Interview - Interventional Cardiology (2013) Volume 5, Issue 5
Taming coronary chronic total occlusions
- Corresponding Author:
- Chad Kugler
BridgePoint Medical, Two Scimed Place
Maple Grove, MN 55311, USA
E-mail: chad.kugler@bsci.com
Abstract
▪What attracted you to a career in interventional cardiology?
Good question, I think for me, interventional cardiology provides an opportunity to have an impact in medicine and on patients’ lives. Heart disease remains the number one cause of death; interventional cardiology provides the least invasive procedures and an opportunity for patient treatment. Interventional cardiology historically relies heavily on devices, technologies and techniques, so there has always been, and continues to be, great opportunity for device innovation. Cardiologists also have a history of focusing on devices; it has always been a fast moving area of medicine, so the interest of physicians in new technologies has always been very high. It is a fertile ground for new patient treatments and device innovation, making interventional cardiology an exciting opportunity to create new technology companies.
▪ Can you explain a little bit about your career background so far?
I have a Bachelor of Science in mechanical engineering and have been working on medical devices since the early 1990s. I started my career in medical devices at SciMed Life Systems (MN, USA) where, back in the early days of cardiology, everything seemed possible. There were significant unmet clinical needs and there were a lot of new device innovations. As a young innovator, I found the environment very exciting and was inspired to focus on medical technology as a career path. During those early days and throughout my career, I have had the opportunity to develop strong relationships and collaboration with physicians/researchers working at the cutting edge of medicine. In my experience, physicians are always striving to advance medicine where an entrepreneur with new ideas is well received within the medical community. Utilizing these partnerships along with my engineering background and inventive nature, I have been able to learn different areas of medicine and provide innovative solutions to address unmet clinical problems. I left SciMed Life Systems/Boston Scientific (MA, USA) in the late 1990s and have spent the bulk of my career from 1997 until now with early stage innovative technologies and companies including Teramed (MN, USA; aortic aneurysms), Torax (MN, USA; acid reflux) and Prospex (MN, USA; medical device incubator). These opportunities provided a broad experience in engineering, medical technology, regulatory, clinical, business and finance and provided the launch pad for BridgePoint Medical (MN, USA) and my work in coronary and peripheral chronic total occlusions (CTOs) back in 2007.
▪What is your proudest career achievement to date?
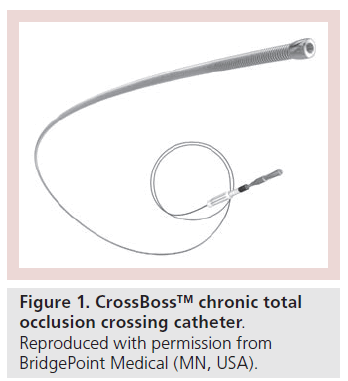
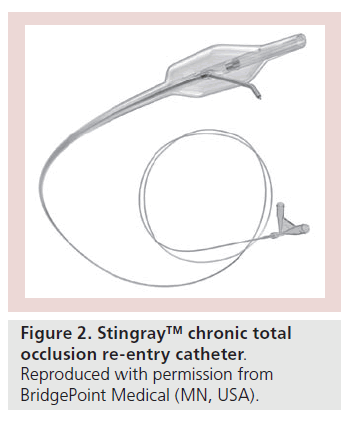
BridgePoint is the company and technology that has had the most success and is the crowning achievement in my career thus far. The CrossBoss™ and Stingray™ (BridgePoint Medical) devices address patients with a very challenging disease state, completely blocked arteries and help facilitate less invasive interventional treatment (Figures 1 & 2). Completely blocked arteries or CTOs are usually treated using invasive bypass surgery or are left alone where the symptoms are managed by medications. The BridgePoint devices and associated interventional techniques facilitate the broad treatment of these patients in the catheterization laboratory and provide a third option for this underserved and often suffering population. Over the past few years, we have watched the BridgePoint devices serve as a nidus to mainstream CTO percutaneous cardiac intervention (PCI). The devices have enabled physicians to achieve a significant level of success in these highly challenging cases. BridgePoint is the proudest achievement in my career thus far, owing to the impact its technology has had on patients’ lives; we have been able to reduce the need for surgery and treat patients who were otherwise untreatable by common or traditional means. Very few companies and technologies have had such a significant impact and it has been a privilege to be involved with the CTO PCI community.
