Research Article - Clinical Investigation (2017) Volume 7, Issue 3
Selection of Methods for Percutaneous Endoscopic Gastrostomy (PEG) that is more Safety and Useful Techniques on the Patients
- Corresponding Author:
- Ken Kawaura
Gastroenterological Endoscopy Division
Kanazawa Medical University 1-1 Daigaku
Uchinada- machi, Kahoku-gun, Ishikawa, 920-0293, Japan
E-mail: ura-ken@kanazawa-med.ac.jp
Submitted: 25 August 2017; Accepted: 09 September 2017; Published online: 15 September 2017
Abstract
Objective: Percutaneous endoscopic gastrostomy has been widely adopted, and its use is increasing in Japan due to the rapid aging of society and promotion of medical care at home. Percutaneous endoscopic gastrostomy is performed in patients with a variety of underlying basic diseases. Therefore, a procedure that is safe and less burdensome for the patient is required.
Material and methods: We studied a percutaneous endoscopic gastrostomy procedure that is both safe and less burdensome, in 260 patients undergoing gastrostomy in our department. The items studied were postoperative risk factors for fever, postoperative risk factors for elevated leukocyte count, and risk factors for C-reactive protein (CRP) elevation.
Results: Serious complications were fewer with the three-point fixing method of the abdominal and gastric walls. Multivariate analysis indicated that the conventional Pull method was an independent risk factor for fever (P<0.0001), and the bedridden state of the patient was a risk factor for leukocyte elevation. High Prognostic Nutrition Index (PNI) was an independent risk factor for CRP elevation.
Conclusions: Percutaneous endoscopic gastrostomy performed with the Modified Introducer method by fixing the abdominal and gastric walls showed fewer complications and reduced burden on the patient compared to other methods.
Keywords
Percutaneous endoscopic gastrostomy (PEG), Three-point fixing method of the abdominal and gastric walls, Modified Introducer method
Introduction
Ponsky successfully performed endoscopic gastrostomy for the first time in 1979 [1]. Since then, endoscopic gastrostomy has been widely adopted, and its use is increasing in Japan due to the rapid aging of society and promotion of medical care at home according to policy instruction of Ministry of Health, Labour and Welfare [2-6]. The gastrostomy method has undergone various improvements, and many procedures have been developed. Gastrostomy is relatively easy to perform with intravenous anesthesia if the environment is conducive to endoscopy. On the other hand, patients requiring gastrostomy generally have a variety of underlying diseases [7-9]. Therefore, a safe procedure that can reduce the burden on the patients as much as possible is required [10-13].
At present, the procedures can be broadly classified into two types, i.e., the Pull/Push method and the Modified Introducer method [14]. Percutaneous endoscopic gastrostomy (PEG) has been performed in our department since May 2001. We used the Pull method to create a fistula with a PEG kit from Boston Scientific from May 2001 to June 2007 [15,16]. We have performed PEG with the Modified Introducer method using the product from Olympus Corp. or a Seldinger PEG kit from February 2006 to the present [17,18]. In future, the need for gastrostomy is expected to increase due to further aging of society and the corresponding increase in number of dementia patients. Therefore, we reconsidered the PEG procedure that is safe and less burdensome by comparison based on the complication rate and blood sampling data in patients undergoing PEG in our department. This research received approval from the Kanazawa Medical University Hospital Ethics Committee.
Material and Methods
A total of 260 patients that underwent gastrostomy in our department between May 2001 and December 2014 were included in this study. In the first half of the study period from May 2001 to June 2007, the fistula was created with the Pull method using the PEG kit manufactured by Boston Scientific Corp. In the later years, we performed PEG with the Modified Introducer method using the product from Olympus Corp. or the Seldinger PEG kit from February 2006 to the present. The fistula is created by fixing the gastric and abdominal walls at three points in our department. The procedure is performed under intravenous anesthesia administered by the endoscopic center. We used the small-diameter scopes XP-240 and XP-260 manufactured by Olympus Corp. The scope was inserted orally.
