Review Article - Interventional Cardiology (2011) Volume 3, Issue 6
Role of the functional SYNTAX score in evaluating multivessel coronary artery disease
- Corresponding Author:
- William F Fearon
Division of Cardiovascular Medicine, Stanford University Medical Center
300 Pasteur Drive, H2103, Stanford, CA, 94305, USA
Tel: +1 650 725 2621
Fax: +1 650 725 6766
E-mail: wfearon@stanford.edu
Abstract
Keywords
coronary angiography, coronary artery bypass, coronary artery disease, fractional flow reserve, prognosis, stent
Multivessel coronary artery disease (MVD) is one of the unresolved complex lesion subsets in the current era of interventional cardiology. Historically, coronary artery bypass grafting (CABG) has been the preferred method of revascularization in patients with MVD. However, as a result of the recent drug-eluting stent (DES) revolution, a large and growing number of patients with MVD are undergoing percutaneous coronary intervention (PCI) [1–4].
The SYNergy between percutaneous intervention with TAXus DES and cardiac surgery (SYNTAX) Score (SS) is a comprehensive angiographic scoring system for risk stratification of patients with MVD undergoing contemporary revascularization [5,6]. It has been shown to stratify risk for both early and late outcomes in patients with MVD [2,3,7,8]. However, the SS is inherently limited because it is angiography-based [9]. Recent studies have shown that many angiographically significant lesions are not hemodynamically significant and stenting these stenoses results in worse outcomes. The SS weighs equally all epicardial lesions of greater than 50% stenosis, despite the fact that some may not be physiologically significant (i.e., not responsible for myocardial ischemia). The FAME study demonstrated that fractional flow reserve (FFR) measurement can be used as guidance to decrease rates of major adverse cardiac events (MACE) in patients with MVD compared with angiography-guided PCI [10–12], presumably by focusing intervention on ischemia-producing lesions only. A recent substudy from the FAME trial demonstrated that an FFR-guided functional SS (FSS) can better discriminate risk for adverse events in patients with MVD undergoing PCI than the classic SS [13]. In this article, we will review revascularization methods for patients with MVD and the role of the SS and FSS in evaluating patients with MVD.
How to treat MVD: prior to the SY NTAX trial
Although there has been a dramatic improvement in devices and percutaneous techniques for the treatment of complex stenoses, CABG remains the reference standard approach for revascularizing patients with MVD [14,15].
Historical data from trials comparing PCI with stent implantation and surgical revascularization revealed no differences in terms of mortality and myocardial infarction (MI), but a more favorable outcome has been observed in the CABG arm regarding repeat revascularization [2,3,16]. However, in these initial randomized PCI versus CABG studies, fewer than 10% of patients screened were actually enrolled.
The ERACI II compared bare-metal stent (BMS) implantation with CABG in symptomatic patients with MVD [16]. At the 5-year follow-up, patients initially treated with PCI had similar survival and freedom from non-fatal MI compared with CABG (92.8 vs 88.4% and 97.3 vs 94%, respectively; p = 0.16). Freedom from repeat revascularization procedures was significantly lower with PCI compared with CABG (71.5 vs 92.4%; p = 0.0002). Freedom from MACE was also significantly lower with PCI compared with CABG (65.3 vs 76.4%; p = 0.013).
The ARTS II study compared the efficacy of sirolimus-eluting stent implantation with the two historical arms of ARTS [3]. The 5-year major adverse cardiac and cerebrovascular event (MACCE) rate in ARTS II (27.5%) was significantly higher than ARTS I CABG (21.1%; p = 0.02), and lower than in ARTS I BMS (41.5%; p < 0.001). Although the re-intervention rates in the PCI group were still higher than those of the CABG group, this was counterbalanced by a higher incidence of death/stroke and MI in the CABG group.
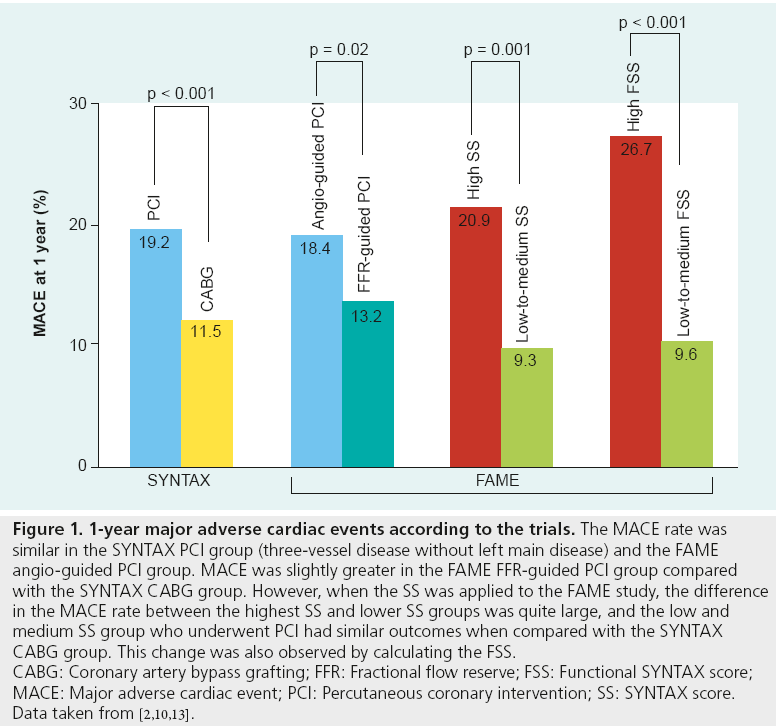
Fueled by these promising results, the SYNTAX trial was performed. It was a multicenter, randomized study designed to evaluate the optimal revascularization treatment for allcomer patients with de novo three-vessel disease and/or left main disease by randomizing patients to either PCI with paclitaxel-eluting stents or surgery [2]. The 1-year rate of MACCE among patients with three-vessel disease in the absence of left main coronary artery disease (CAD) was significantly increased in the PCI group as compared with the CABG group (19.2 vs 11.5%; p < 0.001) (Figure 1), as was the rate of repeat revascularization (14.6 vs 5.5%; p < 0.001). The rate of death from any cause, stroke, or MI in this subgroup was similar with PCI and CABG (8.0 and 6.6%, respectively; p = 0.39). However, at 3 years in the same group, not only MACCE (CABG 18.8% vs PCI 28.8%; p < 0.001), but also the rates of the composite safety end point (death/stroke/MI 10.6 vs 14.8%; p = 0.04) was higher in the PCI arm. These results are consistent with previous registries reporting a survival advantage and a marked reduction in the need for repeat revascularization with CABG in comparison with PCI in patients with more severe CAD [17]. In general, CABG has the advantages of longer durability and more complete revascularization, regardless of the morphology of the obstructing atherosclerotic lesions [18]. However, we also have to remember that the very longterm durability of CABG has not been compared with DES as the data are currently unavailable.
