Research Article - Clinical Practice (2018) Volume 15, Issue 1
Risk of pressure ulcer in hospitalized patients after stroke: relation of nutritional factors and of morbidity
- Corresponding Author:
- Elisângela Colpo
Department of Nutrition
Center Franciscan University
Santa Maria, Brazil
E-mail: elicolpo@yahoo.com.br
Abstract
Introduction: Hospitalized patients after stroke stay more time bedridden, what increases the risk of developing Pressure Ulcer (PU). Objective: To verify which nutritional and morbidity parameters are more associated to the risk of pressure injury development in hospitalization of patients after stroke. Methodology: Cross-sectional descriptive study, with sample composed by 52 old adults hospitalized after stroke. The patients were submitted to nutritional evaluation in until 72 hours after the date of hospitalization, which was composed by anthropometric as weight, height, BMI, circumference and skinfold; biochemistry (albumin, hemogram, urea, creatinine, C-reactive protein) and dietetic. As parameters of morbidity were evaluated number and type of stroke, presence of deglutition disorders and anemia. Braden scale was applied to evaluate the risk of PU development. It was applied One-way ANOVA followed of Tukey to comparisons of average of categorizations. Results: Patients who did not presented deglutition disorders (27%, n=14) had less risk of developing PU in relation to patients with deglutition disorders (73%, n=38, p=0.0002). Patients with moderate risk of developing PU had serum albumin and hemoglobin levels statistically lower when compared to low risk patients (p=00.49, p=0.012, respectively). Analyzing these patients anemia type, it was suggested anemia for nutritional deficit, since that the Red Cell Distribution Width (RDW) was elevated and the mean corpuscular volume was normal. Conclusion: According to the results, it was observed an important association of biochemistry and dietetic parameters with the risk of PU development. It was not observed any association of anthropometric parameters with the risk of PU. The presence of anemia and deglutition disorders should be monitored, because they have a relation with PU development. The hospitalized patient nutritional monitoring is necessary in order to decrease the presence of medical complications and readmissions of patients after stroke.
Keywords
neurological diseases, braden scale score, undernutrition, humans, hospitalized patients, nutritional status, deglutition disorders, anemia
Introduction
From 2001 to 2011, the rates of stroke decreased to 31% and the real number of stroke decreased to 21.1%. However, each year, 795,000 individuals present a new or recurrent stroke, being ischemic or hemorrhagic stroke. About 610,000 of these are first episodes and 185,000 are recurrent of stroke. The incidence in 2011 in the United States caused 1 to each 20 deaths for stroke, where to each 40 seconds someone presents a stroke and 1 to each 4 minutes dyes [1].
According to the World Health Organization (WHO), the mortality rates have decreased in Brazil, but even that it still keeps being the first cause of death and inability in the country. According to national data, the annual incidence is of 108 cases per 100,000 habitants [2]. Several factors contribute to development of stroke, such as age, gender, systemic arterial hypertension, dyslipidemia, diabetes mellitus, smoking, obesity, stress, sedentary lifestyle and alcoholism. However, the decrease of mortality in the last decades is related to improvements in interventions of cardiovascular factors control [1].
According to World Stroke Organization (WSO) (2014) [3], stroke is classified in ischemic and hemorrhagic. The most frequent is hemorrhagic stroke, with about 87% of the cases, characterized by arterial obstruction in a determinate encephalon area, caused by thrombi or emboli. Hemorrhagic stroke is responsible for 13% of the cases, in which occurs an abnormal bleeding to inside of the brain extravascular areas, causing aneurysm or trauma. The stroke incidence prevails in middle age adults and elderlies, being larger after 65 year-old, occurring high risk after 55 year-old.