The first-generation antibiotic, cephalosporin, was generally used for only 2 days, i.e., the day of the procedure and the following day.
The body temperature, increase of leukocyte count, increase in the C-reactive protein (CRP) level, and the presence or absence of complications after the procedure were compared as the study items, and the relations with sex, age, Prognostic Nutrition Index (PNI) [4], procedure, and procedure location were studied. Body temperature >37.4°C was treated as “fever,” as cooling is started at this temperature in our department. Cases in which the leukocyte count after gastrostomy was ≥1000/μL were treated as showing “leukocyte elevation.” Cases in which there was an increase in the inflammation response indicator, CRP, compared to before gastrostomy were defined as showing “CRP elevation.” With regard to the procedure location, the lower and middle parts of the body, and the anterior wall and near the greater curvature were studied.
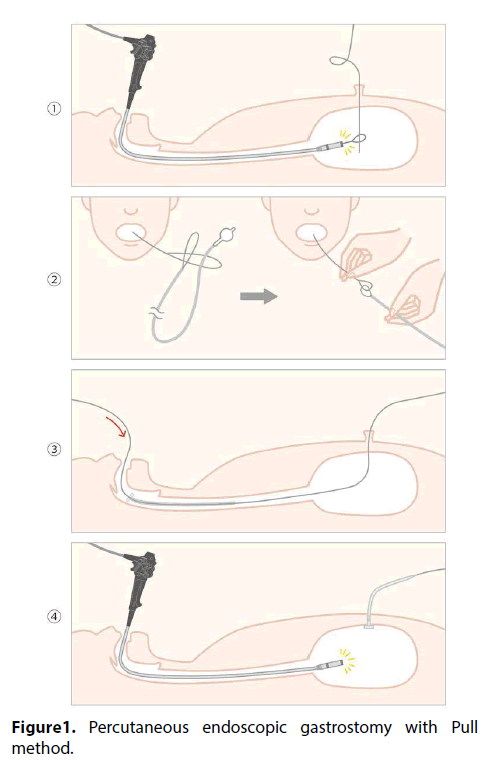
Pull method
The gastric and abdominal walls are fixed at three points with the fixture, and the fistula is created at the center. The guide wire is inserted into the stomach from the abdominal wall and held in place with a snare. It is then drawn from the body along with the endoscope inserted orally, with the catheter and guide wire connected outside the body. In this method, the guide wire coming out of the abdominal wall is pulled, and the fistula catheter is passed from the oral cavity to the stomach (Figure 1) [19-24].
Figure 1: Percutaneous endoscopic gastrostomy with Pull method.
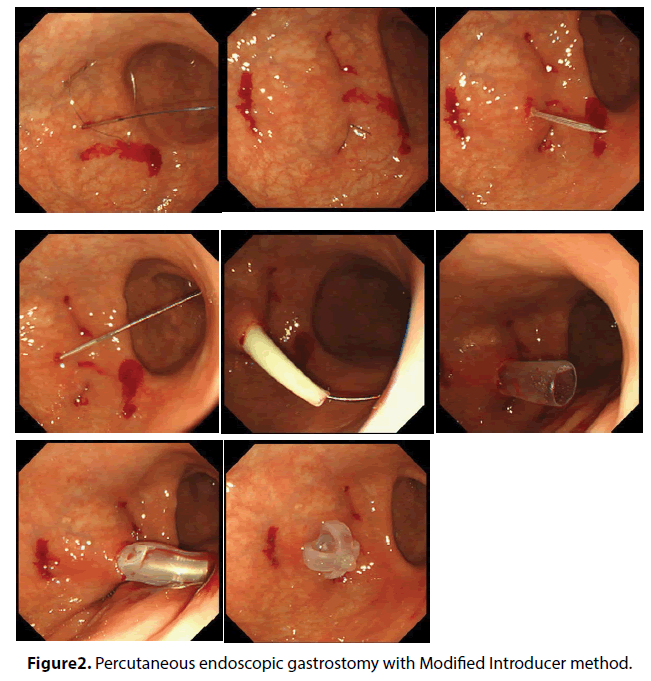
Modified introducer method
In the same way, the gastric wall and abdominal wall are fixed at three points with the fixture and the fistula is created at the center. An incision is made with a scalpel in the central part that is fixed, and the guide wire is inserted into the stomach through the fistula. In this method, the fistula is expanded adequately using a dilator and the fistula catheter is placed directly from the abdominal wall. In recent years, the fistula has been created using the over tube accessory; there are few usage examples for over tube at present and it has not been studied in detail (Figure 2) [20,21,24].