Figure 1: 1-year major adverse cardiac events according to the trials. The MACE rate was
similar in the SYNTAX PCI group (three-vessel disease without left main disease) and the FAME
angio-guided PCI group. MACE was slightly greater in the FAME FFR-guided PCI group compared
with the SYNTAX CABG group. However, when the SS was applied to the FAME study, the difference
in the MACE rate between the highest SS and lower SS groups was quite large, and the low and
medium SS group who underwent PCI had similar outcomes when compared with the SYNTAX
CABG group. This change was also observed by calculating the FSS.
CABG: Coronary artery bypass grafting; FFR: Fractional flow reserve; FSS: Functional SYNTAX score;
MACE: Major adverse cardiac event; PCI: Percutaneous coronary intervention; SS: SYNTAX score.
Data taken from [2,10,13].
Although DES significantly decrease the rate of restenosis compared with BMS and have demonstrated promising results regarding high risk populations with complex lesions [19–21], new concerns including the long-term safety and efficacy of DES have been raised, as a consequence of increased risk of late thrombosis and a late catch-up phenomenon [22,23]. Furthermore, the cost–effectiveness of DES in MVD has been raised [24,25]. All of the studies comparing PCI with DES to CABG performed PCI based on angiographic guidance. The FAME trial demonstrated that PCI guided by angiography alone results in a greater number of stents placed in functionally nonsignificant stenoses. In these cases, the patient suffers the early and late risks of PCI without accruing any benefit from relief of ischemia [10,12,26]. More judicious selection of target lesions and/or patients may make possible similar outcomes after PCI as compared with CABG in patients with MVD.
The role of the SS
In the SYNTAX study, a new scoring system called the SS was introduced in an attempt to better risk stratify patients and inform decision regarding PCI versus CABG for achieving optimal revascularization [5]. The SS is an angiographic scoring system based on coronary anatomy and lesion characteristics, such as presence of total occlusion, bifurcation or trifurcation, angle and involvement of branch vessels, calcification, lesion length, ostial location, tortuosity and presence of thrombus. The SS not only quantifies lesion complexity, but also predicts early and late outcomes after PCI in patients with three-vessel disease and/or left main disease [2,6,8,27]. From the diagnostic angiogram, each coronary lesion producing ≥50% diameter stenosis in vessels ≥1.5 mm is scored separately and added together to provide the overall SS. From the SYNTAX study, three tertiles of SS were established: a low score defined as ≤22, an intermediate score as 23–32 and a high score as ≥33 [5].