Affected patients by neurological diseases stay more time restrict to hospital bed, what decreases their mobility and increases the risk of developing pressure ulcer. Patients with this profile have a diminished consciousness level and are unable to relieve bone prominence pressures, keeping, this way, intensity and duration of the pressure on the tissues [4,5]. PU is localized damage to the skin and underlying soft tissues, usually painful, of hard cicatrization. Its etiology presents extrinsic factors, such as, pressure, shear, friction, maceration; and intrinsic ones such as, immobility in bed, age, undernutrition, bad perfusion, presence of chronic diseases, comorbidity, among others [5]. The instrument Braden Scale is periodically applied to prevent the PU development in hospitalized patients. It is the most used method in international level for prevention, identification and classification of PU risk [6,7].
Studies have showed that undernutrition and PU are complications after stroke, increasing morbidity and mortality. Still there are few studies about the association between PU and stroke. However, due to physical and psychological consequences present after stroke, the patient stays more time hospitalized, increasing the chance of undernutrition because the low dietary intake and anorexia, with consequent metabolic stress and immunity decreasing, what can cause PU [8].
Researches indicate that an inadequate nutritional status retards the cicatrization, due to reduction of fibroblasts, angiogenesis and collagen synthesis, besides less capacity of tissue remodeling [9,10]. Anemia can predispose the emergence of PU, for occurring oxygen reduction to fibroblasts, making difficult the collagen formation and resulting the damaged tissue increase [11]. Nutritional evaluation is important, because through that, it is possible to make a nutritional diagnosis based on clinical, dietetic, anthropometric and biochemical history of the patient.
Usually, after stroke patients present deglutition disorders. It is known that this association is directly linked to the individual general health commitment, what may cause pneumonia, dehydration, undernutrition, and also can result in an increase in time of hospitalization [12]. An early identification of deglutition disorders is relevant, since it can reduce the risk of co-morbidities, undernutrition and mortality [13].
This way, a nutritional evaluation contributes to the nutritional deficit investigation [14]. Therefore, the early nutritional intervention and the PU risk evaluation become vital, inasmuch as they help in the treatment efficiency, decreasing the undernutrition and PU risk, thus, reducing hospital complication rates and hospitalization time as consequent improvement in these patients’ quality of life and cost reduction related to health services [4-8]. In such way, this study had as objective to verify what nutritional and of morbidity parameters are more associated with the risk of PU in after stroke patients hospitalization.
Methodology
It is about a cross-sectional descriptive prospective study with quantitative approach. The research was performed in a public hospital in Santa Maria, RS, from August to December of 2016. The sample was by convenience, composed by adults and elderlies hospitalized after stroke, which were fed orally and/or enteral nutrition, ambulant or not. The stroke and deglutition disorders diagnosis were performed by a physician and a speech therapist, respectively, and collected in the patients records. Stroke was diagnosed by computed tomography and magnetic resonance. The adopted exclusion criteria were the following: patients with parenteral nutrition, sepsis, anasarca or who did not have conditions of being submitted to anthropometric evaluation.
To analyze the nutritional parameters, the patients were submitted to an evaluation in until 72 hours after the hospitalization date, being composed by: anthropometry, biochemistry and dietetic. To occur a standardization of nutritional evaluation, the researcher had training in an anthropometric evaluation laboratory.
The patients’ weight was verified in an analogue scale Sul Fitness™ with capacity of 150 Kilograms (kg) and the height was set from a mobile rod stadiometer. When it was not possible weight the patients in the scale or height them with the stadiometer, it was realized a weight estimate second Rabito [15] or Chumlea [16] and the recumbent height according to Gray [17].
The circumferences, half arm span, knee height, found in the formulas were gauged by a tape measure and tricipital skinfold (TSF) and subscapular skinfold (SSF) were gauged by a scientific adipometer Cescorf ™.
The procedures to gauging of the mid upper arm circumference (MUAC), calf, TSF, and SSF were performed according to Martins [14]. The calf circumference is considered a muscle reserve marker, however, there are few studies proving that this measure indicates a nutritional risk or undernutrition. Values fewer than 31 centimeters indicate muscle depletion in elderly people [18].
The body mass index (BMI) was obtained from the actual weight, in Kg, divided by height2 in meters (Kg/m2). The nutritional status in adults was classified second the World Health Organization [19] criteria. Nevertheless, the BMI in elderlies was classified according to Lipschitz [20], being defined with the different cut points proposed to the classification.
