Case Report - Interventional Cardiology (2020) Volume 12, Issue 4
Rumpel-Leede phenomenon after brachial artery catheterization
Ali Izzat Toufaily1*, Ali Amine El Sayed21Division of cardiology, Faculty of medical sciences, Lebanese University, Beirut, Lebanon
2Division of cardiology, Al Zahraa Hospital University Medical Center, Beirut, Lebanon
- *Corresponding Author:
- Ali Izzat Toufaily
Division of cardiology
Faculty of medical sciences
Lebanese University, Beirut, Lebanon
E-mail: alitfayli81@gmail.com
Received date: July 08, 2020; Accepted date: July 23, 2020; Published date: July 30, 2020
Abstract
Background: Rumpel-Leede (R-L) phenomenon is a rare event in which the small dermal capillaries of an extremity rupture in response to application of mechanical pressure to that extremity, such as when inflating a cuff during noninvasive blood pressure monitoring , when tying a tourniquet to draw blood or when applying compressive devices to the arm arteries following heart catheterization.
Case presentation: In this report, we present an interesting case of a patient who develops Rumpel-Leede phenomenon, characterized by the appearance of a petechial rash that results from acute dermal capillary rupture that occurred secondary to raised pressure in the dermal vessels caused by the inflation of a compression device at the brachial artery site post coronary angioplasty.
Conclusion: This report highlighted the importance of considering the Rumpel-Leed phenomenon as a benign and self-limited condition in patient who develops a petechial rash following compression of the upper extremity arteries.
Keywords
umpel-leede phenomenon; Petechial rash; Compression device; Brachial artery
Introduction
The Rumpel‐Leede phenomenon (RLP), first described by Theodor Rumple (1909) and Carl Stockbridge Leede (1911) is characterized by an acute dermal capillary rupture caused by tourniquet‐like forces leading to distal petechia and purpura on release of the pressure.
It has been associated with conditions that predispose patients to capillary fragility or bleeding diathesis or both, such as scarlet fever, Epstein ‐ Barr virus infection, diabetic microangiopathy, hypertension, thrombocytopenia, Ehlers- Danlos syndrome etc., [1-3].
The first reported association of Rumpel- Leede sign with coronary intervention via radial artery cannulation was described by Manuel Rattka, and Wolfgang Rottbauer [4], thereafter others have reported the same association (almost four published cases report in the literature) [5,6]. Thus we report the first case of Rumpel-Leede phenomenon following brachial artery access.
Case presentation
We present a case of 65 year old female patient, light smoker, nondrinker, overweight presented for elective angioplasty for known severe stenosis of her right coronary artery (RCA).
Her medical history was significant for coronary artery disease status post double stenting of her left anterior descending artery (LAD) two months ago, hypertension and dyslipidemia. She did not have diabetes mellitus.
Her medications included aspirin, clopidogrel, ACEi and a high-dose statin. Laboratory panel revealed normal GFR and coagulopathy studies.
She underwent successful stenting of her right coronary artery with no adverse reaction. However, both radial vessels were very tortuous and spastic which made navigating the arm extremely difficult. Then due to patient’s refusal to switch to the transfemoral approach, coronary angioplasty was performed via the left brachial artery and initial hemostasis at access site was achieved by placement of a brachial artery compression band.
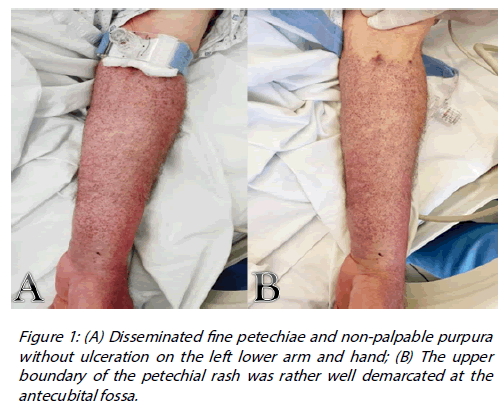
According to the brachial band deflation protocol, the first deflation will take place after 30 minutes. Meanwhile, just a few minutes later, the patient developed a non-blanching non-raised and non-tender rash with a multiple fine petechiae around the left lower arm (Figure 1). There was no evidence of rash on her face, trunk, or lower limbs.
Remarkably, the upper boundary of the petechial rash was well demarcated at the antecubital fossa, extended from just below the elbow from the lower edge of the compression device and involved the dorsal and ventral surface of the left forearm, the dorsal surface of the left hand as well as the palmar surface of the left hand, although to a lesser extent. No other skin lesions were present except for a small hematoma at the brachial puncture site.
Notice that radial and ulnar pulses remained well palpable and all motor and sensory function appeared intact.
The acute development of a petechial rash within a couple of minutes distally from the compression band typically applied to the upper arm (at the brachial artery site), raised the possibility of the Rumpel-Leede phenomenon which is characterized by acute capillaries rupture into the dermis secondary to abrupt raised pressure in the dermal vessels.
Other explanations such as drug related reaction or vasculitis are very unlikely mainly due to the very located and demarcated rash just below the level of compression device and the non-progressive nature of the rash over the following 24 hours despite continuation of dual antiplatelet therapy [7].
Of note, our patient did not have a prior history of this phenomenon. Her petechial hemorrhages regressed within two days without any specific treatment and were no longer visible on further outpatient follow-up.
Conclusion
Physicians should be aware that acute dermal capillary rupture, although rare, can occur post brachial artery compression and prompt diagnosis of Rumpel-Leede phenomenon is crucial to avoid lengthy, costly and unnecessary investigations.
References
- Chester MW, Barwise JA, Holzman MD, et al. Acute dermal capillary rupture associated with noninvasive blood pressure monitoring. J Clin Anesth. 19(6):473-5 (2007).
- Grande AJ, Reid H, Thomas E, et al. Tourniquet test for dengue diagnosis: systematic review and meta-analysis of diagnostic test accuracy. PLoS Negl Trop Dis. 10(8): e0004888 (2016).
- Dubach P, Mantokoudis G, Lämmle B. Rumpel-Leede sign in thrombocytopenia due to Epstein-Barr virus-induced mononucleosis. Br J Haematol. 148(1): 2 (2010).
- Rattka M, Rottbauer W. Rumpel-Leede sign after coronary angiography. Dtsch Arztebl Int. 11(4): 115(6) (2018).
- Khoury Abdulla R, Safian RD. Rumpel-Leede phenomenon after radial artery catheterization. Circ Cardiovasc Interv. 11(4): e006507 (2018).
- Lee S, Jang YB, Kang KP, et al. Rumpel-Leede phenomenon in a hemodialysis patient. Kidney Int. 78(2): 224 (2010).
- Pritchard AE, Lockhart EL. Rumpel-Leede phenomenon in a patient being treated with prasugrel. Transfusion. 57(7): 1642 (2017).