Short Article - Interventional Cardiology (2013) Volume 5, Issue 4
Rotational angiography and 3D overlay in transcatheter congenital interventions
- Corresponding Author:
- Jamil Aboulhosn
Ahmanson/UCLA Adult Congenital Heart Disease Center, Division of Cardiology
David Geffen School of Medicine at UCLA, CA, USA
E-mail: jaboulhosn@mednet.ucla.edu
Abstract
The incidence of moderate and severe forms of congenital heart disease (CHD) is 6/1000 live births. Without early medical or surgical treatment, the majority of patients with complex CHD would not survive into adulthood. Over the past 60 years, surgical and medical advances have dramatically altered the once bleak prognosis of patients with CHD. In the current era, over 85% of patients with CHD survive to reach adulthood and most live productive and functional lives. Cardiac catheterization with angiocardiography has long been the gold standard for making and confirming hemodynamic and anatomical findings in patients with CHD.
Keywords
congenital heart disease, CTA, MRI, overlay, rotational angiography
The incidence of moderate and severe forms of congenital heart disease (CHD) is 6/1000 live births. Without early medical or surgical treatment, the majority of patients with complex CHD would not survive into adulthood. Over the past 60 years, surgical and medical advances have dramatically altered the once bleak prognosis of patients with CHD. In the current era, over 85% of patients with CHD survive to reach adulthood and most live productive and functional lives [1,2]. Cardiac catheterization with angiocardiography has long been the gold standard for making and confirming hemodynamic and anatomical findings in patients with CHD. This position of pre-eminence is being challenged in the current era by an array of noninvasive imaging techniques, each with certain strengths and weaknesses, which together are capable of almost