The used biochemical parameters were analyzed according to each healthcare center in which the patient attended to, being considered hemogram, albumin, urea, creatinine and CRP. The blood counting was performed by a licensed professional of the hospital clinical analyzes laboratory (CAL). These exams were evaluated and interpreted according to the reference values of the hospital lab.
The acceptance of both diet by oral as by enteral way was evaluated in the following way: dietary intake or enteral nutrition infusion >75%: good acceptance; average dietary intake of 50% or enteral nutrition infusion of 50%: medium acceptance; dietary intake <25% or enteral nutrition infusion lesser then 25%: low acceptance.
To evaluate the morbidity parameters were analyzed the stroke type and number, the presence of deglutition disorders and anemia, as well as its severity, being classified according to WHO [21], with the following cut points: to men >13 g/dL without anemia; 11 to 12.9 g/dL mild anemia; 8 to 10.9 g/dL moderate anemia; <8 g/dL severe anemia. To women >12 g/dL without anemia; 11 to 11.9 g/dL mild anemia; 8 to 10.9 g/dL moderate anemia; <8 g/dL severe anemia.
The data to evaluate the risk of pressure ulcer development were collected from the Braden scale recorded by the hospital nursing team. The scale was applied according to the risk presented, that is, without risk patients, classified in the score >15 points, and was applied each 24 hours.
The Braden scale has scores that vary from 6 to 23 points and is subdivided in sub-scales. These scores evaluate the following points: sensorial perception, humidity, mobility, nutrition, friction, and shear of the patient’s skin with the bed. Each scale sub item has from 1 to 4 scores. The interpretation is realized in accordance to the score, in which the lesser score, the high the risk of developing PU [7].
The study was approved by the ethics and research committee of the Franciscan University, through the CAAE (Certificate of Presentation for Ethical Consideration) number 51109315.4.0000.5306. The patients or responsible were invited to participate in the research in a voluntary way. The data collect only started after they had signed the consent form (CF).
To associate the PU risk with nutritional and morbidity parameters were categorized the following analyzes: BMI according to age, adults and elderlies, respectively: low weight was considered BMI under 18.5 or 22; eutrophy between 18.5 to 24.9 or 22 to 27; overweight with BMI above 25 or 27. The albumin was classified according to the severity degree: 3.5 g/dL without depletion; 3.0 to 3.5 g/dL mild depletion; 2.4 to 2.9 g/dL moderate depletion; <2.4 g/dL severe depletion [22]. The Braden score was classified according to the severity degree, that is, hospitalized patients with score >16 points were considered with low risk to development of PU, while the scores <11 pointed high risk. The classifications were categorized in the following way: score >16 low risk; score between 13 and 14 moderate and <11 high risk.
Data are expressed as mean +SD. It was applied One-way ANOVA followed of Tukey to comparisons of average of categorizations, besides the relative frequency. Differences were considered significant at P<0.05.
Results
Seventy-seven hospitalized stroke patients initially composed the sample. Fifteen patients were excluded: eight were found swollen, two with hypothesis of stroke diagnosis, three with diagnosis of sepsis and two were found in bed with no companion and enable to sign the CF. This way, 52 patients participated in the study, with average age of 64 ± 14 years-old, being 69.2% (n=36) elderlies and 30.8% (n=16) adults, being 67.3% male and 32.7% female.
