Mini Review - Interventional Cardiology (2020) Volume 12, Issue 7
Subclinical atrial fibrillation in patients with cardiac resynchronization therapy caused heart failure hospitalization
- Corresponding Author:
- Mitsuharu Kawamura
Division of Cardiology,
Showa University School of Medicine,
1-5-8 Hatanaodai, Shinagawa- ku,
Tokyo, 142-8555, Japan,
E-mail: mitsuhitoharu@yahoo.co.jp
Received date: October 15, 2020; Accepted date: October 29, 2020; Published date: November 05, 2020
Abstract
Current study reported that early detection and early rhythm control therapy in patient with Atrial Fibrillation (AF) was associated with a lower risk of cardiovascular outcomes than usual care for AF. Early detection and early treatment for AF is important. However, subclinical AF is likely to go undetected and untreated, because patients with subclinical AF had no symptoms. It is unclear the relationship subclinical AF and Heart Failure (HF). This review summarizes the relationship between subclinical AF and HF hospitalization in patients with cardiac dysfunction using Cardiac Resynchronization Therapy Defibrillator (CRT-D).
Keywords
Subclinical atrial fibrillation •Heart failure• Cardiac resynchronization therapy
Introduction
Recently, Kirchhof et al. [1] reported that early detection and early rhythm control therapy in patient with atrial fibrillation (AF) was associated with a lower risk of cardiovascular outcomes than usual care for AF. The Assert study [2,3] showed that subclinical Atrial Fibrillation (AF) was associated with stoke event. However, these studies found no relationship between subclinical AF and heart failure (HF) hospitalization. Furthermore, the relationship between subclinical AF and HF hospitalization is still unclear, and subclinical AF is likely to go untreated in patients with Cardiac Resynchronization Therapy Defibrillator (CRT-D). This review summarizes to investigate the relationship between subclinical AF and HF hospitalization in patients with CRT-D. Furthermore, we clear the mechanism of HF due to subclinical AF.
Detection of Subclinical AF by Device Report
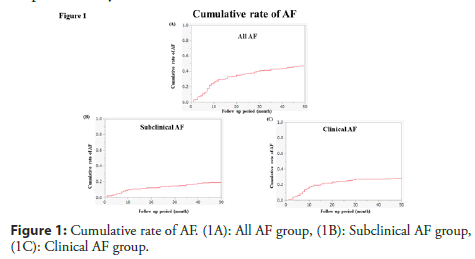
Previous studies have reported that the rate of device-detected subclinical AF is about 10% [2,3]. This study included patients with hypertension and no history of AF, in whom a pacemaker and defibrillator. Recently, we described a higher rate of device-reported subclinical AF (19.6%) [4]. We defined subclinical AF as asymptomatic episodes of AF detected and confirmed by device report and not previously detected by electrocardiographic or ambulatory monitoring. We need to distinguish subclinical AF from atrial high rate episode (AHRE). AHRE was defined as atrial tachyarrhythmia episodes, with frequency >170-190/min and minimum duration of 10-20 successive beats. The numbers of AHRE recorded by device report, more than 90% are in fact subclinical AF episodes, being difficult to define atrial tachyarrhythmia manifestations (atrial flutter, atrial tachycardia). If possible, we try to check the report device and we distinguish subclinical AF from AHRE. We enrolled only patients with CRT-D, and all patients had a low Ejection Fraction (EF). Furthermore, the follow-up period in our study was long. Therefore, it is likely that we found more AF in our study due to the population studied or the duration of follow-up. The detection of subclinical AF was about 10%-20%, these results exceeded our expectations. Figure 1 showed the cumulative rate of AF. The cumulative rate was 49% in all AF, 29% in clinical AF and 19% in subclinical AF for 50 months. Most of clinical AF was detected within a one year. While subclinical AF gradually increased every year. Subclinical AF might be late to detect AF due to without symptoms. Early detect and treatment for AF is very important to us. Home monitoring system might be helpful to early detection of subclinical AF.