complete noninvasive anatomical and functional cardiovascular assessment; such techniques include Doppler echocardiography, computed tomographic angiography (CTA) and MRI [3]. In parallel with the decreasing need for diagnostic catheterization, there has been a dramatic increase in the number of transcatheter cardiac interventions in patients with CHD [4]. The success of percutaneous transcatheter interventions is contingent upon proper patient selection [5]. MRI is an attractive potential alternative to fluoroscopy for guiding transcatheter procedures owing to the avoidance of radiation and development of near real-time dynamic imaging sequences; however, it has not yet come into routine clinical use. Fluoroscopic angiography has remained the dominant modality for vascular navigation and intervention owing to the high spatial and temporal resolution, widespread commercial availability and ease of use.
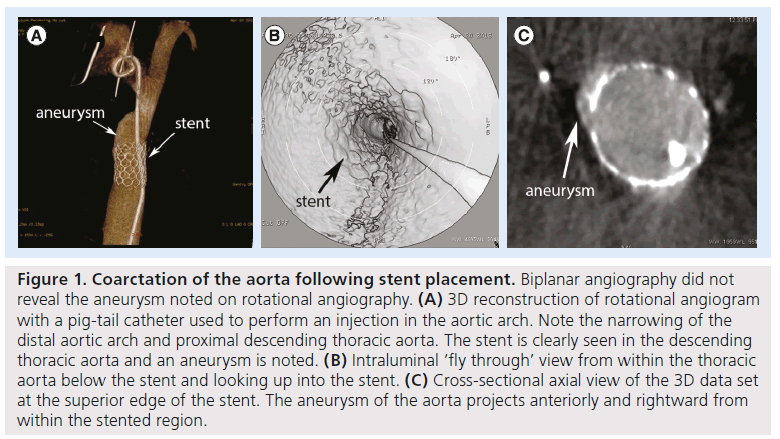
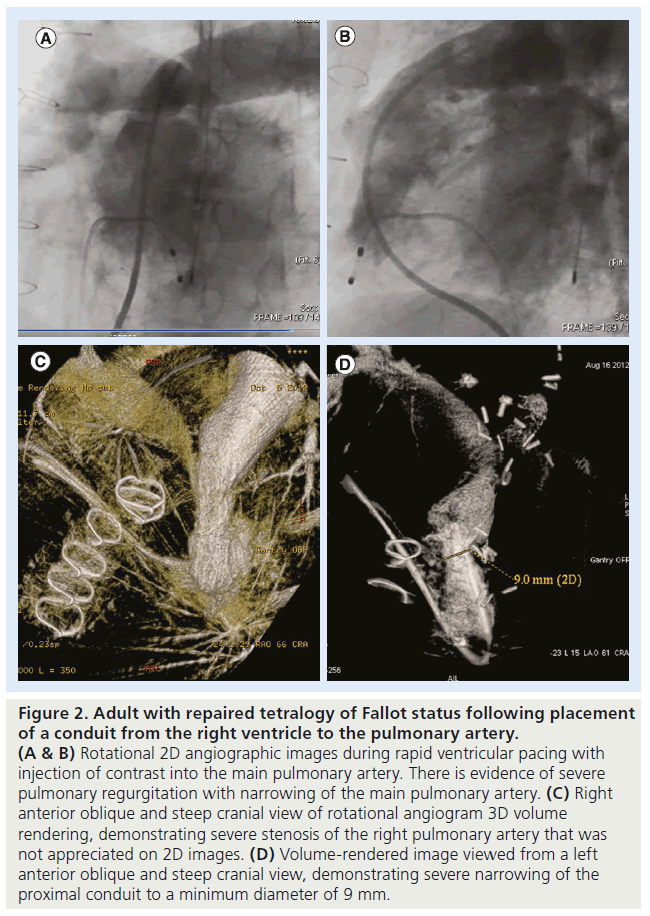
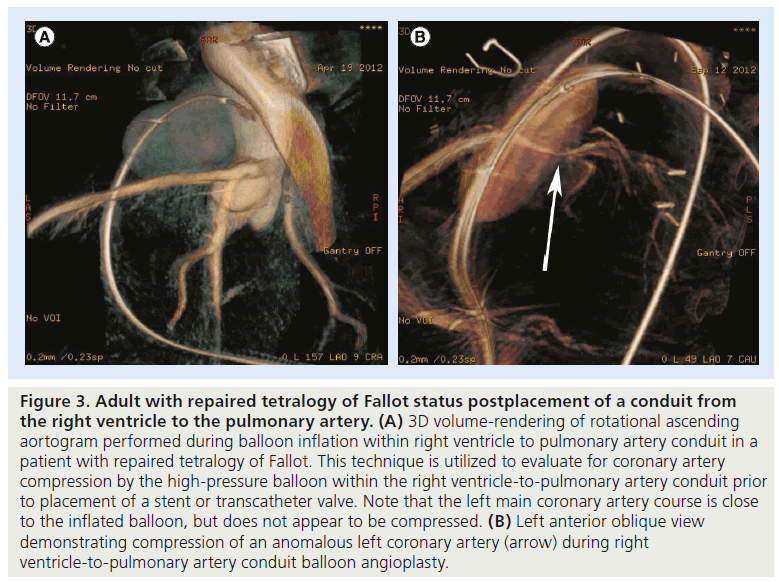
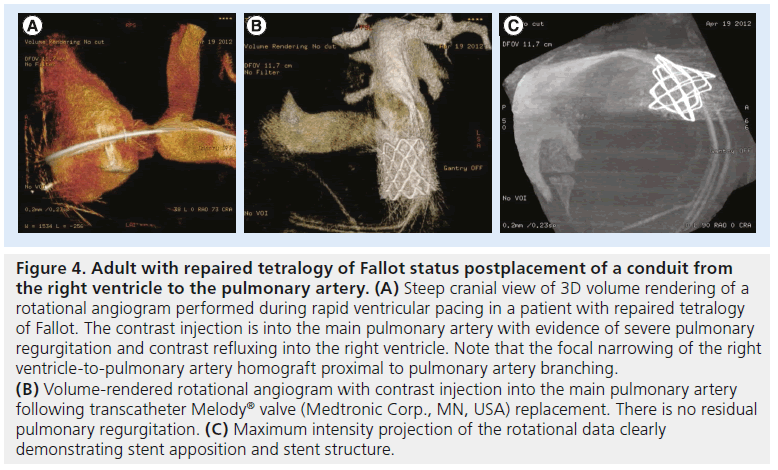
The use of rotational fluoroscopy to generate true 3D computed rotational angiograms has gone from a research tool to the clinical arena in the past two decades (Figures 1–4) [6]. Endovascular treatment planning and execution can be greatly aided by computed rotational angiography, which also yields quantitative information by reconstruction of the raw projection data into a volume database (Figures 1–5) [7,8]. These techniques are increasingly used in the planning and execution of vascular interventional procedures; the hardware and software necessary to perform rotational angiography with 3D reconstruction is commercially available from all major vendors. Rotational angiography to guide coronary arterial imaging and interventions has been reported, but is not yet widely utilized in the clinical setting (Figure 3) [9–11].