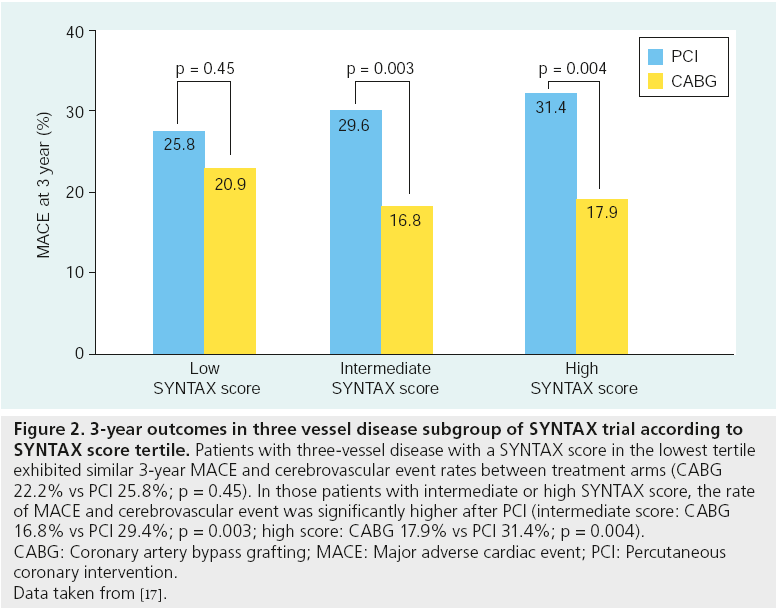
The 1-year rate of MACCE in the PCI group in the SYNTAX study was significantly higher among patients with high SS (23.4%) as compared with those with low scores (13.6%) or intermediate scores (16.7%; p = 0.002 for high vs low scores; p = 0.04 for high vs intermediate scores) [2]. In contrast, in the CABG group, the rate of MACCE was similar among patients with low, intermediate and high scores (14.7, 12.0 and 10.9%, respectively; p > 0.05). There was a significant interaction between SS and treatment group (p = 0.01); patients with low or intermediate scores in the CABG group and in the PCI group had similar rates of MACCE, whereas among patients with high scores, the event rate was significantly increased in the PCI group. A similar result was observed at 3-year follow-up [17]. Patients with 3-vessel disease with a SS in the lowest tertile exhibited similar 3-year MACCE rates between treatment arms (CABG 22.2% vs PCI 25.8%; p = 0.45). In those patients with intermediate or high SS, the rate of MACCE was significantly higher after PCI (intermediate score: CABG 16.8% vs PCI 29.4%; p = 0.003; high score: CABG 17.9% vs PCI 31.4%; p = 0.004) (Figure 2). This finding suggests that a percutaneous approach should be avoided in patients with high or intermediate SS.
Figure 2: 3-year outcomes in three vessel disease subgroup of SY NTAX trial according to
SY NTAX score tertile. Patients with three-vessel disease with a SYNTAX score in the lowest tertile
exhibited similar 3-year MACE and cerebrovascular event rates between treatment arms (CABG
22.2% vs PCI 25.8%; p = 0.45). In those patients with intermediate or high SYNTAX score, the rate
of MACE and cerebrovascular event was significantly higher after PCI (intermediate score: CABG
16.8% vs PCI 29.4%; p = 0.003; high score: CABG 17.9% vs PCI 31.4%; p = 0.004).
CABG: Coronary artery bypass grafting; MACE: Major adverse cardiac event; PCI: Percutaneous
coronary intervention.
Data taken from [17].
The value of the SS was validated by several subsequent studies. The SS was applied to 1292 lesions in 306 patients who underwent PCI for three-vessel disease in the ARTS II trial. When compared with the lowest tertile group (SS < 16; 5-year MACE-free rate: 80.1%), both the intermediate (SS: 16–24) and high (SS > 24) tertile groups demonstrated a lower MACE-free survival rate (intermediate: 70.1%, log-rank p = 0.02; high: 67.1%; p = 0.001) [3]. The SS also had a role in the risk stratification of 1707 all-comer patients undergoing PCI in the LEADERS trial [27]. There was a lower 1-year MACE-free survival in the highest tertile of the SS; 92.2% in low SS (≤8), 91.1% in mid SS (>8 and ≤16) and 84.6% in high SS (>16), respectively (p < 0.001). Similar results were observed in the RESOLUTE all-comers study as the rate of MACE at 1-year was significantly higher in patients in the highest SS tertile [28]. Recently, the largest assessment of the SS in 6508 patients treated with PCI from seven contemporary coronary stent trials was performed by an independent academic research organization and confirmed the ability of the SS to identify patients who are at highest risk of adverse events, irrespective of clinical presentation [29]. Because of these findings, the SS can have a role in patients with any degree of CAD. Recent guidelines have recommended using the SS to decide whether a patient with MVD is appropriate for PCI or CABG [14].
An important limitation of using the SS is that anatomy-based scoring systems have been shown to have a lower ability to predict mortality, when compared with scoring systems using clinical characteristics [30]. The ability to predict outcomes can be improved by adding clinical variables, as is the case in the euroSCORE, the ACEF score, the Mayo Clinic Risk Score or the clinical SS [31–34]. However, despite a continuous effort to detect new and progressively more sophisticated markers of prognosis in patients with CAD, implementation of complicated risk stratification algorithms in the clinical setting remains problematic [35], and the use of too many individual variables may reduce the overall accuracy of data [36].
FFR-guided PCI for MVD
FFR, measured with a coronary pressure wire, is an accurate and lesion-specific index for determining the functional significance of a particular stenosis. FFR takes into account the myocardial distribution of a vessel and the presence of collaterals [37–39]. Assessing the functional significance of nonculprit coronary lesions after culprit lesion intervention in patients with acute coronary syndrome is critical, as increasing stent length or number is associated with worse outcomes [40,41]. Determining the physiological significance of each lesion is challenging with noninvasive or invasive imaging techniques [42–46]. Although nuclear perfusion imaging and other noninvasive stress imaging modalities are generally accurate in patients with single-vessel disease, they are significantly less accurate in patients with MVD [42]. Coronary angiography is not reliable for assessing the functional significance of moderate (50–80% narrowed) single stenoses, let alone multiple or complex abnormalities [45,46]. Intravascular ultrasound (IVUS) in MVD patients generally shows diffuse disease of varying degrees of severity along the coronary artery and is unable to provide functional information of distinct lesions [44,47]. These findings were supported by our previous study, which included 167 consecutive patients with intermediate coronary lesions evaluated by FFR or IVUS (FFR-guided, 83 lesions vs IVUS-guided, 94 lesions) [44]. Although baseline percent diameter stenosis and lesion length were similar in both groups, the IVUS-guided group underwent revascularization therapy significantly more often (91.5 vs 33.7%; p < 0.001). No significant difference was found in MACE between the two groups (3.6% in FFR-guided PCI vs 3.2% in IVUS-guided PCI). However, FFR assessment for multiple lesions is invasive, can be time consuming in some cases and demands systemic injection of vasodilator pharmacotherapy. The technical aspect of FFR measurement and interpretation is also important, especially in multiple lesions in the same vessel and in bifurcation lesions. For example, in the setting of tandem lesions, it is important to measure FFR with the sensor beyond both lesions. If the FFR is not ischemic, then no further intervention is necessary. If it is ischemic then a slow pullback should be performed to identify which lesion is responsible for most of the pressure gradient. The more significant lesion should be stented and then FFR should be measured again. If the FFR remains ischemic, the second lesion should be stented.
