Case Report - Interventional Cardiology (2022) Volume 14, Issue 3
Stent failure: OCT identification of false lumen wiring of distal stent edge dissection
- Corresponding Author:
- Ali Hillani
Department of Cardiology, McMaster University, 1280 Main St West, Hamilton, L8L2X2, Canada,
E-mail: dr.alihillani@gmail.com
Received date: 22-Apr-2022, Manuscript No. FMIC-22-61498; Editor assigned: 25-Apr -2022, PreQC No. FMIC-22-61498 (PQ); Reviewed date: 12-May-2022, QC No. FMIC-22-61498; Revised date: 19-May-2022, Manuscript No. FMIC-22-61498 (R); Published date: 26-May-2022, DOI: 10.37532/1755-5310.2022.14(3).514
Abstract
Background: Coronary artery dissection occurring during or at the end of the percutaneous intervention may lead to vessel closure and are significantly associated with increased short-term risk of major adverse cardiovascular events. Although the occurrence of final residual dissections has been reduced in the current era. The use of Optical Coherence Tomography (OCT) may show the exact position of the wire and helps prevent serious complications of stenting a long false lumen segment.
Case summary: A 52-year-old male patient presented for inferior ST Elevation Myocardial Infarction (STEMI) after one hour of oppressive chest pain. Coronary angiogram revealed, apart from a significant lesion at the ostium of the first Diagonal branch (Dg) which it was deferred for staged PCI, a 99% lesion of the Left Circumflex (LCX) that was immediately addressed by Primary Percutaneous Intervention (PPCI). One hour after PCI of Dg branch, he developed anterior STEMI and invasive angiogram showed patent stents in LCX and LAD into the Dg with a flush occlusion of the mid LAD just after the stent. The OCT identified the location of wire exiting into the false lumen, and the relative position of the true lumen opposite the carina, allowing redirection of the wire into the true lumen, which was confirmed in a subsequent OCT.
Conclusion: In our patient, balloon angioplasty of the mid LAD induced an iatrogenic edge dissection which caused subsequent artery occlusion either through spiral propagation or inadvertent false lumen wiring. OCT was instrumental in diagnosing these complications and correcting them.
Keywords
Acute coronary syndrome • Primary percutaneous coronary intervention • Optical coherence tomography
Abbreviations
CTO: Chronic Total Occlusion; DES: Drug Eluting Stent; Dg: Diagonal; LAD: Left Anterior Descending Artery; OCT: Optical Coherence Tomography; PPCI: Primary Percutaneous Intervention; STEMI: ST Segment Elevation Myocardial Infarction
Introduction
Residual dissections after percutaneous coronary interventions are associated with increased risk of major adverse cardiovascular events [1]. Overall, final dissections occurred with increased frequency in complex lesions and whenever a balloon-only angioplasty was performed to a side branch [2]. This case illustrates the use of OCT to diagnose and manage a post procedural dissection.
Case Presentation
A 52-year-old male patient presented for oppressive chest pain of one hour duration, radiating to the back. He had no associated symptoms. He had no significant family history of sudden cardiac death, myocardial infarction, or heart failure.
His vital signs were blood pressure, 100/65 mm Hg; heart rate, 70 beats/min; respiratory rate, 18 breaths/min; temperature, 98.6°F; and oxygen saturation of 96% (on room air). On physical examination, the patient appeared in severe pain, although he had clear breath sounds bilaterally, a regular heart rhythm without any murmurs, no peripheral edema, and warm extremities.
Past medical history
He is known to have diabetes mellitus, hypertension, dyslipidemia. He is actively smoker of 1 pack per year for 30 years.
Differential diagnosis
The differential for acute-onset chest pain includes MI, aortic dissection, pulmonary embolism, spontaneous pneumothorax, and musculoskeletal chest pain.