Figure 1: Coarctation of the aorta following stent placement. Biplanar angiography did not reveal the aneurysm noted on rotational angiography. (A) 3D reconstruction of rotational angiogram with a pig-tail catheter used to perform an injection in the aortic arch. Note the narrowing of the distal aortic arch and proximal descending thoracic aorta. The stent is clearly seen in the descending thoracic aorta and an aneurysm is noted. (B) Intraluminal ‘fly through’ view from within the thoracic aorta below the stent and looking up into the stent. (C) Cross-sectional axial view of the 3D data set at the superior edge of the stent. The aneurysm of the aorta projects anteriorly and rightward from within the stented region.
Figure 2: Adult with repaired tetralogy of Fallot status following placement of a conduit from the right ventricle to the pulmonary artery. (A & B) Rotational 2D angiographic images during rapid ventricular pacing with injection of contrast into the main pulmonary artery. There is evidence of severe pulmonary regurgitation with narrowing of the main pulmonary artery. (C) Right anterior oblique and steep cranial view of rotational angiogram 3D volume rendering, demonstrating severe stenosis of the right pulmonary artery that was not appreciated on 2D images. (D) Volume-rendered image viewed from a left anterior oblique and steep cranial view, demonstrating severe narrowing of the proximal conduit to a minimum diameter of 9 mm.
Figure 3: Adult with repaired tetralogy of Fallot status postplacement of a conduit from the right ventricle to the pulmonary artery. (A) 3D volume-rendering of rotational ascending aortogram performed during balloon inflation within right ventricle to pulmonary artery conduit in a patient with repaired tetralogy of Fallot. This technique is utilized to evaluate for coronary artery compression by the high-pressure balloon within the right ventricle-to-pulmonary artery conduit prior to placement of a stent or transcatheter valve. Note that the left main coronary artery course is close to the inflated balloon, but does not appear to be compressed. (B) Left anterior oblique view demonstrating compression of an anomalous left coronary artery (arrow) during right ventricle-to-pulmonary artery conduit balloon angioplasty.
Figure 4: Adult with repaired tetralogy of Fallot status postplacement of a conduit from the right ventricle to the pulmonary artery. (A) Steep cranial view of 3D volume rendering of a rotational angiogram performed during rapid ventricular pacing in a patient with repaired tetralogy of Fallot. The contrast injection is into the main pulmonary artery with evidence of severe pulmonary regurgitation and contrast refluxing into the right ventricle. Note that the focal narrowing of the right ventricle-to-pulmonary artery homograft proximal to pulmonary artery branching. (B) Volume-rendered rotational angiogram with contrast injection into the main pulmonary artery following transcatheter Melody® valve (Medtronic Corp., MN, USA) replacement. There is no residual pulmonary regurgitation. (C) Maximum intensity projection of the rotational data clearly demonstrating stent apposition and stent structure.