▪ This issue of Interventional Cardiology specifically focuses on CTO. In your opinion, what has been the most important advancement in the treatment of CTO over the last decade?
The first contribution, from research and publication over the past decade, is the fact that CTO treatment is good for patients and that when you put a drugeluting stent across CTOs, arteries remain widely patent. Over the years, there have been many contributions from around the world, in particular, Japan, Europe and the USA, publishing different experiences either from a single patient experience to broader registries tracking survival and other chronic end points. During this process, interventionalists have proven that revascularizing a CTO reduces symptoms and is good for patients in the long term. This work continues with ongoing registries that are prospectively tracking patient outcomes for years postprocedure.
The next big challenge involves crossing the occlusion in an effort to place a drug-eluting stent in place across a CTO. These occlusions tend to be very long and calcified, they have a challenging level of disease and have often been occluded for years.
The second contribution is the retrograde approach synthesized by Japanese interventionalists. They took a lead position over a decade ago in creating a technical understanding of how to get tools beyond CTOs. Retrograde CTO PCI enabled high success rates, but the procedure takes significant time and persistence, is quite challenging and difficult to teach broadly. These methods ended up taking too much time, too much effort and not all physicians have been able to replicate the success rates of the Japanese. Technical challenges aside, these methods have shown the interventional community that CTO PCI is possible in a broad array of patients with diffuse disease.
The third advancement concerns the BridgePoint devices and associated techniques that have been refined by a select group of US and EU interventionalists. This approach allows for a broader array of cases to be treated using a less technically challenging antegrade approach. These devices simplify CTO PCI and help the procedures meet the criteria of safety, efficacy, cost and time constraints of western catheterization laboratories.
Along with BridgePoint, a training methodology was established called the hybrid algorithm. The hybrid algorithm enables physicians to make the best decisions on the techniques and devices to use according to angiographic criteria. Bridge- Point and hybrid algorithm have allowed CTO PCI to be moved more and more into mainstream in medicine.
▪ You cofounded BridgePoint Medical, can you explain a little bit about the company and the progress it has made since its conception?
We have humble beginnings similar to many start-up medical device companies; we were meagerly funded with a few ideas that we thought were promising. The CTO PCI opportunity developed over time as we iterated on different ideas and approaches. The early days included a consolidated team of talented engineers focused on proving that we could add value to CTO crossing. We did significant cadaveric research in those days to refine the devices and prove our approach would meet the clinical need. As we started discussing the approach of subintimal crossing and the ideas of CrossBoss and Stingray, many in the interventional community thought we were a bit crazy. A few visionary physicians saw the value of what we were working on and ‘took us under their wing’, including Pat Whitlow from the Cleveland Clinic (OH, USA), Bill Lombardi from PeaceHealth (WA, USA), Craig Thompson from Yale University (CT, USA) and Michael Wyman from Torrance Memorial (CA, USA). We iterated and refined the devices rapidly over approximately 1.5 years, starting in 2007 and executing our first-in-man experience in South America in 2008. Our first-in-man experience was instrumental and put us on a path for successful EU and US clinical trials in 2009 and 2010 and commercialization starting in 2011. By the end of 2012, BridgePoint devices were in over 200 hospitals worldwide and growing. Our commercial success caught the attention of many of the larger medical device companies. We were acquired by Boston Scientific in October of 2012.
▪ You mentioned the devices; can you explain firstly about the design and function of the CrossBoss catheter and then the Stingray.
The CrossBoss is designed to rapidly and safely move beyond a CTO. A completely closed artery is difficult to see under angiography where two major challenges in CTO crossing are vessel perforation and uncontrolled dissections. The CrossBoss has the ability to get across these vessels while staying within the vessel structure and minimizing the disruption along the way. These two features of the device help it safely and effectively get across and beyond very challenging long and diffuse CTOs. In many cases the CrossBoss goes from true lumen where blood is, across the vessel to the true lumen beyond the CTO. There are also times when the device ends up finding tissue planes, a very common occurrence in treating CTOs, and we need to steer back toward the center of the vessel. In this situation, the Stingray, the second device in our suite of tools, is used to steer back into the true vessel lumen.
The Stringray is an over-the-wire balloon catheter that has the ability to align itself with the circumference of the vessel. It does this using a flat shape balloon that naturally aligns upon inflation. From this device, the physician is able to gain certain orientation angiographically aligning the C-arm to the balloon. The physician is then able to accurately steer a speciality guidewire from a tissue plane back into the true lumen and beyond the CTO. The CrossBoss and Stingray in concert are able to address many of the major obstacles that the physicians see when crossing CTOs. Crossing is the main challenge in CTO PCI treatment, then the physician can use the tools, techniques and devices they use in regular angioplasty to ultimately open the CTO.