Recent studies have shown that stenting functionally nonsignificant coronary stenoses does not improve outcome [10,26,44,48], and optimal medical treatment results in similar outcomes [49]. In the DEFER study [26], eventfree survival at 5 years was not different between the DEFER and perform groups who had FFR ≥ 0.75 (80 and 73%, respectively; p = 0.52), but was significantly worse in the Reference group with FFR < 0.75 (63%; p = 0.03). The composite rate of cardiac death and acute MI in the Defer, Perform and Reference groups was 3.3, 7.9 and 15.7%, respectively (p = 0.21 for Defer vs Perform group; p = 0.003 for the Reference vs both other groups).
The FAME study was a multicenter trial designed to compare two strategies for performing PCI in 1005 patients with MVD [10]. All patients were randomly assigned to angiographyguided PCI (497 patients) or FFR-guided PCI (509 patients). Patients assigned to angiographic guidance underwent stenting of all indicated lesions with DES. In patients assigned to FFR guidance, FFR was measured in each vessel with at least one stenosis and stents were placed only if the FFR was ≤0.80. MACE occurred in 91 patients (18.3%) in the angiography group and in 67 (13.2%) in the FFR group (p = 0.02) at 1 year (Figure 1) [10]. At 2-year follow-up, death or MI occurred in 12.9% of the angiographyguided patients and in 8.4% of the FFR-guided patients (p = 0.02) [12]. These results support the evolving strategy of revascularization of ischemic lesions and medical treatment of nonischemic lesions in patients with MVD.
FSS
Although the SS quantifies lesion complexity and predicts early and late clinical outcomes after PCI in patients with MVD, it can also under- or over-estimate the severity of a significant number of lesions because it is based on angiographic information.
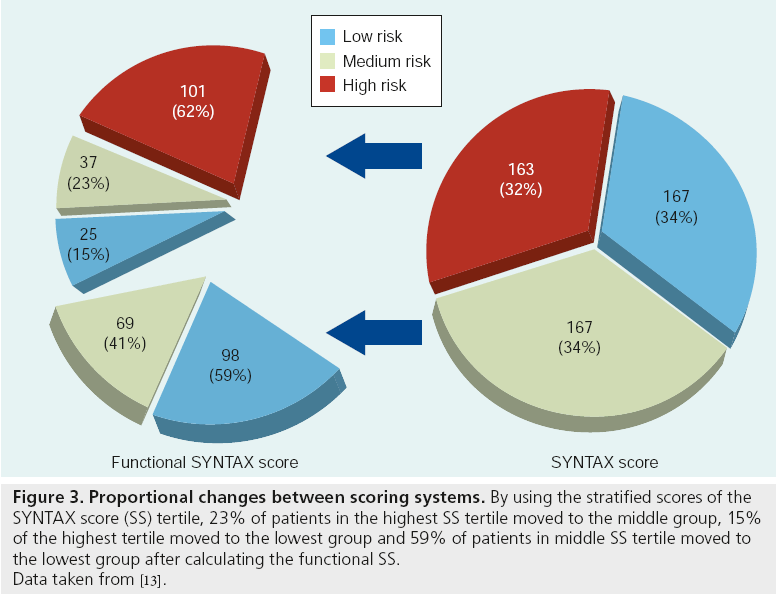
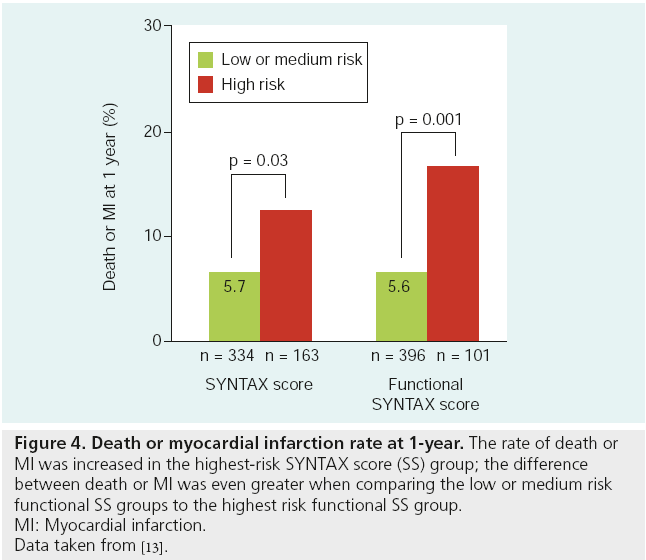
In a recent study, we introduced the FSS, which is determined by recalculating the SS after counting only ischemia-producing lesions with FFR ≤ 0.80. We found that the FSS shifted many apparently high-risk patients into a lower risk group. In addition. it was more reproducible than the SS and a better predictor of outcomes in patients with MVD undergoing PCI [13]. The SS and FSS were prospectively collected in 497 patients enrolled in the FFR-guided arm of the FAME trial. Approximately 23% of patients in the highest SS tertile moved to the middle group, 15% of the highest tertile moved to the lowest group and 59% of patients in middle SS tertile moved to the lowest group. 32% of all patients moved from a higher risk SS group to lower risk groups by calculation of the FSS (Figure 3). Death or MI occurred 15.8% in the highest FSS group and 5.6% in lower FSS groups (p = 0.001) (Figure 4). The rate of MACE was 26.7% in the highest FSS group and 9.6% in lower FSS groups (p < 0.001) (Figure 1). The area under the ROC curve for 1-year MACE was greater with the FSS than with the SS (Harrell’s C of FSS, 0.677 vs SS, 0.630; p = 0.02). FSS demonstrated a better predictive accuracy for MACE compared with SS (integrated discrimination improvement of 1.94%; p < 0.001). Finally, the inter- and intraobserver variability of the FSS was better than that for the SS.