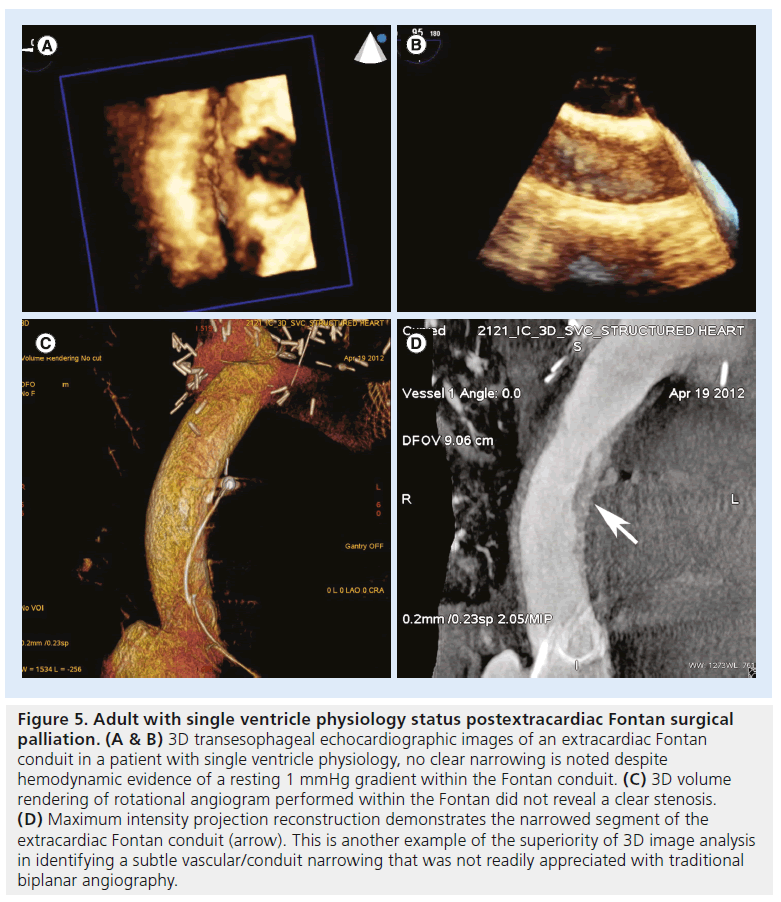
Figure 5: Adult with single ventricle physiology status postextracardiac Fontan surgical palliation. (A & B) 3D transesophageal echocardiographic images of an extracardiac Fontan conduit in a patient with single ventricle physiology, no clear narrowing is noted despite hemodynamic evidence of a resting 1 mmHg gradient within the Fontan conduit. (C) 3D volume rendering of rotational angiogram performed within the Fontan did not reveal a clear stenosis. (D) Maximum intensity projection reconstruction demonstrates the narrowed segment of the extracardiac Fontan conduit (arrow). This is another example of the superiority of 3D image analysis in identifying a subtle vascular/conduit narrowing that was not readily appreciated with traditional biplanar angiography.
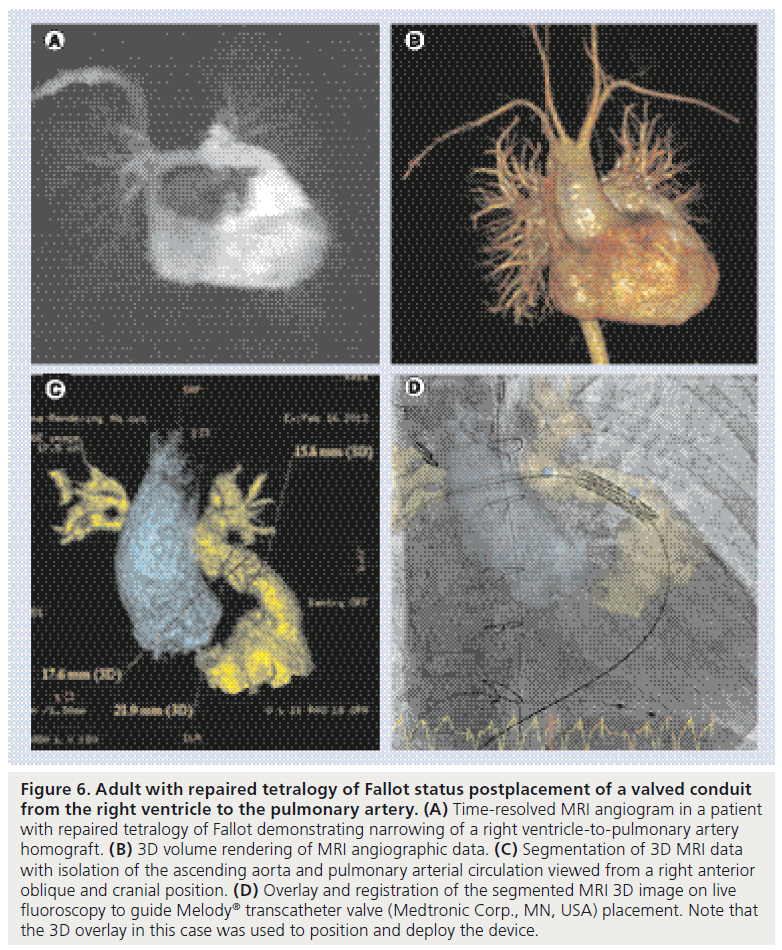
Advanced image registration software has been developed and allows 3D acquisitions from either CTA or MRI to be used intraprocedurally by overlaying the image on the x-ray fluoroscopy screen (Figure 6) [12,13]. The overlaid segmentations are registered with x-ray views in various image planes. A variety of registration modalities are currently in use, including registration to fiducial markers [14], automatic 2D/3D registration, automatic 3D/3D registration and manual 3D to 2D visual matching. These techniques have been effectively used to guide electrophysiologic interventions, such as placement on coronary sinus pacing leads by overlay of 3D CTA data [15].The use of 3D rotational angiography and CTA overlay may improve image quality and registration to guide complex structural interventions, such as transcatheter aortic valve implantation, trans-septal puncture and pulmonary vein stent placement [16]. Rotational angiography and MRI/CTA overlay are not widely utilized in the congenital catheterization arena, but they have been successfully used to guide interventions and may potentially reduce radiation exposure by decreasing the number of cineangiograms that need to be performed during interventional or diagnostic procedures, potentially reducing the radiation dose by 30% [11,17–23].