Investigation
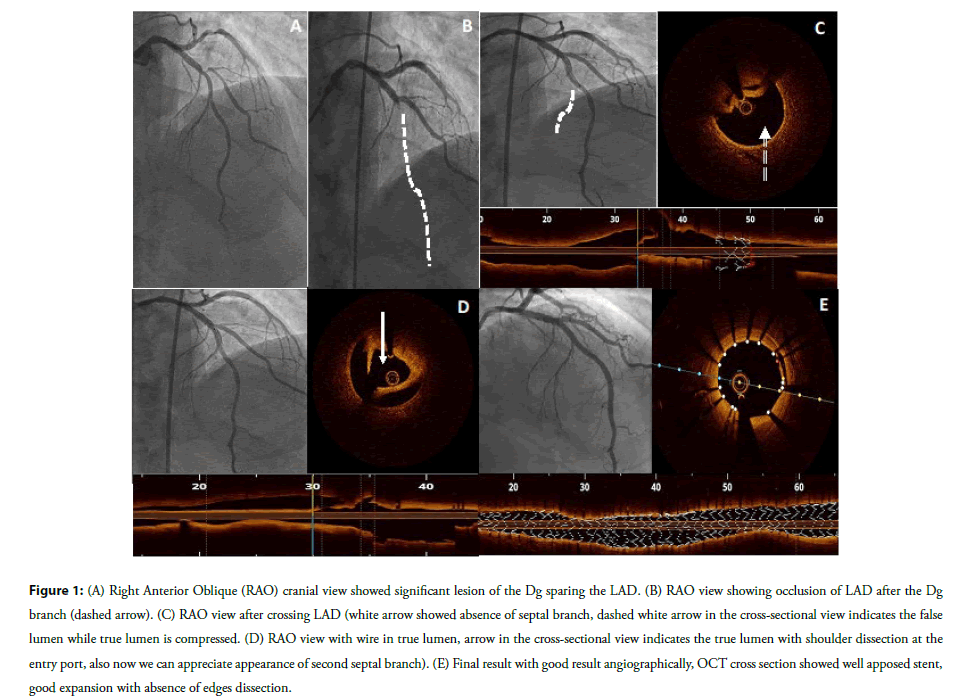
Surface electrocardiogram was consistent with ST-segment elevations in leads II, III, and aVF. He was immediately taken for a coronary angiogram which, apart from a significant lesion at the ostium of the first Diagonal branch (Dg) which it was deferred for staged PCI, revealed a 99% lesion of the Left Circumflex (LCX) (Figures 1A-1E and Video 1).
Figure 1: (A) Right Anterior Oblique (RAO) cranial view showed significant lesion of the Dg sparing the LAD. (B) RAO view showing occlusion of LAD after the Dg branch (dashed arrow). (C) RAO view after crossing LAD (white arrow showed absence of septal branch, dashed white arrow in the cross-sectional view indicates the false lumen while true lumen is compressed. (D) RAO view with wire in true lumen, arrow in the cross-sectional view indicates the true lumen with shoulder dissection at the entry port, also now we can appreciate appearance of second septal branch). (E) Final result with good result angiographically, OCT cross section showed well apposed stent, good expansion with absence of edges dissection.
Video 1: Right anterior oblique cranial (RAO cranial) view showed moderate lesion of the proximal segment Left Anterior Descending (LAD) artery and significant lesion at the ostium of the diagonal branch (Dg).
Management
Culprit lesion in the LCX was immediately addressed by Primary Percutaneous Intervention (PPCI) with one Drug Eluting Stent (DES).
After 24 hrs, provisional stenting technique with 1 DES 3.0 × 20 mm from Left Anterior Descending artery (LAD) into Dg with proximal optimization technique of proximal LAD, opening strut toward mid LAD with final kissing balloon by drug eluting balloon 3.5 at the carina and a 3.0 non-compliant balloon for the Dg. Final angiogram showed excellent result (Video 2).
Video 2: Final result. Left anterior oblique cranial view (LAO cranial).
One hour later, he developed severe chest pain with anterior STEMI and was brought back emergently for invasive angiogram that showed patent stents in LCX and LAD into the Dg with a flush occlusion of the mid LAD just after the stent (Figure 1B and Video 3). A workhorse wire was used to cross the distal occlusion, restoring flow (Video 4). OCT was performed to evaluate the mechanism, identifying both a culprit distal edge dissection, and a wire path in a false lumen for 30 mm before re-entering the true lumen in the distal LAD. The OCT identified the location of wire exiting into the false lumen, and the relative position of the true lumen opposite the carina, allowing redirection of the wire into the true lumen, which was confirmed in a subsequent OCT (Video 5). The LAD was subsequently repaired with 3 DES with excellent result (Figures 1C-1E and Videos 6-8).