Figure 2: Percutaneous endoscopic gastrostomy with Modified Introducer method.
Prognostic nutrition index (PNI)
Prognostic Nutrition Index (PNI) is an index of nutritional status in humans and is calculated with the following formula determined using two factors, i.e., serum albumin level and peripheral lymphocyte count, as reported by Onodera et al. [4].
PNI=10×Alb(g/dL) + 0.005×Lymph. C. (/mm3 peripheral blood)
We use JMP9 (SAS Institute Japan Ltd.) for statistics. Univariate and multivariate analyses along with logistic analyses are used to study the presence or absence of fever, age, sex, procedure, procedure location, activity factor, PNI, leukocyte elevation, and CRP elevation. In all analyses, P<0.05 was taken to indicate statistical significance.
Results
Patient characteristics are shown in Table 1. The procedures used were the Pull method for 52 cases and Modified Introducer method for 208 cases. The procedure was performed in the lower part of the body in 100 cases and the middle part of the body in 160 cases. The procedure was performed on the anterior wall in 232 cases and on near the greater curvature in 28 cases. With regard to the activity factor, 104 cases were self-reliant and 156 were bedridden patients (Table 1).
| Fever | WBC | CRP | ||||||
|---|---|---|---|---|---|---|---|---|
| Variable | n | No fever 210 (%) | Fever 50 (%) | Leukocyte no change 163 (%) |
Leukocyte elevation 97 (%) |
CRP no change 122 (%) |
CRP elevation 138(%) |
|
| Sex | Male Female |
165 95 |
134 (81.2) 76 (80.0) |
31 (18.8) 19 (20.0) |
109 (66.1) 54 (56.8) |
56 (33.9) 41 (43.2) |
81 (49.1) 41 (43.2) |
84 (50.9) 54 (56.8) |
| Age | ≤74 ≥75 |
118 142 |
102 (86.4) 108 (76.1) |
16 (13.6) 34 (23.9) |
77 (65.3) 86 (60.6) |
41 (34.8) 56 (39.4) |
58 (49.2) 64 (45.1) |
60 (50.8) 78 (54.9) |
| PNIa | ≤34 ≥35 |
96 164 |
79 (82.3) 131 (79.9) |
17 (17.7) 33 (20.1) |
61 (63.5) 102 (62.2) |
35 (36.5) 62 (37.8) |
56 (58.3) 66 (40.2) |
40 (41.7) 98 (59.8) |
| Method | MImb Pullc |
208 52 |
188 (90.4) 22 (42.3) |
20 (9.6) 30 (57.7) |
134 (64.4) 29 (55.8) |
74 (35.6) 23 (44.2) |
95 (45.7) 27 (51.9) |
113 (54.3) 25 (48.1) |
| Location Midd vs. Lowe |
Midd Lowe |
160 100 |
130 (81.3) 80 (80.0) |
30 (18.8) 20 (20.0) |
101 (63.1) 62 (62.0) |
59 (36.9) 38 (38.0) |
81 (50.6) 41 (41.0) |
79 (49.4) 59 (59.0) |
| Location Antf vs. Greg |
Antf Greg |
232 28 |
188 (81.0) 22 (78.6) |
44 (19.0) 6 (21.4) |
143 (61.6) 20 (71.4) |
89 (38.4) 8 (28.6) |
107 (46.1) 15 (53.6) |
125 (53.9) 13 (46.4) |
| Activity | Self Bedridden |
104 156 |
92 (88.5) 118 (75.6) |
12 (11.5) 38 (24.4) |
74 (71.2) 89 (57.1) |
30 (28.9) 67 (42.9) |
51 (49.0) 71 (45.5) |
53 (51.0) 85 (54.5) |
Table 1. Patient characteristics
The status after the procedure is shown in Table 2. There were 50 cases with fever >37.4°C. The Pull method was used in 30 cases and Modified Introducer method was used in 20 cases. The number of patients with leukocyte count ≥1000/μL after the procedure was 97, and 138 patients had elevated CRP after the procedure (Table 2).