Figure 3: Proportional changes between scoring systems. By using the stratified scores of the
SYNTAX score (SS) tertile, 23% of patients in the highest SS tertile moved to the middle group, 15%
of the highest tertile moved to the lowest group and 59% of patients in middle SS tertile moved to
the lowest group after calculating the functional SS.
Data taken from [13].
Figure 4: Death or myocardial infarction rate at 1-year. The rate of death or
MI was increased in the highest-risk SYNTAX score (SS) group; the difference
between death or MI was even greater when comparing the low or medium risk
functional SS groups to the highest risk functional SS group.
MI: Myocardial infarction.
Data taken from [13].
Clinical application of FSS
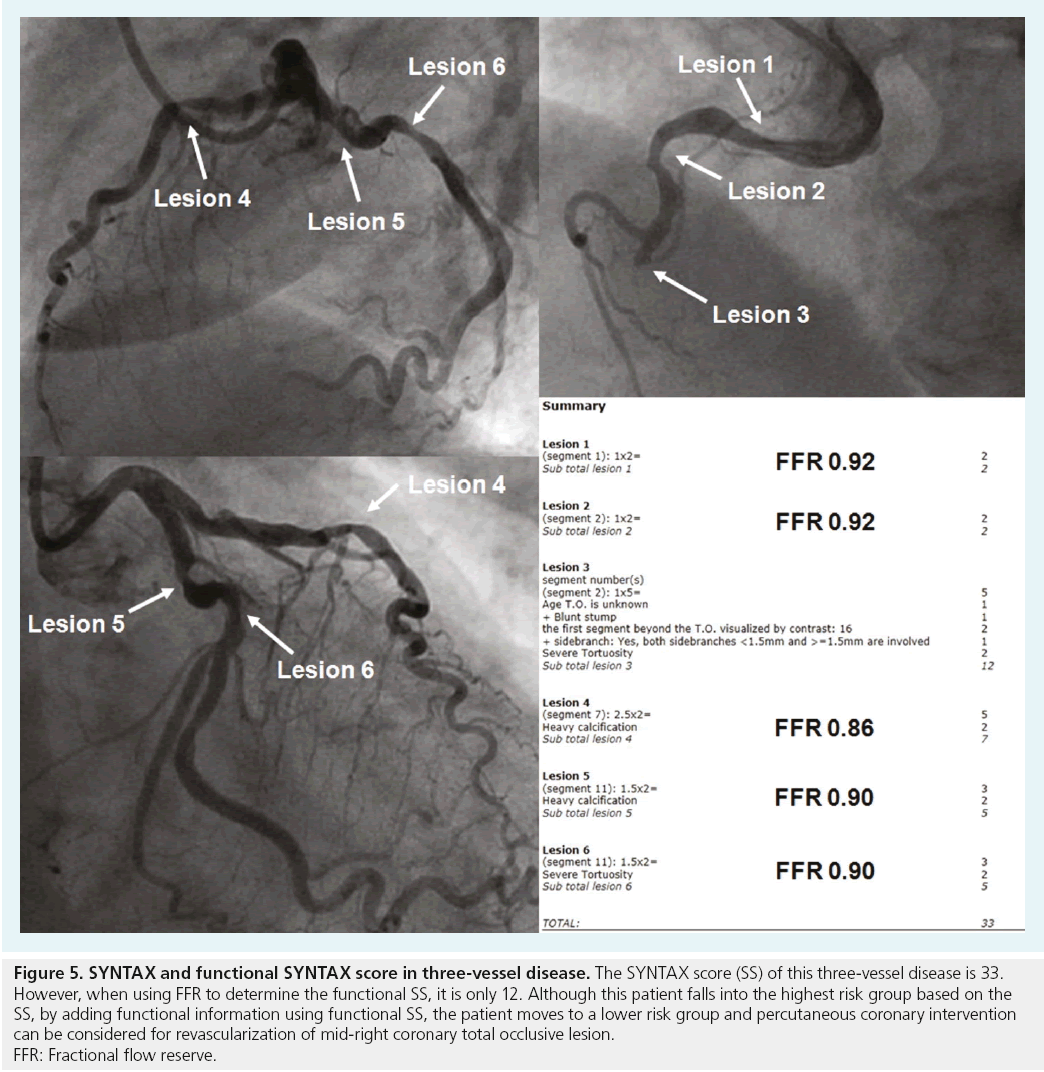
To optimize outcomes in patients undergoing PCI for MVD, the ability to identify those patients and lesions at highest risk of undesired events is very important. With this in mind, the FSS may be an important tool for risk stratification. The FSS can help to more accurately stratify the risk in each patient with multivessel CAD. The MACE rate of the patients who moved from the highest SS tertile to a low or medium risk group based on the FSS, was significantly lower when compared with those patients who remained in the highest risk group (11.3 vs 26.7%; p = 0.028). It means that the patients who moved to a lower risk group are located in a high-risk group angiographically, but in a lower risk group functionally. Their prognosis is similar to patients who started in the lower risk group based on the angiogram alone. This change was driven, in large part, by the conversion of angiographic three-vessel CAD to functional one- or two-vessel CAD. In a FAME subanalysis [11], of all stenoses with an angiographic severity of 50 to 70%, only 35% were functionally significant by FFR. Even in more severe stenoses between 71 and 90% angiographic stenosis severity, a full 20% did not induce reversible MI as established by an FFR value above the ischemic threshold. By first measuring FFR, patients with apparent three-vessel disease can be converted to one- or two-vessel disease. In this manner, the number of low and medium risk patients with MVD in whom percutaneous revascularization can be recommended is increased. A representative case is shown in Figure 5. Although the SS of this case is 33, the FSS is only 12. This patient with angiographic three-vessel disease falls in the highest risk SS group, and CABG is the recommended method for revascularization. However, by adding functional information using the FSS, the patient is only actually in the medium-risk group, and therefore PCI can be considered for revascularization.
Figure 5: SY NTAX and functional SY NTAX score in three-vessel disease. The SYNTAX score (SS) of this three-vessel disease is 33.
However, when using FFR to determine the functional SS, it is only 12. Although this patient falls into the highest risk group based on the
SS, by adding functional information using functional SS, the patient moves to a lower risk group and percutaneous coronary intervention
can be considered for revascularization of mid-right coronary total occlusive lesion.
FFR: Fractional flow reserve.