Follow-up
Video 3: RAO cranial view showed flush occlusion of the mid LAD artery right after the bifurcation with the Dg. Dg branch is patent.
Video 4: RAO cranial view after passing the wire distally and restoring the flow. We can appreciate the absence of the septal branch.
Video 5: RAO cranial view, rewiring the LAD and appearance of the septal branch.
Video 6: Final result.
Video 7: Final result.
Video 8: Final result.
After intervention, patient went to cardiac care unit for observation. His hospital stay was uncomplicated with no signs of heart failure. He was discharged on dual antiplatelet therapy. His ejection fraction on the day of discharge was 55%.
Results and Discussion
Coronary artery dissection after PCI has decreased from 3% in the balloon angioplasty era to 0.3% in the current era [3]. Treatment includes deployment of a stent to exclude the dissection from the lumen. Intravascular imaging including Intravascular Ultrasound (IVUS), and OCT are useful to confirm the presence and extent of dissection, and plan further interventions. The use of contrast during OCT acquisition might play a role extending the dissection false lumen distally.
There is strong evidence that intravascular imaging modalities play a key role in PCI by improving clinical outcomes and reducing the incidence of MACE [4]. Use of intravascular imaging during the staged PCI may have detected balloon injury related dissection before it caused a clinical event. Once stent failure is identified, use of intravascular imaging to diagnose the underlying etiology is growing [5]. Furthermore, use of intravascular imaging to precisely localize guidewires within an artery (true lumen versus sub intima) has proved valuable in chronic total occlusion intervention, where it can be used to determine the optimal entry point and evaluate guidewire penetration of the proximal cap [6].
In our case, OCT showed the exact position of the wire and helps prevent serious complications of stenting a long false lumen segment. This complication should be recognised initially as treatment improves vessel patency and patient outcome.
Conclusion
In our patient, balloon angioplasty of the mid LAD induced an iatrogenic edge dissection which caused subsequent artery occlusion either through spiral propagation or inadvertent false lumen wiring. OCT was instrumental to understand the mechanism of acute stent failure, diagnose subintimal wire position and correct it. This case highlights the importance of intravascular imaging in identifying the false lumen.
Author Contributions
All authors have contributed into the patient care, manuscript preparation and final approval.
Acknowledgements
I would thank you Dr. Jorge Chavarria and Dr. Gustavo Dutra for their help making the manuscript and the figures.
Disclosures
The authors have nothing to disclose.
Conflicts of Interest
Dr Sibbald is a consultant for Abbott Vascular Inc. None of the other authors have conflicts of interest.
References
- Rogers JH, Lasala JM. Coronary artery dissection and perforation complicating percutaneous coronary intervention. J Invas Cardiol. 16(9): 493-499 (2004).
[Google Scholar] (All versions) [PubMed]
- Biondi-Zoccai GGL, Agostoni P, Sangiorgi GM, et al. Incidence, predictors, and outcomes of coronary dissections left untreated after drug-eluting stent implantation. Eur Heart J. 27(5): 540-546 (2006).
[Crossref] [Google Scholar] [PubMed]
- Venkitachalam L, Kip KE, Selzer F, et al. Twenty-year evolution of percutaneous coronary intervention and its impact on clinical outcomes: A report from the National Heart, Lung, and Blood Institute-sponsored, multicenter 1985-1986 PTCA and 1997-2006 Dynamic Registries. Circ Cardiovasc Interv. 2(1): 6-13 (2009).
[Crossref] [Google Scholar] [PubMed]
- Gatto L, Ramazzotti V, Micari A, et al. Mechanical causes of stent failure: OCT insights. Interv Cardiol J. 3(2): 1-4 (2017).
- Araki M, Yonetsu T, Lee T, et al. Relationship between optical coherence tomography-defined in-stent neoatherosclerosis and out-stent arterial remodeling assessed by serial intravascular ultrasound examinations in late and very late drug-eluting stent failure. J Cardiol. 71(3): 244-250 (2018).
[Crossref] [Google Scholar] (All versions) [PubMed]
- Stone GW, Reifart NJ, Moussa I, et al. Percutaneous recanalization of chronically occluded coronary arteries: A consensus document: part II. Circulation. 112(16): 2530-7 (2005).
[Crossref] [Google Scholar] [PubMed]