| Variable | n |
|---|---|
| Fistula bleeding | 22 (Pullb 2, MImc 20) |
| Gastric internal bleeding | 5 (Pullb 0, MImc 5) |
| Peritonitis | 0 |
| Pneumoperitoneum | 0 |
| Severe pneumonia | 0 |
Table 2. Complications for PEGa
The rate of complications during the procedure was 10% and occurred in 26 cases. The most common complication was fistula bleeding, which occurred in 22 patients. There were two cases in the Pull method and 20 cases in the Modified Introducer method. Although the number of cases of complications was higher for the Modified Introducer method, the difference was not statistically significant. There were no cases of gastric internal bleeding in the Pull method, while there were five cases in the Modified Introducer method. However, there were no cases of serious complications, such as peritonitis, pneumoperitoneum, and severe pneumonia, after the procedure (Table 3) [25].
| N | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| variable | No fever | fever | ORh (95%CIi) | P-value | OR (95%CI) | P-value | |
| Sex | Male Female |
134 76 |
31 19 |
Referent 1.081 (0.564–2.029) |
0.8116 | Referent 0.829 (0.378–1.831) |
0.6385 |
| Age | ≤74 ≥75 |
102 108 |
16 34 |
Referent 1.203 (0.740–1.960) |
0.4567 | Referent 0.706 (0.319–1.531) |
0.3808 |
| PNIa | ≤34 ≥35 |
79 131 |
17 33 |
Referent 0.573 (0.349–0.934) |
0.0253 | Referent 0.970 (0.442–2.156) |
0.9390 |
| Method | MImb Pullc |
188 22 |
20 30 |
Referent 26.941 (14.240–53.550) |
<0.0001 | Referent 12.024 (5.657–26.702) |
< 0.0001 |
| Location1 | Midd Lowe |
130 80 |
30 20 |
Referent 1.860 (1.140–3.053) |
0.0129 | Referent 1.023 (0.475–2.173) |
0.9525 |
| Location2 | Antf Greg |
188 22 |
44 6 |
Referent 8.640 (5.001–15.314) |
<0.0001 | Referent 1.566 (0.474–4.702) |
0.4375 |
| Activity | Self Bedridden |
92 118 |
12 38 |
Referent 1.000 (0.615–1.627) |
1.0000 | Referent 1.260 (0.557–2.922) |
0.5817 |
Table 3. Risk factors for fever
Risk factors for fever
The risk factors for patients with fever >37.4°C after the procedure were studied. As shown in Table 1, 50 of the 260 cases (19.2%) had fever after the procedure; 30/52 cases (57.7%) had fever in the Pull method and 20/208 cases (9.6%) had fever in the Modified Introducer method. As shown in Table 3, univariate analysis indicated that the risk of fever with the Pull method was 26.941 times that of the Modified Introducer method (P<0.0001). In addition, a significant difference was observed even in the high PNI value group (odds ratio: 0.573, P=0.0253). In the study of the procedure location, location 1 (comparison of the middle and lower parts), and location 2 (comparison of the anterior wall and near the greater curvature), the risk of fever was high for the procedure (odds ratio: 1.860, P =0.0129) performed in the middle part of the body and the procedure (odds ratio: 8.640, P<0.0001) performed in near the greater curvature for fistula respectively, and the differences were statistically significant. Further, on multivariate analysis, gastrostomy was an independent factor for fever in the Pull method (P<0.0001) with an odds ratio of 12.024 in comparison with the Modified Introducer method (Table 3).