Figure 6: Adult with repaired tetralogy of Fallot status postplacement of a valved conduit from the right ventricle to the pulmonary artery. (A) Time-resolved MRI angiogram in a patient with repaired tetralogy of Fallot demonstrating narrowing of a right ventricle-to-pulmonary artery homograft. (B) 3D volume rendering of MRI angiographic data. (C) Segmentation of 3D MRI data with isolation of the ascending aorta and pulmonary arterial circulation viewed from a right anterior oblique and cranial position. (D) Overlay and registration of the segmented MRI 3D image on live fluoroscopy to guide Melody® transcatheter valve (Medtronic Corp., MN, USA) placement. Note that the 3D overlay in this case was used to position and deploy the device.
There are a number of important limitations or the clinical utility of these technologies that must be addressed. Rotational angiography is dependent on suspension of respiration and rapid pacing or adenosine injections to minimize cardiac output. This is difficult to perform in patients who are not under general anesthesia. The 3D overlay techniques can be gated to the respiratory cycle, but there is typically some temporal delay resulting in image motion that is not perfectly synchronized to the respiratory cycle. The currently available systems do not allow for dynamic cardiac motion and only allow for static image overlay, which makes the definition of intracardiac anatomy less reliable than the overlay of pulmonary or systemic vasculature. The overlayed CTA or MRI may not represent the immediate anatomy during a procedure owing to the distortion that can be introduced by catheters and stiff wires. Moreover, patient motion and positioning on the catheterization table may alter the orientation and position of the anatomy and may result in further inaccuracy. It should also be noted that MRI of metallic objects results in artifacts that can obscure anatomy. All of these limitations should be factored into a procedure where these techniques will be utilized. The next generation of systems may address many of these limitations.
Figures 1–6 are examples of 3D rotational angiographic reconstructions or 3D overlay in patients with various types of CHD. These cases illustrate the potential advantages of 3D imaging techniques in patients with CHD, including:
▪ Improved visualization of complex structures not well seen using 2D imaging alone;
▪ Selection of the best working view from the 3D data set;
▪ Appreciation of subtle abnormalities not seen well by traditional imaging modalities;
▪ 3D image overlay on live f luoroscopy for intraprocedural image guidance;
▪ Assessment of coronary arterial circulation for compression during pulmonary angioplasty and stenting procedures.