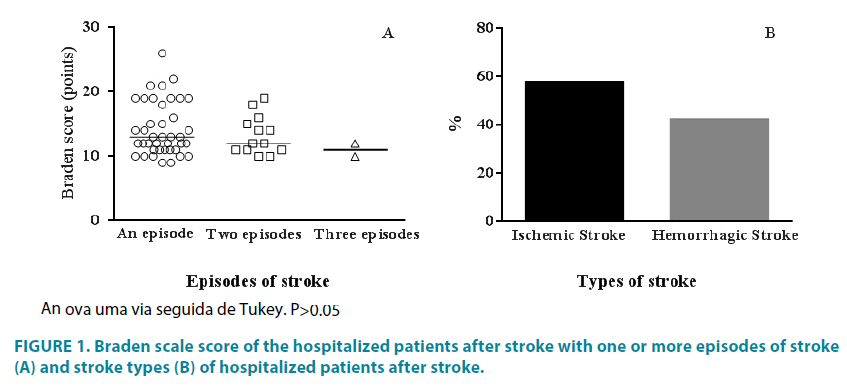
The most prevalent risk factors in the studied sample to developing stroke was hypertension, with 73% (n=38); diabetes mellitus (DM), with 31% (n=17); dyslipidemia 28.84% (n-15). In the present study, the most part of patients presented an episode of stroke (76%) (FIGURE 1A). In FIGURE 1B and 42.3% hemorrhagic stroke. In FIGURE 1B, 57.7% (n = 30) of the patients presented diagnosis of ischemic stroke and 42.3% (n=22) hemorrhagic stroke. The most part of patients presented physical and/ or mental sequels, that is, 69% (n=36) of the patients were found in bed and 31% (n=16) walking. From the studied sample 9.6% (n=5) presented PU in the hospitalization.
According to the PU risk classification, 32.7% (n=17) of the patients were hospitalized with low PU risk; 63% (n=33) with moderate risk and 3.8% (n=2) with very high risk of developing PU. In agreement with Braden scores it was observed that 34% (n-17) of the patients presented completely limited sensorial perception; 82% (n=41) were occasionally wet; 69% (n=36) were found in hospital bed; 38% (n=19) with very limited mobility; 76% (n=38) with probably adequate nutrition and 42% with friction and shear problems.
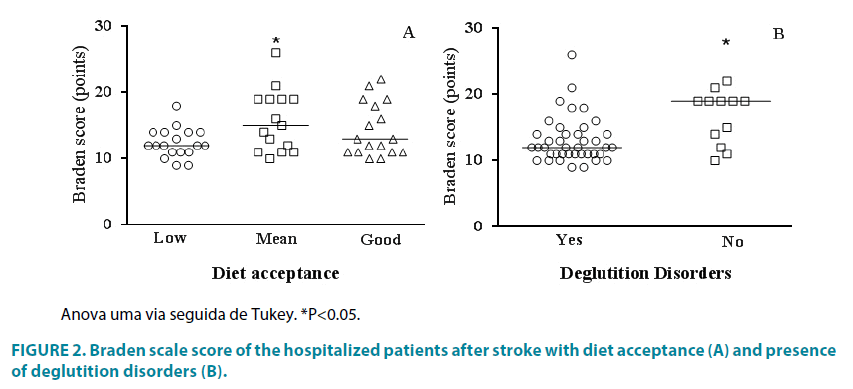
In relation to diet acceptance in the hospitalization, 37% (n=19) referred medium acceptance; 29% (n=15) presented low acceptance and 34% (n=18) presented good one. When associated the diet acceptance with the risk of developing PU, the patients with medium acceptance presented significant PU risk (15.7 ± 4.6 points) lower than patients with low diet acceptance (12.4 ± 2.2 points; p=0.034), according to FIGURE 2A.
When associated the presence of deglutition disorders and the PU risk (FIGURE 2B), the patients who did not present deglutition disorders (27%; n=14) had significant PU risk lesser than those who had it (73%; n=38; p= 0.0002). In the present study, 55.8% (n=29) of the patients were found with exclusive Enteral Nutritional Therapy (ENT); 36.5% (n=19) with oral feeding; 7.7% (n=4) with oral associated to ENT.
Figure 2: Braden scale score of the hospitalized patients after stroke with diet acceptance (A) and presence of deglutition disorders (B).