Risk factors for leukocyte elevation
As shown in Table 4, the results of univariate and multivariate analyses showed significant differences only for activity of the patients as a risk factor for leukocyte elevation. That is, patients that are bedridden are at greater risk of leukocyte elevation than those that live independently (odds ratio: 1.757, P=0.0473). Leukocyte elevation was observed in 30/104 (28.9%) of the patients living independently, and in 67/156 (42.9%) of bedridden patients (Table 4).
| N | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| Variable | no change | elevation | ORh (95%CIi) | P-value | OR (95%CI) | P-value | |
| Sex | Male Female |
109 54 |
56 41 |
Referent 0.677 (0.403 – 1.138) |
0.1397 | Referent 0.720 (0.415–1.250) |
0.2423 |
| Age | ≤74 ≥75 |
77 86 |
41 56 |
Referent 1.222 (0.738 – 2.036) |
0.4567 | Referent 1.050 (0.609–1.812) |
0.8599 |
| PNIa | ≤34 ≥35 |
61 102 |
35 62 |
Referent 0.828 (0.558–1.587) |
0.8284 | Referent 0.941 (0.540–1.645) |
0.8302 |
| Method | MImb Pullc |
134 29 |
74 23 |
Referent 1.436 (0.770–2.657) |
0.2521 | Referent 1.212 (0.626–2.329) |
0.5635 |
| Location1 | Midd Lowe |
101 62 |
59 38 |
Referent 1.049 (0.624–1.755) |
0.8553 | Referent 1.163 (0.672–2.012) |
0.5877 |
| Location2 | Antf Greg |
143 20 |
89 8 |
Referent 0.643 (0.257–1.472) |
0.3033 | Referent 0.618 (0.2373–1.4850) |
0.2986 |
| Activity | Self Bedridden |
74 89 |
30 67 |
Referent 1.857 (1.100 – 3.181) |
0.0203 | Referent 1.757 (1.012 – 3.092) |
0.0473 |
Table 4. Risk factors for leukocyte elevation
Risk factors for CRP elevation
The risk factors impacting CRP elevation after gastrostomy were examined (Table 5). CRP elevation was observed (Table 1) in 98 cases (59.8%), and high PNI was an independent risk factor (odds ratio: 2.101, P =0.0074) in both univariate and multivariate analyses.
| N | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| Variable | No change | elevation | ORh (95%CIi) | P-value | OR (95%CI) | P-value | |
| Sex | Male Female |
81 41 |
84 54 |
Referent 1.270 (0.765–2.117) |
0.3555 | Referent 1.193 (0.692–2.064) |
0.5250 |
| Age | ≤ 74 ≥ 75 |
58 64 |
60 78 |
Referent 1.178 (0.722–1.924) |
0.4567 | Referent 1.373 (0.807–2.352) |
0.2442 |
| PNIa | ≤ 34 ≥ 35 |
56 66 |
40 98 |
Referent 2.079 (1.245–3.485) |
0.0047 | Referent 2.101 (1.225–3.642) |
0.0074 |
| Method | MImb Pullc |
95 27 |
113 25 |
Referent 0.778 (0.422–1.432) |
0.2521 | Referent 0.640 (0.328–1.234) |
0.1846 |
| Location1 | Midd Lowe |
81 41 |
79 59 |
Referent 1.475 (0.893–2.454) |
0.8553 | Referent 1.460 (0.855–2.512) |
0.1679 |
| Location2 | Antf Greg |
107 15 |
125 13 |
Referent 0.742 (0.333–1.631) |
0.4560 | Referent 0.751 (0.320–1.743) |
0.5044 |
| Activity | Self Bedridden |
51 71 |
53 85 |
Referent 1.152 (0.700–1.896) |
0.5769 | Referent 1.131 (0.660–1.938) |
0.6538 |
Table 5. Risk factors for CRP elevation
Discussion
We studied a gastrostomy method that is safe and less burdensome on the patient based on the cases of gastrostomy performed in our department. First, we will discuss the complications. The fistula was created using the Pull method with a small-diameter endoscope and Funada-style device to fix the gastric and abdominal walls at three points from the very beginning of gastrostomy in our department. The small-diameter endoscope is used to reduce the burden in the pharyngeal region and physical stress on the patients, and also to reduce the risk of accidental aspiration. Further, it is possible to prevent the leakage of gastric juice and contents of the stomach into the intraabdominal cavity by fixing the gastric and abdominal walls at three points, and the risk of serious complications, such as peritonitis caused by infection and inflammation, can be significantly reduced. When we adopted the Modified Introducer method, there were many reports indicating pneumoperitoneum as a complication of this method. There were no cases of pneumoperitoneum in our department with the method where the gastric and abdominal walls were securely fixed at three points. While fixing, it is