In Figure 1, outcomes between SYNTAX and FAME trials, which included patients with MVD and analyzed into tertile risk groups, are described. Although direct comparison of these two trials is impossible due to the different degree of coronary disease [2,13], the MACE rate looks similar in the SYNTAX PCI group and the FAME angio-guided PCI group. MACE was slightly greater in the FAME FFR-guided PCI group compared with the SYNTAX CABG group. However, when the SS was applied to the FAME study, the difference in the MACE rate between the highest SS and lower SS groups was quite large and the low and medium SS group who underwent PCI had similar outcomes when compared with the SYNTAX CABG group. This change was also observed by calculating the FSS. Because the patients with the highest FSS had the worst outcome after PCI, surgical revascularization should be considered in this group to hopefully improve outcomes.
A major limitation of the work performed to date on the FSS is that it is retrospective. It remains unclear whether and to what extent our findings can be reproduced in a different group of patients with extensive CAD. Similarly, more data are required to clarify whether the slightly better performance of the FSS observed in this study justifies its use in clinical practice compared with the classic SS or conventional ACC/AHA classification system.
Future perspective
A new paradigm for performing PCI only on physiologically significant lesions based on FFR assessment and medically treating functionally insignificant lesions, even if angiographically significant, has been introduced. The FSS is a new mechanism for further defining which MVD patients will benefit most from PCI as compared with CABG. The next step in establishing this new paradigm is to perform a prospective trial comparing an FSS-guided approach to PCI in patients with MVD with traditional CABG surgery. It may be that with this approach PCI performs as well as CABG in this challenging patient population.
Financial and competing interests disclosure
W Fearon has an institutional research grant from St Jude Medical. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilized in the production of this manuscript.
Executive summary
How to treat multivessel coronary artery disease
▪ Coronary artery bypass graft is a reference standard approach for multivessel coronary artery disease (MVD).
▪ Coronary artery bypass graft has a lower rate of repeat revascularization, and a similar rate of death or myocardial infarction. Selection of target lesions or patients is important for percutaneous coronary intervention (PCI) in MVD.
The role of the SYNTAX score
▪ SYNTAX score (SS) is a new anatomical scoring system for MVD.
▪ SS quantifies lesion complexity and predicts early or late outcomes after PCI in MVD.
Fractional flow reserve-guided PCI for MVD
▪ Stenting in coronary stenoses, without demonstrating their physiologic significance, does not improve outcome.
▪ Treatment based on fractional flow reserve in addition to angiography can decrease adverse cardiac events in MVD.
New anatomical & functional scoring system: functional SS
▪ Functional SS (FSS) is determined by recalculating the SS after counting only ischemia-producing lesions with fractional flow reserve ≤0.80.
▪ FSS has better reproducibility and prognostic value in patients with MVD undergoing PCI.
Clinical application of FSS
▪ Increase the number of lower risk patients with MVD in whom PCI can be recommended.
▪ Significant implications on decision making regarding the choice of revascularization strategy in MVD.