In relation to anthropometric evaluation, the most part of the patients were hospitalized with no nutritional risk. In agreement with the BMI classification, 44.2% were found eutrophy, 40.4% (n=21) with overweight and 15.4% (n=8) with low weight. When associated anthropometric parameters with weight, BMI, calf circumference and MUAC adequacy, it was not observed statistically significant associations with the PU risk development (data not show). These results can be associated to the fact of the majority of the patients, when hospitalized, did not present undernutrition second BMI (84.6%; n=44), did not present lean body mass depletion according to calf circumference (78.8%; n=41) or adequacy of arm muscle circumference (86.5%; n=45).
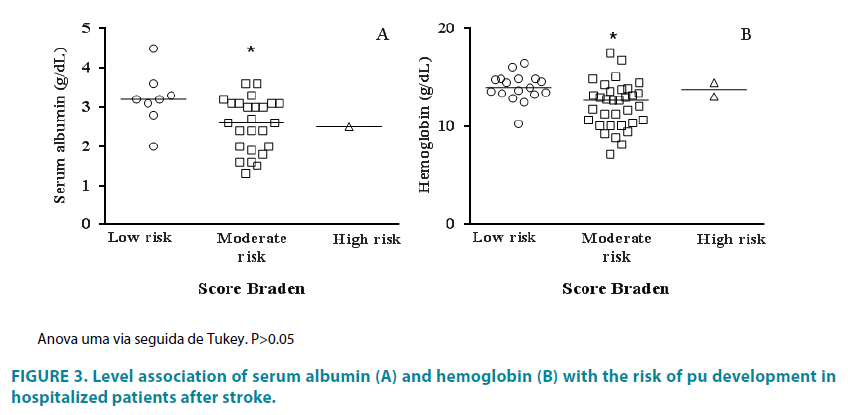
In accordance with the albumin serum levels categorization, just 12% (n=4) of the studied sample did not present depletion; 38% (n=13) mild depletion; 29% (n=10) moderate depletion; and 21% (n=7) severe depletion. In relation to the presence of anemia, according to the hemoglobin, 67% (n=35) of the patients did not present it, 10% (n=5) mild anemia and 23% (n=12) moderate anemia.
When associated the Braden scale with serum albumin and the hemoglobin levels, it was observed that low PU risk patients presented medium values of serum albumin 3.2 ± 0.7 g/ dL and hemoglobin 14 ± 1.4 g/dL. Moderate risk patients presented average of 2.5 ± 0.7 g/ dL of serum albumin and 12.2 ± 2.3 g/dL of hemoglobin. In patients classified with high risk of developing PU the average values of albumin were 2.5 ± 0.0 and hemoglobin 13.8 ± 0.9 g/ dL (FIGURE 3). The results were statistically significant when compared the moderate PU risk with moderate hypoalbuminemia (p= 0.049) and moderate anemia (p= 0.012). Few individuals were classified with high PU risk in relation to serum albumin and hemoglobin. Probably for this reason, the results were not statistically significant.
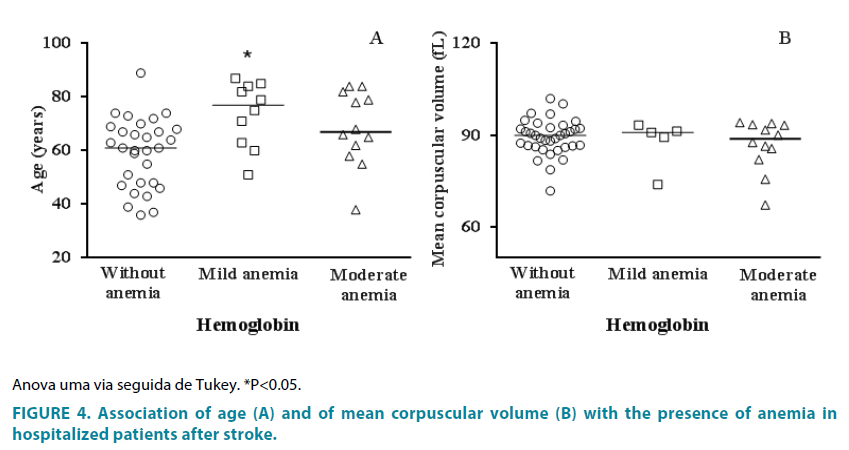
Analyzing the association between the presence of anemia with age and mean corpuscular volume (MCV), the patients without anemia had an age average of 60.8 ± 13.7 years and MCV of 89.4 ± 5.9 fL and with moderate anemia an average of 68.1 ± 8.3 fL. The patients without anemia were younger than the patients with mild anemia were (p= 0.038), according to FIGURE 4A. According to the erythrogram, the majority of the sample presented values of BMI inside the normality (80-95 fL) regardless the anemia classification, in accordance with FIGURE 4B.