important to bear in mind that a surface has to be created by maintaining a distance of 5 mm between the sutures. The surface area is reduced if the distance between the sutures is less than 5 mm, and the risk of infection increases due to the reduced blood circulation in the surrounding tissues. On the other hand, fixing of the gastric and abdominal walls becomes slack when the surface area increases, and the risks of inflammation, infection, and pneumoperitoneum increase. The frequency of complications is expected to be decreased by fixing the gastric and abdominal walls securely. There was a severe bleeding tendency from the fistula in 20 of 22 cases with the Modified Introducer method. However, there were no statistically significant differences for either. There are no effective measures for preventing fistula bleeding at present, and the risk factors have not been identified. If there is bleeding, the fistula is sutured, hemostatic treatment is provided, and the sutures are removed the next day. Hemostatic treatment was possible for all cases in this method. Based on our experience, if there is excessive bleeding, the incision is large, or compression hemostasis is difficult when an incision is made on the skin during the procedure, bleeding is stopped by suturing the area surrounding the fistula after insertion of the fistula catheter. Although the procedure has been performed in a small number of cases, no cases of fistula bleeding were observed with this method. We believe that this may be an effective method to prevent fistula bleeding.
We examined the rate of increases in fever and leukocyte count, the number of cases with CRP elevation after the procedure, and studied the impact of the PEG procedure on the patients. Fifty of the 260 patients (19.2%) had fever >37.4°C after the procedure. We studied the relationships between each factor with the risk factors. On univariate analysis, the risk factors for fever were low PNI value, Pull method, and procedure locations of the lower body and near the greater curvature. From the results of multivariate analysis, gastrostomy with the Pull method was an independent factor. This was considered to be due to the risk of aspiration or introduction of bacteria from the oral cavity into the wound, because the endoscope is drawn out of the oral, and the fistula catheter is again passed through the oral cavity along with the endoscope in the conventional Pull method. The endoscope is inserted only once with the Modified Introducer method procedure, which is used at present, and the risk of infection is only at the insertion location because the fistula catheter is inserted from the abdominal wall side and the overall risk is considered to be low. In addition, the risk of fever was higher for procedures performed in the lower part of the body than the middle, and for near the greater curvature than the anterior wall. Anatomically, there are fewer blood vessels, and the distance from the abdominal wall is shorter for the middle part of the body and the anterior wall. On the other hand, the greater omentum of the stomach with abundant blood vessels is close to the greater curvature and lower part of the body, and also the distance from the abdominal wall is greater. The increase in risk of bacterial exposure compared to the lower part of the body and the anterior wall is considered to be because of the greater insertion distance for the fistula catheter. The body network in the greater curvature also has abundant blood vessels and is not a suitable location for gastrostomy. Therefore, the anterior wall in the middle part of the body is considered to be the best location for gastrostomy. With regard to PNI, the risk of fever was low in the group with good nutritional status. The results indicated a lower risk of fever when the general health condition was good although the reason remains unclear. The nutritional status of gastrostomy patients is often poor. However, maintaining a good nutritional status during the procedure is considered to be important.
