (2.5 × 16 mm, 2.5 × 38 mm and 3.0 × 38 mm Promus Premier [Boston Scientific]) and were postdilated with a 3.5 × 20 mm noncompliant balloon at 15–18 atm. Final angiography revealed an excellent result with TIMI-3 RCA flow, and no residual stenosis (Figure 5). Radiation dose (air kerma) was 2.1 Gy and approximately 400 cc of contrast was used.
Discussion
To the best of our knowledge, this is the first report of retrograde CTO PCI to overcome failure of antegrade crossing due to subintimal hematoma formation.
Patients who present with acute myocardial infarction (with [8] or without [9] ST-segment elevation) have higher mortality when they have a concomitant CTO in the noninfarct-related artery. Our patient presented with non-ST-segment elevation myocardial infarction; since he was not a surgical candidate, complete revascularization including PCI of the CTO likely decreased his risk for recurrent cardiovascular events.
Antegrade dissection re-entry is commonly utilized to cross long (>20 mm) coronary CTOs, often as an upfront strategy [1,6]. It is a highly efficient method for CTO crossing, however, it is subject to unique challenges, such as failure to enter the subintimal space or failure to re-enter into the distal true lumen after subintimal guidewire crossing. Both challenges were encountered in the present case. Entry into the subintimal space could not be easily achieved, requiring a proximal dissection by inflation of a 3.0-mm balloon. Re-entry could not be completed due to formation of a large hematoma, in spite of using several advanced techniques, such as attempt to re-enter in different vessel locations (‘bobsled’) and the ‘stick and swap’ technique, in which an initial puncture with the stiff Stingray guidewire is followed by a polymer-jacketed Pilot 200 guidewire [6]. Attempts to aspirate the hematoma (‘STRAW’ technique) also failed.
The retrograde approach has revolutionized CTO PCI by significantly increasing procedural success, even among very complex CTOs [10–12]. The retrograde approach can be used as the initial crossing strategy in CTOs with ambiguous proximal cap or very diffusely diseased distal vessel, or more commonly, after failure of antegrade crossing [1]. It has also been used to salvage side branches after antegrade CTO crossing into one branch of a bifurcation [13], as well as in cases of acute myocardial infarction with failed antegrade crossing [14]. In our case, the retrograde approach enabled wiring of the distal true lumen and resolution of the subintimal hematoma after stent deployment. Use of the retrograde approach necessitates availability of adequately sized collateral vessels as well as expertise in the retrograde equipment and techniques. The retrograde approach is subject to unique risks, such as collateral vessel perforation and donor vessel dissection [6,15]. Moreover, use of the retrograde approach should be considered early during the case, before the contrast and radiation limits are reached.
In summary, use of the retrograde approach can enable successful CTO crossing in cases of failed re-entry during subintimal antegrade crossing.
Conclusion and future perspective
This report demonstrates that subintimal hematoma should not deter operators from pursuing a retrograde approach, as successful recanalization can still be achieved. CTO PCI techniques have evolved considerably over the last few years with improved success rates and granting of an ‘appropriate’ status in patients with high-risk noninvasive testing or high-grade angina symptoms. Intraprocedural technical issues, such as a subintimal hematoma in our case, are being overcome successfully with newer techniques. Over the next 5–10 years, the field of CTO PCI will progress where patients, who are not candidates for coronary bypass grafting, can still undergo complete revascularization, which will improve symptoms as well as major adverse cardiovascular events such as hospitalizations due to acute coronary syndromes.
Financial and competing interests disclosure
ES Brilakis received consulting honoraria/speaker fees from Sanofi, Janssen, St Jude Medical, Terumo, Asahi, Abbott Vascular, Elsevier and Boston Scientific; research grant from Guerbet; and his spouse is an employee of Medtronic. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Informed consent disclosure
The authors state that they have obtained verbal and written informed consent from the patient/patients for the inclusion of their medical and treatment history within this case report.
Executive summary
• A subintimal hematoma should not preclude the retrograde approach.
• Utilize subintimal transcatheter withdrawal technique to reduce the size of subintimal hematoma and attempt re-entry.
• Switch from ante- to retrograde approach should be time efficient to prevent overuse of radiation and contrast.