Figure 4: Association of age (A) and of mean corpuscular volume (B) with the presence of anemia in hospitalized patients after stroke.
The patients without anemia had RDW average values of 13.6 ± 1.1%; with mild anemia of 15.4 ± 2.5% and with moderate anemia presented average of 16.2 ± 2.2%, being increased in patients classified with mild and moderate anemia (RDW reference values; 11.5 – 14.5%). Analyzing RDW values, the patients classified with mild and moderate anemia had the values increased. However, high RDW values with normal BMI can indicate a possible anemia beginning for nutritional deficit. The consumption of micronutrients as vitamin B12, folic acid and iron are necessary to prevent anemia for nutritional deficit.
Discussion
In the present study could be observed that the most part of the patients were male elderly people. According to Cerasuolo [23], the stroke incidence has kept constant for more than 12 years between people with age of 20 to 49 year-old and has decreased to over 50 year-old people. The incidence rate in relation to gender is higher in men than in women.
Due to physical and/or mental sequels present in stroke, the patient can exhibit a series of severe complications such as immunity reduction, predisposition to infection, anemia, hypoalbuminemia, PU and other complications that favor the difficulty of recovering, increasing the hospitalization time and the functional inability after hospitalization [24,25].
When associated the stroke episodes with PU risk development, it was observed that patients with one episode presented lower risk than the others who presented two or three stroke episodes. However, these data were not statistically significant and only two patients were hospitalized with three episodes.
Related to stroke type, the found data were associated to Smith [26], in which the study evidenced ischemic stroke as the most frequent, with 82.4% of the cases and only 27.2% of hemorrhagic stroke. Physical and/or mental inability that the patient can present after stroke depends of the stroke number and type. In this study could be observed that these patients exhibited some physical and/or mental sequel, since the majority was found restricted to the hospital bed. Due to these consequences, these patients can exhibit difficulties in evaluating the pressure on bone prominences favoring the emergence of PU.
According to the PU risk classification, it can be seen that these patients are a risk group to developing PU, since the majority presented moderate PU risk in the hospitalization, being an aggravating factor to PU development during the stay of these patients in the hospital.
Analyzing the sub-scales and Braden scores, the results linked with the study by Menegon [27], in which 39% of the hospitalized patients with cerebrovascular diseases were found with very limited mobility; pretty much wet; with very limited sensorial perception; with friction and shear problems. Besides that, it was observed the patients with stroke diseases had good scores referred to nutrition (probably adequate or excellent) and this could be related to disease acute phase, in which the patient still was found in a good state nutritional.
When associated the deglutition disorders and the risk of developing PU, the presence of deglutition disorders compromises deglutition, damaging the food consumption. Despite of the majority of the patients did not present low diet acceptance in hospitalization, deglutition disorders can affect negatively the acceptance on diet during hospitalization, increasing the chances of these patients developing undernutrition and PU.
The enteral nutrition therapy is necessary when the clinical conditions related to deglutition were compromised [4]. The enteral nutrition has as objective to offer needed nutrients to patients, in order to guarantee the adequate nutritional intake and prevent the clinical undernutrition. Nevertheless, the early enteral nutrition indication in patients enable of feeding orally does not happen, damaging the receipt of caloric/protein daily needs.