▪ Can you explain what the aims of the FAST-CTOs trial was with these devices?
The aim really is proving safety and efficacy of the device. It was a US Investigational Device Exemption trial with the aim of providing evidence to the US FDA, in an effort to get approval in the USA.
▪What were the inclusion criteria for this trial?
The most important inclusion criteria surrounded occlusion difficulty where the FDA required a crossing attempt using guidewires. The FDA wanted us to make sure this lesion was truly a CTO; one that was challenging to treat. There were obviously other criteria regarding patient symptoms, as well as angiographic criteria, that were modeled after similar FDA clinical trials.
▪What were the primary end points that you were looking for?
Safety and efficacy, which in clinical trial terms, are predefined levels of complications and procedural success compared with historical published literature controls. To gain approval we needed to have greater than 59% crossing success and less than 6.9% 30-day major adverse cardiac events (MACE).
▪What sort of time frame did you do this over and what results did you see?
It took 1.5 years to enroll the trial in 2009 and early 2010. The devices achieved a 77% overall efficacy defined as a guidewire beyond the CTO (wire in the distal true lumen). The interesting thing was that the investigators improved as they refined their technique, so the second half of the trial ended up getting 87% overall success. There was a slight learning curve, but both 77 and 87 are great measures of success in a refractory patient population. The other primary end point was safety, which was defined as 30-day MACE. We achieved a MACE rate of 4.8% which compares favourably against historical controls. Both end points were met and both are end points that we are quite proud of.
▪Were they expected results or better than expected?
I think that from our extensive cadaver preclinical work and our early clinical experience in South America, we knew the devices would be quite successful and safe, so the results met expectations.
▪What does the future hold in terms of treatment of CTOs after these trials?
A number of things, but most important is supporting and training physicians to effectively treat CTOs. There are a few techniques and tips associated with CTO PCI and the BridgePoint devices that are new to physicians. BridgePoint and Boston Scientific are now in the process of providing training courses to physicians who want to learn how to effectively use the devices. The next phase for technology is worldwide adoption, hospital by hospital, physician by physician, really expanding the practice and having the opportunity to treat every symptomatic CTO patient.
▪How do you plan to carry out this expansion?
It is a stepwise process, we have a significant number of regional courses, which are live demonstration courses that we support in the US and Europe and we are starting that process in Asia. We have physicians come in and watch experts and learn from them in the devices and techniques. So it is a matter of expanding out those courses to meet the worldwide need and to train as many physicians as we can in a high-quality way, each and every year. We expect it to take approximately 3–4 years to be able to teach and train physicians at each hospital in a way that they can then treat the patients with symptomatic CTOs with the best medical care. Therfore, this year we focused on the USA and Europe and in 2014, 2015 and probably 2016 for the rest of the world, for example, Asia and Australia. So it is really a matter of stepwise growth of physician technique and experience of physicians, to make sure they have access to the technology and that they are using it effectively.
▪ In general, what progress do you expect to be made in the treatment of CTOs in the next 5 years?
It is hard to predict, but I think that first, the clinical evidence will increase. There are a number of registries currently underway in Japan and Europe, and Boston Scientific is sponsoring registries in Europe and in the USA in an effort to provide all of the objective evidence from which patients can benefit from CTO PCI. There will be increasing and high-quality clinical evidence. Second, is that there is still a ton of opportunity for devices, be it drug-eluting stents, or the devices used to cross the CTO themselves will also improve in the next 5 years and as this now becomes mainstream, there will be more and more physicians, companies and engineers focused on tools for CTO PCI.
I think ultimately in the next 5 years, we will come to a point where every CTO can be treated by a larger number of physicians who will access patients who need this form of therapy. I think all physicians treating CTOs are looking for total revascularization, so that every artery is open, that physicians walk away from the table having every major coronary vessel treated in a way that is high quality and I think in the next 5 years that quest for total revascularization will be achieved.
Disclaimer
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of Future Medicine Ltd.
Financial & competing interests disclosure
C Kugler is an employee of BridgePoint Medical and Boston Scientific. He owns stock in BridgePoint Medical, Torax and Apnex. He has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.