References
Papers of special note have been highlighted as:
• of interest; •• of considerable interest
- Brilakis ES, Grantham JA, Rinfret S et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc. Interv. 5, 367–379 (2012).
- Michael TT, Papayannis AC, Banerjee S, Brilakis ES. Subintimal dissection/reentry strategies in coronary chronic total occlusion interventions. Circ. Cardiovasc. Interv. 5, 729–738 (2012).
- Christopoulos G, Menon RV, Karmpaliotis D et al. The efficacy and safety of the “hybrid” approach to coronary chronic total occlusions: insights from a contemporary multicenter US registry and comparison with prior studies. J. Invasive Cardiol. 26(9), 427–432 (2014).
- Michael TT, Mogabgab O, Fuh E et al. Application of the “hybrid approach” to chronic total occlusion interventions: a detailed procedural analysis. J. Interv. Cardiol. 27, 36–43 (2014).
- Pershad A, Eddin M, Girotra S, Cotugno R, Daniels D, Lombardi W. Validation and incremental value of the hybrid algorithm for CTO PCI. Catheter Cardiovasc. Interv. 84(4), 654–659 (2014).
- Manual of coronary chronic total occlusion interventions. In: A Step-By-Step Approach. Brilakis ES (Ed.). Elsevier, MA, USA (2013).
- Vo M, Brilakis ES. Faster, easier, safer: “guideliner reverse CART” for retrograde chronic total occlusion interventions. Catheter Cardiovasc. Interv. 83, 933–935 (2014).
- Claessen BE, Dangas GD, Weisz G et al. Prognostic impact of a chronic total occlusion in a non-infarct-related artery in patients with ST-segment elevation myocardial infarction: 3-year results from the HORIZONS-AMI trial. Eur. Heart J. 33, 768–775 (2012).
- Gierlotka M, Tajstra M, Gasior M et al. Impact of chronic total occlusion artery on 12-month mortality in patients with non-ST-segment elevation myocardial infarction treated by percutaneous coronary intervention (from the PL-ACS registry). Int. J. Cardiol. 168, 250–254 (2013).
- El Sabbagh A, Patel VG, Jeroudi OM et al. Angiographic success and procedural complications in patients undergoing retrograde percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 3482 patients from 26 studies. Int. J. Cardiol. 174, 243–248 (2014).
- Brilakis ES, Grantham JA, Thompson CA et al. The retrograde approach to coronary artery chronic total occlusions: a practical approach. Catheter Cardiovasc. Interv. 79, 3–19 (2012).
- Karmpaliotis D, Michael TT, Brilakis ES et al. Retrograde coronary chronic total occlusion revascularization: procedural and in-hospital outcomes from a multicenter registry in the United States. JACC Cardiovasc. Interv. 5, 1273–1279 (2012).
- Kotsia A, Christopoulos G, Brilakis ES. Use of the retrograde approach for preserving the distal bifurcation after antegrade crossing of a right coronary artery chronic total occlusion. J. Invasive Cardiol. 26, E48–E49 (2014).
- Patel VG, Zankar A, Brilakis E. Use of the retrograde approach for primary percutaneous coronary intervention of an inferior ST-segment elevation myocardial infarction. J. Invasive Cardiol. 25, 483–484 (2013).
- Brilakis ES, Karmpaliotis D, Patel V, Banerjee S. Complications of chronic total occlusion angioplasty. Interventional Cardiol. Clinics 1, 373–389 (2012).
• Describes the ‘hybrid’ approach to chronic total occlusion (CTO) percutaneous coronary intervention, and forms the basis for contemporary CTOs percutaneous coronary intervention (PCI) in the USA and increasingly around the world.
• Discusses how the use of both antegarde and retrograde approaches complement each other and improves chances of successful PCI.
•• Is an excellent primer for CTO PCI. It details the various aspects of these complex procedures in an easy to follow sequence.
• This case report details the steps involved in the reverse controlled antegrade and retrograde tracking technique to safely and successfully complete PCI using the retrograde approach.
•• Provides a practical, step-by-step description of the procedural steps needed for the retrograde approach.
•• This case report demonstrates how the retrograde approach can be used to maintain patency of a side branch that becomes compromised during antegrade CTO crossing.