The leukocyte count has increased in 97 (37.3%) of the 260 cases. The activity factor of the patient was a risk factor for leukocyte elevation on both univariate and multivariate analyses. The bedridden state was a risk factor for the condition of the patient. Notably, gastrostomy method and gastrostomy location were not risk factors for leukocyte elevation. Thus, the leukocyte count elevation after gastrostomy is considered to reflect physical stress and not infection symptoms due to gastrostomy. In gastrostomy, it is considered that the physical stress may be greater in patients that are bedridden.
We also took into consideration elevated CRP, but factors directly related to fistula techniques, such as gastrostomy location, and gastrostomy methods, were not risk factors for CRP elevation in contrast to leukocyte count elevation. As a risk factor, the nutritional status of the group with a high PNI value was good. Liver function was inferred to be almost normal in cases with good nutritional status, and the reaction is sensitive and is considered to participate in CRP elevation.
In this study, age, sex, gastrostomy method, and gastrostomy location were not risk factors for leukocyte count elevation or CRP elevation after gastrostomy. These values should be taken as references rather than to trust them completely during follow-up because there were no increases based on the gastrostomy technique used in the present study.
Conclusion
We believe that the use of the small-diameter scope and three-point fixing method for the gastric and abdominal walls at our department was very effective for preventing infection. Further, the gastrostomy procedure performed using the Modified Introducer method at the anterior wall in the middle part of the body was shown to result in lower risk of fever and reduced risk of infection in patients, and this method is considered to reduce the burden on the patient. Gastrostomy itself is a burden on the patient, but safer gastrostomy with less burden is possible if gastrostomy is performed maintaining the health of the patient using a suitable method at the appropriate location.
Acknowledgements
The author wishes to thank R. Nozaki for their secretarial assistance.
Disclosures Statement
Drs. Ken Kawaura, Tohru Itoh, Kazu Hamada, Hidekazu Kitakata, Sadahumi Azukisawa, Hideyuki Okamura, Sachio Urashima, Masaru Sakurai, and Masao Ishizaki have no conflicts of interest or financial ties to disclose.
References
- Gauderer MW, Ponsky JL, Izant RJ Jr. Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg 15: 872-875 (1980).
- Tokunaga T, Kubo T, Ryan S, Tomizawa M, Yoshida S, Takagi K, et al. Long-term outcome after placement of a percutaneous endoscopic gastrostomy tube. Geriatr Gerontol Int 8: 19-23 (2008).
- Suzuki Y, Tamez S, Murakami A, Taira A, Mizuhara A, Horiuchi A, et al. Survival of geriatric patients after percutaneous endoscopic gastrostomy in Japan. World J Gastroenterol 16: 5084-5091 (2010).
- Tominaga N, Shimoda R, Iwakiri R, Tsuruoka N, Sakata Y, Hara H, et al. Low serum albumin level is risk factor for patients with percutaneous endoscopic gastrostomy. Intern Med 49: 2283-2288 (2010)
- Grant JP. Comparison of percutaneous endoscopic gastrostomy with Stamm gastrostomy. Ann Surg 207: 598-603 (1988).
- Rabeneck L, Wray NP, Petersen NJ. Long-term outcomes of patients receiving percutaneous endoscopic gastrostomy tubes. J Gen Intern Med 11: 287-293 (1996).
- Sanders DS, Carter MJ, D'Silva J, James G, Bolton RP, Bardhan KD. Survival analysis in percutaneous endoscopic gastrostomy feeding: a worse outcome in patients with dementia. Am J Gastroenterol 95: 1472-1475 (2000).