References
Papers of special note have been highlighted as:
▪ of interest
- Kukreja N, Onuma Y, Garcia-Garcia HM, Daemen J, Van Domburg R, Serruys PW. Three-year survival following multivessel percutaneous coronary intervention with bare-metal or drug-eluting stents in unselected patients. Am. J. Cardiol. 103(2), 203–211 (2009).
- Serruys PW, Morice MC, Kappetein AP et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360(10), 961–972 (2009).
- Serruys PW, Onuma Y, Garg S et al. 5-year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J. Am. Coll. Cardiol. 55(11), 1093–1101 (2010).
- Kappetein AP, Dawkins KD, Mohr FW et al. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease. Insights from the SYNTAX run-in phase. Eur. J. Cardiothorac. Surg. 29(4), 486–491 (2006).
- Sianos G, Morel MA, Kappetein AP et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1(2), 219–227 (2005).
- Serruys PW, Onuma Y, Garg S et al. Assessment of the SYNTAX score in the SYNTAX study. EuroIntervention 5(1), 50–56 (2009).
- Capodanno D, Di Salvo ME, Cincotta G, Miano M, Tamburino C. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ. Cardiovasc. Interv. 2(4), 302–308 (2009).
- Van Gaal WJ, Ponnuthurai FA, Selvanayagam J et al. The SYNTAX score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int. J. Cardiol. 135(1), 60–65 (2009).
- Marcus ML, Skorton DJ, Johnson MR, Collins SM, Harrison DG, Kerber RE. Visual estimates of percent diameter coronary stenosis: ‘a battered gold standard’. J. Am. Coll. Cardiol. 11(4), 882–885 (1988).
- Tonino PA, De Bruyne B, Pijls NH et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360(3), 213–224 (2009).
- Tonino PA, Fearon WF, De Bruyne B et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J. Am. Coll. Cardiol. 55(25), 2816–2821 (2010).
- Pijls NH, Fearon WF, Tonino PA et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2 year follow-up of the FAME study. J. Am. Coll. Cardiol. 56(3), 177–184 (2010).
- Nam CW, Mangiacapra F, Entjes R et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J. Am. Coll. Cardiol. 58(12), 1211–1218 (2011).
- Wijns W, Kolh P, Danchin N et al. Guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery. Eur. Heart J. 31(20), 2501–2555 (2010).
- Smith SC Jr, Feldman TE, Hirshfeld JW Jr et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (ACC/AHA/ SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J. Am. Coll. Cardiol. 47(1), e1–e121 (2006).
- Rodriguez AE, Baldi J, Fernandez Pereira C et al. Five-year follow-up of the Argentine randomized trial of coronary angioplasty with stenting versus coronary bypass surgery in patients with multiple vessel disease (ERACI II). J. Am. Coll. Cardiol. 46(4), 582–588 (2005).
- Kappetein AP, Feldman TE, Mack MJ et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur. Heart J. 32(17), 2125–2134 (2011).
- Loop FD, Lytle BW, Cosgrove DM et al. Influence of the internal-mammaryartery graft on 10 year survival and other cardiac events. N. Engl. J. Med. 314(1), 1–6 (1986).
- Chieffo A, Stankovic G, Bonizzoni E et al. Early and mid-term results of drug-eluting stent implantation in unprotected left main. Circulation 111(6), 791–795 (2005).
- Ong AT, Serruys PW, Aoki J et al. The unrestricted use of paclitaxel- versus sirolimus-eluting stents for coronary artery disease in an unselected population: one-year results of the Taxus-Stent Evaluated at Rotterdam Cardiology Hospital (T-SEARCH) registry. J. Am. Coll. Cardiol. 45(7), 1135–1141 (2005).
- Daemen J, Ong AT, Stefanini GG et al. Three-year clinical follow-up of the unrestricted use of sirolimus-eluting stents as part of the Rapamycin-Eluting Stent Evaluated at Rotterdam Cardiology Hospital (RESEARCH) registry. Am. J. Cardiol. 98(7), 895–901 (2006).
- Pfisterer M, Brunner-La Rocca HP, Rickenbacher P et al. Long-term benefit-risk balance of drug-eluting versus bare-metal stents in daily practice: does stent diameter matter? Three-year follow-up of BASKET. Eur. Heart J. 30(1), 16–24 (2009).
- Park DW, Hong MK, Mintz GS et al. Two-year follow-up of the quantitative angiographic and volumetric intravascular ultrasound analysis after nonpolymeric paclitaxel-eluting stent implantation: late ‘catch-up’ phenomenon from ASPECT Study. J. Am. Coll. Cardiol. 48(12), 2432–2439 (2006).
- Poulin F, Rinfret S, Gobeil F. Potential shift from coronary bypass surgery to percutaneous coronary intervention for multivessel disease and its economic impact in the drug-eluting stent era. Can. J. Cardiol. 23(14), 1139–1145 (2007).
- Brunner-La Rocca HP, Kaiser C, Bernheim A et al. Cost-effectiveness of drug-eluting stents in patients at high or low risk of major cardiac events in the Basel Stent KostenEffektivitats Trial (BASKET): an 18-month analysis. Lancet 370(9598), 1552–1559 (2007).
- Pijls NH, Van Schaardenburgh P, Manoharan G et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5 year follow-up of the DEFER study. J. Am. Coll. Cardiol. 49(21), 2105–2111 (2007).
- Wykrzykowska JJ, Garg S, Girasis C et al. Value of the SYNTAX score for risk assessment in the all-comers population of the randomized multicenter LEADERS trial. J. Am. Coll. Cardiol. 56(4), 272–277 (2010).