Conclusion
Rotational angiography with 3D reconstruction and MRI/CTA overlay on traditional fluoroscopic images is revolutionizing transcatheter procedures in patients with CHD. The advantages of these techniques include: improved visualization of complex structures, selection of the best working view and appreciation of subtle abnormalities not seen well by traditional imaging modalities. With further advances in the ease of use and wider availability, the use of these 3D imaging techniques will become routine in the performance of congenital transcatheter interventional procedures.
Future perspective
The following are the envisioned next steps for this technology in the congenital catheterization laboratory:
▪ The ‘triple-overlay’ technique with coregistration of preprocedural MRI/CTA, intraprocedural 3D rotational angiography, 3D echocardiography and live fluoroscopy with 3D manipulation;
▪ Overlay and live registration of dynamic 3D echocardiographic and Doppler data;
▪ Dynamic cardiac overlay to facilitate interventions on a 3D beating heart overlay;
▪ Live MRI- and CTA-guided interventions.
Financial & competing interests disclosure
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ Fluoroscopy and cineangiography continue to be essential and are the backbone of imaging in the catheterization laboratory.
▪ Advances in 2D and 3D echocardiography have resulted in the widespread use of transesophageal and intracardiac imaging to guide interventions, so much so that these techniques are considered essential for the safe performance of certain procedures (e.g., atrial septal defect/patent foramen ovale closure and ventricular septal defect closure).
▪ Computed tomographic angiography/MRI overlay and rotational angiography with 3D reconstruction are likely to play an increasing role in interventional congenital catheterization.
▪ Commercially available systems allow for the efficient and relatively simple utilization of these techniques in the catheterization laboratory.
▪ Although there is a paucity of literature on the topic to support this assertion, the potential benefits of these 3D techniques in the catheterization laboratory are immense and include improved image quality, improved interventional guidance, the potential for lower radiation and improved patient safety.
References
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- Moller JH, Taubert KA, Allen HD, Clark EB, Lauer RM. Cardiovascular health and disease in children: current status. A Special Writing Group from the Task Force on Children and Youth, American Heart Association. Circulation 89(2), 923–930 (1994).
- Warnes CA, Liberthson R, Danielson GK et al. Task force 1: the changing profile ofcongenital heart disease in adult life. Care of the adult with congenital heart disease. J. Am. Coll. Cardiol. 37(5), 1170–1175 (2001).
- Brancaccio G, Miraldi F, Ventriglia F, Michielon G, Di Donato RM, De Santis M. Multidetector-row helical computed tomography imaging of unroofed coronary sinus. Int. J. Cardiol. 91(2–3), 251–253 (2003).
- Schneider DJ, Levi DS, Serwacki MJ, Moore SD, Moore JW. Overview of interventional pediatric cardiology in 2004. Minerva Pediatr. 56(1), 1–28 (2004).
- Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K; Amplatzer Investigators. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J. Am. Coll. Cardiol. 39(11), 1836–1844 (2002).
- Himbert D, Pontnau F, Messika-Zeitoun D et al. Feasibility and outcomes of transcatheteraortic valve implantation in high-risk patients with stenotic bicuspid aortic valves. Am. J. Cardiol. 110(6), 877–883 (2012).
- Zegdi R, Ciobotaru V, Noghin M et al. Is it reasonable to treat all calcified stenotic aortic valves with a valved stent? Results from a human anatomic study in adults. J. Am. Coll. Cardiol. 51(5), 579–584 (2008).
- Therrien M, Morrison DK, Wong AM, Rubin GM. A genetic screen for modifiers of a kinase suppressor of Ras-dependent rough eye phenotype in Drosophila. Genetics 156(3), 1231–1242 (2000).
- Tani LY, Minich LL, Pagotto LT, Shaddy RE. Usefulness of Doppler echocardiography to determine the timing of surgery for supravalvar aortic stenosis. Am. J. Cardiol. 86(1), 114–116 (2000).
- Stamm C, Li J, Ho SY, Redington AN, Anderson RH. The aortic root in supravalvular aortic stenosis: the potential surgical relevance of morphologic findings. J. Thorac. Cardiovasc. Surg. 114(1), 16–24 (1997).
