Clinical images - Imaging in Medicine (2017) Volume 9, Issue 5
Subglottic stenosis in granulomatosis with polyangiitis (Wegener granulomatosis)
Bo-Nien Chen* and Kuo-Sheng Lee
Department of Otolaryngology-Head and Neck Surgery, Hsinchu MacKay Memorial Hospital, Hsinchu City, Taiwan
- *Corresponding Author:
- Bo-Nien Chen
Department of Otolaryngology-Head and Neck Surgery
Hsinchu MacKay Memorial Hospital Hsinchu City, Taiwan
E-mail: chenbonien@yahoo.com.tw
Abstract
Keywords
Wegener granulomatosis ▪ subglottic stenosis
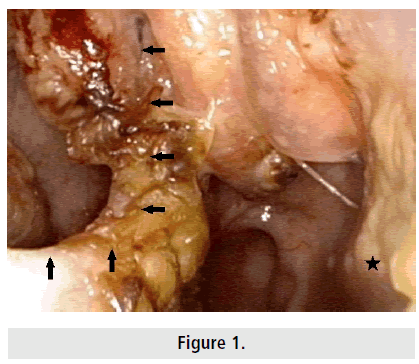
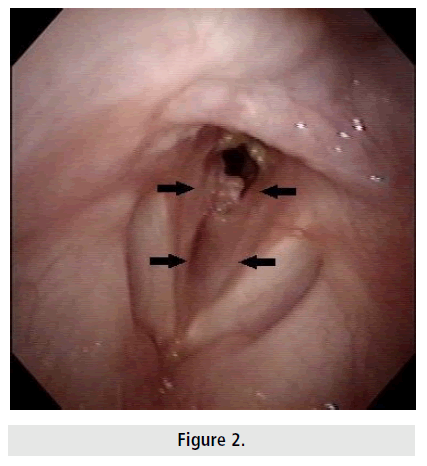
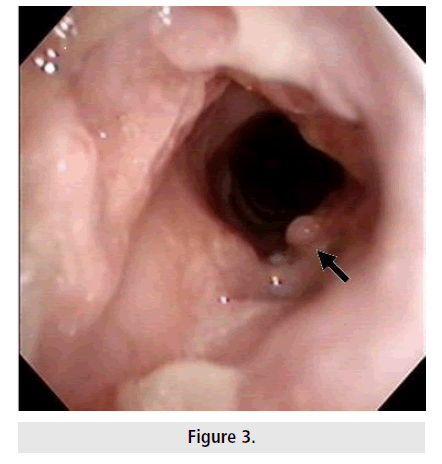
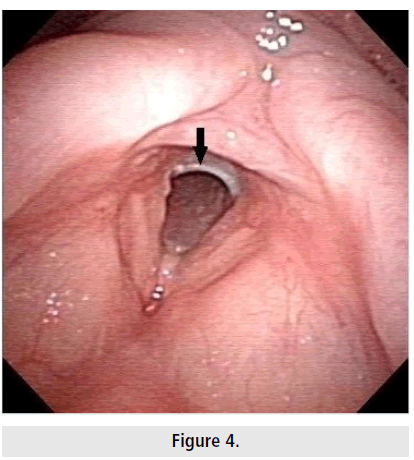
A 36 year old woman presented with a 1 year history of nasal obstruction, exertional dyspnea with biphasic stridor and 10 kg unintentional weight loss. Laboratory investigations revealed that her hemoglobin level was 8.1 g/ dL and erythrocyte sedimentation rate was 41 mmph. Her anti-neutrophil cytoplasmic antibodies were positive. Chest radiograph revealed a small faint patch over left upper lung. Sinoscopy revealed a roomy nasal cavity caused by atrophy of the mucosa, thick discharge, lots of dark yellow crusts, epistaxis and a large perforation of the nasal septum. These findings suggested atrophic rhinitis complicated with perforation of the nasal septum (FIGURE 1 arrows: perforation of the nasal septum, asterisk: atrophy of the inferior turbinate). Bronchoscopy revealed approximately 80% stenosis of the subglottis (grade III, Cotton-Myer grading system) (FIGURE 2 arrows) and long-segmental subglottic granulomatous masses involving the glottis (stage IV, McCaffrey classification system) (FIGURE 3 arrow). An impending life-threatening subglottic stenosis was noted. Therefore, the patient underwent ventilation bronchoscopy and laryngotracheal reconstruction with a T-tube (Montgomery®, Standard Safe- T-Tube™, size 11) stent below the vocal cord (Figure 4 arrow). Postoperatively, granulomatosis with polyangiitis (GPA), formerly known as Wegener granulomatosis, was diagnosed on the basis of clinical features and histological evidence of necrotizing vasculitis and granulomatous inflammation [1]. The patient’s dyspnea was greatly improved by the surgical intervention alone. The patient did not have any vasculitic manifestation except for respiratory tract at 1 year close followup. Guardiani et al. observed 31% patients with GPA presented with subglottic stenosis as part of their initial manifestation. The majority of patients had concurrent sinonasal involvement [2]. Jordan et al. observed 78% patients with GPA presenting with subglottic stenosis were women [3]. Subglottic stenosis is a common and significant presenting manifestation of GPA. Awareness of subglottic stenosis in patients with GPA is essential to avoid delayed diagnosis or lifethreatening crisis.
References
- Lutalo PM, D'Cruz DP. Diagnosis and classification of granulomatosis with polyangiitis (aka Wegener's granulomatosis). J. Autoimmun. 48, 94-98 (2014).
- Guardiani E, Moghaddas HS, Lesser J et al. Multilevel airway stenosis in patients with granulomatosis with polyangiitis (Wegener's). Am. J. Otolaryngol. 36, 361-363 (2015).
- Jordan NP, Verma H, Siddiqui A et al. Morbidity and mortality associated with subglottic laryngotracheal stenosis in granulomatosis with polyangiitis (Wegener's granulomatosis): A single-centre experience in the United Kingdom. J. Laryngol. Otol. 128, 831-837 (2014).