- Garg S, Serruys PW, Silber S et al. The prognostic utility of the SYNTAX score on 1-year outcomes after revascularization with zotarolimus- and everolimus-eluting stents: a substudy of the RESOLUTE All Comers Trial. JACC. Cardiovasc. Interv. 4(4), 432–441 (2011).
- Garg S, Sarno G, Girasis C et al. A patientlevel pooled analysis assessing the impact of the SYNTAX score on 1 year clinical outcomes in 6508 patients enrolled in contemporary coronary stent trials. JACC Cardiovasc. Interv. 4(6), 645–653 (2011).
- Singh M, Rihal CS, Lennon RJ, Garratt KN, Holmes DR Jr. Comparison of Mayo Clinic risk score and American College of Cardiology/American Heart Association lesion classification in the prediction of adverse cardiovascular outcome following percutaneous coronary interventions. J. Am. Coll. Cardiol. 44(2), 357–361 (2004).
- Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur. J. Cardiothorac. Surg. 16(1), 9–13 (1999).
- Ranucci M, Castelvecchio S, Menicanti L, Frigiola A, Pelissero G. Risk of assessing mortality risk in elective cardiac operations: age, creatinine, ejection fraction and the law of parsimony. Circulation 119(24), 3053–3061 (2009).
- Singh M, Rihal CS, Lennon RJ, Spertus J, Rumsfeld JS, Holmes DR Jr. Bedside estimation of risk from percutaneous coronary intervention: the new Mayo Clinic risk scores. Mayo Clin. Proc. 82(6), 701–708 (2007).
- Garg S, Sarno G, Garcia-Garcia HM et al. A new tool for the risk stratification of patients with complex coronary artery disease: the clinical SYNTAX score. Circ. Cardiovasc. Interv. 3(4), 317–326 (2010).
- Valgimigli M, Serruys PW, Tsuchida K et al. Cyphering the complexity of coronary artery disease using the SYNTAX score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am. J. Cardiol. 99(8), 1072–1081 (2007).
- Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann. Intern. Med. 118(3), 201–210 (1993).
- Pijls NH, De Bruyne B, Peels K et al. Measurement of fractional flow reserve to assess the functional severity of coronaryartery stenoses. N. Engl. J. Med. 334(26), 1703–1708 (1996).
- De Bruyne B, Pijls NH, Bartunek J et al. Fractional flow reserve in patients with prior myocardial infarction. Circulation 104(2), 157–162 (2001).
- Nam CW, Rha SW, Koo BK et al. Usefulness of coronary pressure measurement for functional evaluation of drug-eluting stent restenosis. Am. J. Cardiol. 107(12), 1783–1786 (2011).
- Orlic D, Bonizzoni E, Stankovic G et al. Treatment of multivessel coronary artery disease with sirolimus-eluting stent implantation: immediate and mid-term results. J. Am. Coll. Cardiol. 43(7), 1154–1160 (2004).
- Gerber RT, Ielasi A, Al-Lamee R et al. Long-term follow-up of multivessel percutaneous coronary intervention with drug-eluting stents for de novo lesions with correlation to the SYNTAX score. Cardiovasc. Revasc. Med. 12(4), 220–227 (2011).
- Lima RS, Watson DD, Goode AR et al. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J. Am. Coll. Cardiol. 42(1), 64–70 (2003).
- Pijls NH. Optimum guidance of complex PCI by coronary pressure measurement. Heart 90(9), 1085–1093 (2004).
- Nam CW, Yoon HJ, Cho YK et al. Outcomes of percutaneous coronary intervention in intermediate coronary artery disease: fractional flow reserve-guided versus intravascular ultrasound-guided. JACC Cardiovasc. Interv. 3(8), 812–817 (2010).
- Bartunek J, Sys SU, Heyndrickx GR, Pijls NH, De Bruyne B. Quantitative coronary angio- graphy in predicting functional significance of stenoses in an unselected patient cohort. J. Am. Coll. Cardiol. 26(2), 328–334 (1995).
- Nissen SE, Gurley JC. Assessment of the functional significance of coronary stenoses. Is digital angiography the answer? Circulation 81(4), 1431–1435 (1990).
- Kern MJ. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation 101(11), 1344–1351 (2000).
- Nam CW, Hur SH, Koo BK et al. Fractional flow reserve versus angiography in left circumflex ostial intervention after left main crossover stenting. Korean Circ. J. 41(6), 304–307 (2011).
- Boden WE, O’Rourke RA, Teo KK et al. Optimal medical therapy with or without PCI for stable coronary disease. N. Engl. J. Med. 356(15), 1503–1516 (2007).
▪ Landmark trial comparing coronary artery bypass graft and percutaneous coronary intervention (PCI) with drug-eluting stents for treating patients with three-vessel disease and/or left main disease.
▪ First study showing how to calculate SYNTAX score (SS).
▪ Landmark trial comparing angiographyguided PCI and fractional flow reserve (FFR)-guided PCI for treating patients with multivessel disease.
▪ First study introducing functional SS.
▪ Study demonstrating the long-term safety of deferring functionally nonsignificant stenosis.
▪ The largest analysis showing the efficacy of SS score in PCI.
▪ Landmark study demonstrating the role of FFR in PCI.
▪ First report comparing FFR and intravascular ultrasound for the decision of PCI in intermediate coronary disease.