- Sanders DS, Carter MJ, D'Silva J, James G, Bolton RP, Willemse PJ, et al. Percutaneous endoscopic gastrostomy: a prospective audit of the impact of guidelines in two district general hospitals in the United Kingdom. Am J Gastroenterol 97: 2239-2245 (2002).
- Hasan M, Meara RJ, Bhowmick BK, Woodhouse K. Percutaneous endoscopic gastrostomy in geriatric patients: attitudes of health care professionals. Gerontology 41: 326-331 (1995).
- Van Rosendaal GM, Verhoef MJ, Kinsella TD. How are decisions made about the use of percutaneous endoscopic gastrostomy for long-term nutritional support? Am J Gastroenterol 94: 3225-3228 (1999).
- Van Rosendaal GM, Verhoef MJ, Mace SR, Kinsella TD. Decision-making and outcomes for percutaneous endoscopic gastrostomy: a pilot study. J Clin Gastroenterol 24: 71-73 (1997)
- Cervo FA, Bryan L, Farber S. To PEG or not to PEG: a review of evidence for placing feedig tubes in advanced dementia and the decision-making process. Geriatrics 61: 30-35 (2006).
- Suzuki Y, Urashima M, Izumi M, Ito Y, Uchida N, Okada S, et al. The Effects of Percutaneous Endoscopic Gastrostomy on Quality of Life in Patients With Dementia. Gastroenterology Res 5: 10-20 (2012).
- Wu TK, Pietrocola D, Welch HF. New method of percutaneous gastrostomy using anchoring devices. Am J Surg 153: 230-232 (1987).
- Horiuchi A, Nakayama Y, Tanaka N, Fujii H, Kajiyama M. Prospective randomized trial comparing the direct method using a 24 Fr bumper-button-type device with the pull method for percutaneous endoscopic gastrostomy. Endoscopy 40: 722-726 (2008).
- Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, Yoshikawa M. PEG with introducer or pull method: a prospective randomized comparison. Gastrointest Endosc 57: 837-841 (2003).
- Dormann AJ, Wejda B, Kahl S, Huchzermeyer H, Ebert MP, Malfertheiner P. Long-term results with a new introducer method with gastropexy for percutaneous endoscopic gastrostomy. Am J Gastroenterol 101: 1229-1234 (2006).
- Dormann AJ, Glosemeyer R, Leistner U, Deppe H, Roggel R, Wigginghaus B, et al. Modified percutaneous endoscopic gastrostomy (PEG) with gastropexy--early experience with a new introducer technique. Z Gastroenterol 38: 933-938 (2000).
- Sartori S, Trevisani L, Nielsen I, Tassinari D, Abbasciano V. Percutaneous endoscopic gastrostomy placement using the pull-through or push-through techniques: is the second pass of the gastroscope necessary? Endoscopy 28: 686-688 (1996).
- Halkier BK, Ho CS, Yee AC. Percutaneous feeding gastrostomy with the Seldinger technique: review of 252 patients. Radiology 171: 359-362 (1989).
- Hogan RB, DeMarco DC, Hamilton JK, Walker CO, Polter DE. Percutaneous endoscopic gastrostomy--to push or pull. A prospective randomized trial. Gastrointest Endosc 32: 253-258. (1986).
- Jonas SK, Neimark S, Panwalker AP. Effect of antibiotic prophylaxis in percutaneous endoscopic gastrostomy. Am J Gastroenterol 80: 438-441 (1985).
- Sturgis TM, Yancy W, Cole JC, Proctor DD, Minhas BS, et al. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy. Am J Gastroenterol 91: 2301-2304 (1996).
- Kozarek RA, Ball TJ, Ryan JA Jr. When push comes to shove: a comparison between two methods of percutaneous endoscopic gastrostomy. Am J Gastroenterol 81: 642-646 (1986).
- Chaudhary KA, Smith OJ, Cuddy PG, Clarkston WK. PEG site infections: the emergence of methicillin resistant Staphylococcus aureus as a major pathogen. Am J Gastroenterol 97: 1713-1716 (2002).