In the present study, the majority of the patients hospitalized without nutritional risk second BMI classification, calf circumference and arm circumference. These anthropometric parameters also were not statistically associated with PU risk and this can be by the fact of the after stroke patients show low nutritional risk in hospitalization. However, the anthropometric parameters monitoring is important to evaluate the patients’ nutritional status, because during hospitalization, the risk of undernutrition and PU can increase.
The hospitalization time of the after stroke patients was 20 ± 18 days with minimal time of two days and maxim of 72 days. The time hospitalization average of after stroke patients was related with the study by Duarte [28], in which was observed that patients with a period of hospitalization more than 15 days presented high nutritional risk, since they had significant weight loss in this time interval.
In the moment of hospitalization the most part of the patients did not present anemia diagnosis, presented light hypoalbuminemia and low nutritional risk second the classification of BMI, calf circumference and MUAC adequacy, despite of the majority of the sample is hospitalized with moderate risk of developing PU.
Studies show that hypoalbuminemia and low levels of hemoglobin/hematocrit increase the risk of PU emergence [29] and are related to mortality increase after stroke [30,31]. In the study of Satoshi [32], were evaluated patients with acute ischemic stroke. According to the results, anemia was associated with mortality after ischemic stroke, regardless the low weight and the low albumin level. As already discussed throughout this study, the nutritional deficits, inadequate nutritional status, low levels of hemoglobin and albumin can increase the risk of PU emergence and are related with the increase of mortality after stroke.
Conclusion
In summary, it was observed an important association of the biochemical and dietetic parameters with the risk of PU development. However, anthropometric parameters as weight, BMI, MUAC adequacy and calf circumference were not associated with PU risk. The presence of anemia and deglutition disorders should be monitored, because they have an important relation with the PU development. This way, the nutritional monitoring of the hospitalized patient is necessary to performing early nutritional interventions, in order to decrease the presence of complications, morbidity, mortality and readmissions of after stroke patients.
References
- MozaffarianD, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics - 2015 update: a report from the American Heart Association. Circulation 131, 29-322 (2015).
- Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de AçõesProgramáticasEstratégicas. Diretrizes de atenção à reabilitação da pessoa com acidente vascular cerebral / Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de AçõesProgramáticasEstratégicas. Brasília: Ministério da Saúde (2013).
- World Health Organization. Stroke, cerebrovascular accident. Available in: http://www.worldstrokecampaign.org/pt_br/learn/types-of-stroke.html. Accessed: July, 2017.
- Lee SY, Chou CL, Sanford PC, et al. Outcomes after Stroke in Patients with Previous Pressure Ulcer: A Nationwide Matched Retrospective Cohort Study. J. Stroke Cerebral Dis. 25(1), 220-227 (2016).
- National Pressure Ulcer Advisory Panel. Pressure Ulcer Stages Revised. Washington (2016). Available in: http://www.npuap.org/about-us/.
- Cox J Predictive power of the Braden Scale for pressure sore risk in adult critical care patients: a comprehensive review. J. Wound Ostomy. Continence Nurs. 39(6), 613-621 (2012).
- Wound Ostomy and Continence Nurses Society. Guideline for the Prevention and Management of Pressure Ulcers. Mount Laurel, NJ: Wound,Ostomy and Continence Nurses Society (2010).
- Zang J, Zhao X, Wang A, et al. Emerging malnutrition during hospitalization independently predicts poor 3-month outcomes after acute stroke: data from a Chinese cohort. Asia Pac. J.Clin.Nutr. 24(3), 379-386 (2015).
- Collins CE., Kershaw J, Brockington S. Effect of nutritional supplements on wound healing in home nursed elderly: a randomized trial. Nutrition 21,147-55 (2005).
- Desneves KJ, Todorovic BE, Cassar A, et al. Treatment with supplementary arginine, vitamin C and zinc in patients with pressure ulcers: a randomized controlled trial. Clin.Nutr. 24, 979-987 (2005).
- Raffoul W, Far MS, Cayeux MC, et al. Nutritional status and food intake in nine patients with chronic low-limb ulcers and pressure ulcers: importance of oral supplements. Nutrition 22, 82-88 (2006).
- Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 36(12), 2756-2763 (2005).
- Foley NC, Martin RE, Salter KL, et al. A review of the relationship between dysphagia and malnutrition following stroke. J. Rehabil. Med. 41(9), 707-713 (2009).
- Martins C. Avaliaçãodo Estado Nutricional e Diagnóstico. Nutroclínica (2008).
- Rabito EI, Mialich MS, Martínez EZ, et al. Validation of predictive equations for weight and height using a metric tape. Nutr. Hosp. 26, 614-618 (2008).
- Chumlea WC, Guo S, Roche AI, et al. Prediction of body weight for non-ambulatory elderly from anthropometry. J. Am. Diet Assoc. 88, 564-568 (1988).
- Gray DS, Crider JB, Kelley C, et al. Accuracy of recumbent height measurement. J. Parenter. Enteral. Nutr. 9, 712-715(1985).
- Guigoz Y, Vellas B, Garry PJ, et al. The mini nutritional assessment; a practical assessment tool for graing the nutritional status of elderly patients. In: Guigoz, SC, et al. The Mini Nutritional Assessment: MNA, Facts and Research in Gerontology. New York: Serdi 2, p 15-59 (1999).
- World Health Organization. Physical status the use and interpretation of anthropometrics. Report of a World Health Organization. Expert Committee. WHO. Technical Report Series 854,1-452 (1995).
- Lipschitz DA. Screening for nutritional status in the elderly. Prim. Care21(1), 55-67 (1994).
- World Health Organization. Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva, World Health Organization, (2011). Available in: http://www.who.int/vmnis/indicators/haemoglobin. Accessed: July, 2017.
- Lópes, Herrera RMT, Cruz AJP, et al. Prevalencia de desnutriciónempacientesingresadosemun hospital de rehabilitación y traumatologia. Nutr. Hosp. 20, 121-135 (2005).
- Cerasuolo JO, Cipriano LE, Sposato LA, et al. Population-based stroke and dementia incidence trends: Age and sexvariations. Elsevier Inc. on behalf of the Alzheimer’s Association. 1-8 (2017).
- Chen Y, Li S, Sun FH, et al. Monitoring of Medical Complications after Acute Ischemic Stroke in a Neurological Intensive Care Unit.Eur. Neurol. 66, 204-209 (2011).
- Nii M, Maeda k, Wakabayashi H, et al. Nutritional Improvement and Energy Intake Are Associated with Functional Recovery in Patients after Cerebrovascular Disorders. J. Stroke Cerebral Dis. 25(1), 57-62 (2016).
- Smith EE, Shobha N, Dai D, et al. A Risk Score for In-Hospital Death in Patients Admitted With Ischemicor Hemorrhagic Stroke. J. Am. Heart Assoc. 2(1), e005207 (2013).
- Menegon DB, Berciniet RR, Santos CT, et al. Análise das subescalas de Braden comoindicativos de riscoparaÚlceraporpressão. Texto.Contexto.Enferm. 21(4), 854-861(2012).
- Duarte A, Marques AR, Sallet LHB, et al. Risconutricionalempacienteshospitalizadosdurante o período de internação. Nutr. Clin. Diet Hosp. 36(3), 146-152 (2016).
- Breslow RA, Hallfrisch J, Guy DG, et al. The importance of dietary protein in healing pressure ulcers. J. Am.Geriatr. Soc. 41, 357-362 (1993).
- Kim BJ, Lee SH, Ryu WS, et al. Paradoxical longevity in obese patients with intracerebral hemorrhage. Neurology 76, 567-573 (2011).
- Andersen KK, Olsen TS. The obesity paradox in stroke: lower mortality and lower risk of readmission for recurrent stroke in obese stroke patients. Int. J. Stroke 10, 99-104 (2013).
- Kubo S, Hosomi N, Hara N, et al. Ischemic Stroke Mortality Is More Strongly Associated with Anemia on Admission Than with Underweight Status. J. Stroke Cerebral Dis. (2017).