Subclinical AF and HF
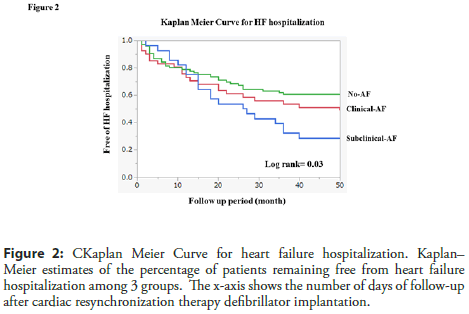
We described the Kaplan Meier curve for HF hospitalization among 3 groups (Figure 2) [4]. HF hospitalization with subclinical AF group had a significantly higher prevalence of HF hospitalization as compared with clinical AF and no-AF group (p=0.03 by logrank). HF hospitalization of rate was 70% in subclinical AF, 49% in clinical AF and 38% in no-AF for 50 months. The Assert study [2,3] did not find a significant relationship between AF and HF. In that study, patients were implanted a pacemaker or ICD and most of patients were normal EF. On the other hand, we described a significant relationship between S-AF and HF hospitalization. Because all patients were implanted CRT-D and had a low EF. AF. Wong et al. [5] reported that in the multivariable analysis, subclinical AF progression was an independent predictor of HF hospitalization. In Wong’s study, almost patients had a normal EF (average EF: 60%) with a pacemaker or ICD. We suspected that subclinical AF did not induce HF hospitalization in patients with pacemarker or ICD, while subclinical AF induced HF hospitalization in patients with CRT-D. If patients with pacemarker or ICD progressed subclinical AF to clinical AF, these patients might induce HF hospitalization.
Figure 2: CKaplan Meier Curve for heart failure hospitalization. Kaplan– Meier estimates of the percentage of patients remaining free from heart failure hospitalization among 3 groups. The x-axis shows the number of days of follow-up after cardiac resynchronization therapy defibrillator implantation.
Mechanism of HF Hospitalization in Patients with Subclinical AF
One potential of the mechanism underling AF progression with HF may be less biventricular pacing due to AF. In our study, biventricular pacing with subclinical AF group was significantly lower as compared to those with no-AF group (subclinical-AF 81% vs. clinical-AF 85% vs. no-AF 94%, p=0.001). Barold et al. [6] reported that uncontrolled ventricular rates reduce the delivery of an optimal of biventricular pacing. A biventricular pacing under 90% was associated with a higher HF hospitalization and death, and a biventricular pacing over 98% significantly reduced HF hospitalization and death. Tachycardia induced cardiomyopathy due to prolonged episodes of subclinical AF may be an important factor in some patient [7,8]. Atrial systole constitutes a considerable proportion of the cardiac output in patients predisposed to HF, and its loss during episodes of subclinical AF might also account for some of the observed increase in HF risk. Furthermore, inappropriate device therapies may induce HF hospitalization. We described that 14% in patients with subclinical AF received inappropriate therapies, 9% in patients with clinical AF received inappropriate therapies, and 7% in patients without AF received inappropriate therapies [4]. Poole et al. [9] reported the occurrence of inappropriate ICD shock was associated with a significant increase in the risk of death as compared with no inappropriate shock. The most common cause of death among patients who received any ICD shock was progressive HF. We summarized the possibility factors of HF.
• Loss of biventricular pacing
• Loss of atrial systole
• Inappropriate device therapy
• Tachycardia induced cardiomyopathy
However, Further studies will be required to be certain the relationship between S-AF and HF hospitalization.
Conclusion
Subclinical-AF after CRT-D implantation was associated with a significantly increased risk of HF hospitalization. The loss of the biventricular pacing and increasing an inappropriate therapy might affect the risk of HF hospitalization. Early detect and treatment for subclinical AF help to reduce HF hospitalization.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med. 383: 1305-1316 (2020).
- Healey JS, Connolly SJ, Gold MR, et al. ASSERT Investigators. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. 366(2): 120-129 (2012).
- van Gelder IC, Healey JS, Crijns HJGM, et al. Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 38(17): 1339-1344 (2017).
- Arai S, Kawamura M, Gokan T, et al. Relationship between device-detected subclinical atrial fibrillation and heart failure in patients with cardiac resynchronization therapy defibrillator. Clin Cardiol. (2020).
- Wong JA, Conen D, Van Gelder IC, et al. Progression of Device-Detected Subclinical Atrial Fibrillation and the Risk of Heart Failure. J Am Coll Cardiol. 71(23): 2603-2611 (2018).
- Barold SS, Herweg B. Cardiac Resynchronization in Patients with Atrial Fibrillation. J Atr Fibrillation. 8(4): 1383 (2015).
- Phan TT, Abozguia K, Shivu GN, et al. Increased atrial contribution to left ventricular filling compensates for impaired early filling during exercise in heart failure with preserved ejection fraction. J Card Fail. 15(10): 890-897 (2009).
- Ellis ER, Josephson ME. Heart failure and tachycardia-induced cardiomyopathy. Curr Heart Fail. 10(4): 296-306 (2013).
- Kirchhof P, Breithardt G, Aliot E, et al. Personalized management of atrial fibrillation: Proceedings from the fourth Atrial Fibrillation competence NET work/European Heart Rhythm Association consensus conference. Europace. 15(11): 1540-1556 (2013).