- de Lezo JS, Pan M, Medina A, Segura J, Pavlovic D, Romero M. Acute aortic insufficiency complicating stent treatment of supravalvular aortic stenosis: successful release of trapped leaflets by wiring the stent. Catheter. Cardiovasc. Interv. 61(4), 537–541 (2004).
- Luijendijk P, Stevens AW, de Bruin-Bon RH et al. Rates and determinants of progressiveaortic valve dysfunction in aortic coarctation. Int. J. Cardiol. doi:10.1016/j.ijcard.2012.07.028(2012) (Epub ahead of print).
- Keshavarz-Motamed Z, Garcia J, Maftoon N, Bedard E, Chetaille P, Kadem L. A new approach for the evaluation of the severity of coarctation of the aorta using Doppler velocity index and effective orifice area: in vitro validation and clinical implications. J. Biomech. 45(7), 1239–1245 (2012).
- George AK, Sonmez M, Lederman RJ, Faranesh AZ. Robust automatic rigid registration of MRI and x-ray using external fiducial markers for XFM-guided interventional procedures. Med. Phys. 38(1), 125–141 (2011).
- Holzer R, Qureshi S, Ghasemi A et al. Stenting of aortic coarctation: acute, intermediate, and long-term results of a prospective multi-institutional registry – Congenital Cardiovascular Interventional Study Consortium (CCISC). Catheter. Cardiovasc. Interv. 76(4), 553–563 (2010).
- Bhalgat PS, Pinto R, Dalvi BV. Transcatheter closure of large patent ductus arteriosus with severe pulmonary arterial hypertension: short and intermediate term results. Ann. Pediatr.Cardiol. 5(2), 135–140 (2012).
- Hokanson JS, Gimelli G, Bass JL. Percutaneous closure of a large PDA in a 35-year-old man with elevated pulmonary vascular resistance. Congenit. Heart Dis. 3(2), 149–154 (2008).
- Pac A, Polat TB, Vural K, Pac M. Successful two-stage correction of ventricular septal defect and patent ductus arteriosus in a patient with fixed pulmonary hypertension. Pediatr. Cardiol. 31(1), 111–113 (2010).
- Yoshimura N, Hori Y, Horii Y et al. Comparison of magnetic resonance imaging with transthoracic echocardiography in the diagnosis of ventricular septal defect-associated coronary cusp prolapse. J. Magn. Reson. Imaging 32(5), 1099–1103 (2010).
- Glatz AC, Zhu X, Gillespie MJ, Hanna BD, Rome JJ. Use of angiographic CT imaging in the cardiac catheterization laboratory for congenital heart disease. JACC Cardiovasc. Imaging 3(11), 1149–1157 (2010).
- Dori Y, Sarmiento M, Glatz AC et al. X-ray magnetic resonance fusion to internal markers and utility in congenital heart disease catheterization. Circ. Cardiovasc. Imaging 4(4), 415–424 (2011).
- Ratnayaka K, Saikus CE, Faranesh AZ et al. Closed-chest transthoracic magnetic resonance imaging-guided ventricular septal defect closure in swine. JACC Cardiovasc. Interv. 4(12), 1326–1334 (2011).
- Ratnayaka K, Raman VK, Faranesh AZ et al. Antegrade percutaneous closure of membranous ventricular septal defect using x-ray fused with magnetic resonance imaging. JACC Cardiovasc. Interv. 2(3), 224–230(2009).
▪ While previous use of MRI and x-ray registration has required time-consuming manual intervention to register the two modalities, in this article, the authors present a fully automatic rigid-body registration method.
▪▪ Sought to evaluate the utility of using rotational angiography with 3D reconstruction in a pediatric cardiac catheterization laboratory.
▪▪ Demonstrated that internal marker-based registration can be performed quickly, with minimal radiation, without the need for contrast, and with clinically acceptable accuracy using commercially available software. The authors also demonstrated several potential uses for x-ray magnetic resonance fusion in routine clinical practice.
▪ Demonstration of the utility of real-time MRI to guide transcatheter closure of ventricular septal defect.