Short Article - Interventional Cardiology (2010) Volume 2, Issue 2
The Austrian Multivessel Taxus̢̢̉ Stent (AUTAX) registry
- Corresponding Author:
- Mariann Gyöngyösi
Department of Cardiology
Medical University of Vienna
Währinger Gürtel 18–20, A-1090 Vienna, Austria
Tel: +43 1 40400 4614
Fax: +43 1 40400 4216
E-mail: mariann.gyongyosi@meduniwien.ac.at
Abstract
Keywords
angiography, CABG, coronary artery, drug-eluting stent, multivessel disease, outcome, Taxus™
Multiple drug-eluting stent implantation or coronary artery bypass surgery for multivessel disease
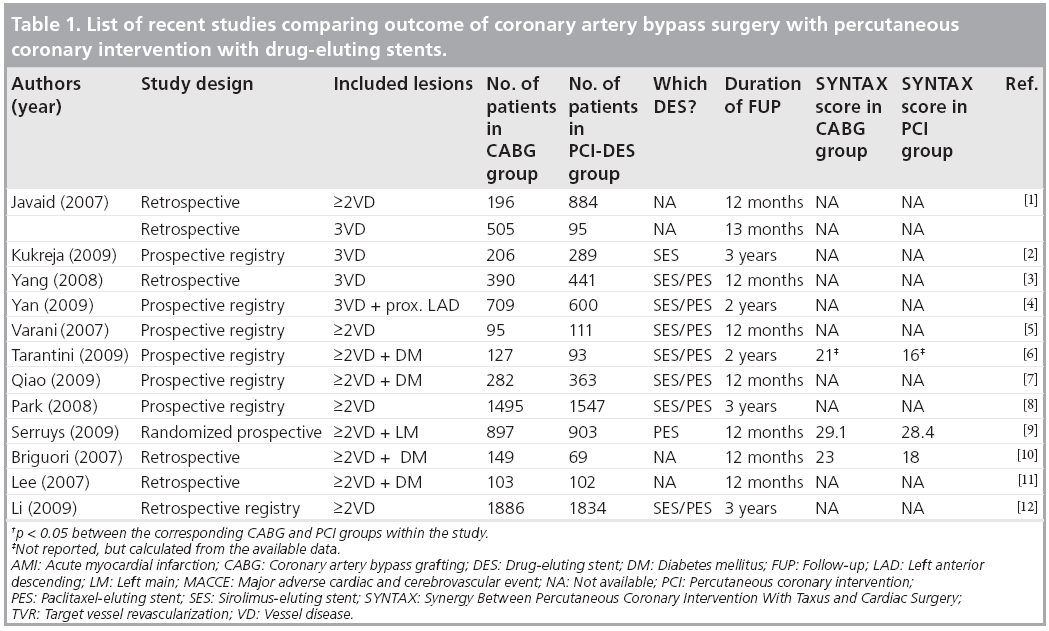
The individual decision of treating coronary artery multivessel disease with either percutaneous transluminal coronary intervention (PCI) using drug-eluting stents (DES) or coronary artery bypass surgery (CABG) is mainly based on coronary anatomy (e.g., complete vessel occlusion, left main, bifurcation or proximal left anterior descending coronary lesions), left ventricular function, coexisting diseases and patient preference. The considerably difference in the lesion anatomy treated by PCI or CABG results in biased comparisons of long-term outcomes of the two treatment arms, and is based mainly on retrospective data analysis or prospective registries, with only a limited number of prospective randomized trials (Table 1) [1–12]. These trials have demonstrated superior long-term outcome in CABG compared with PCI with DES, recommending CABG as the gold-standard treatment for multivessel disease in current guidelines.
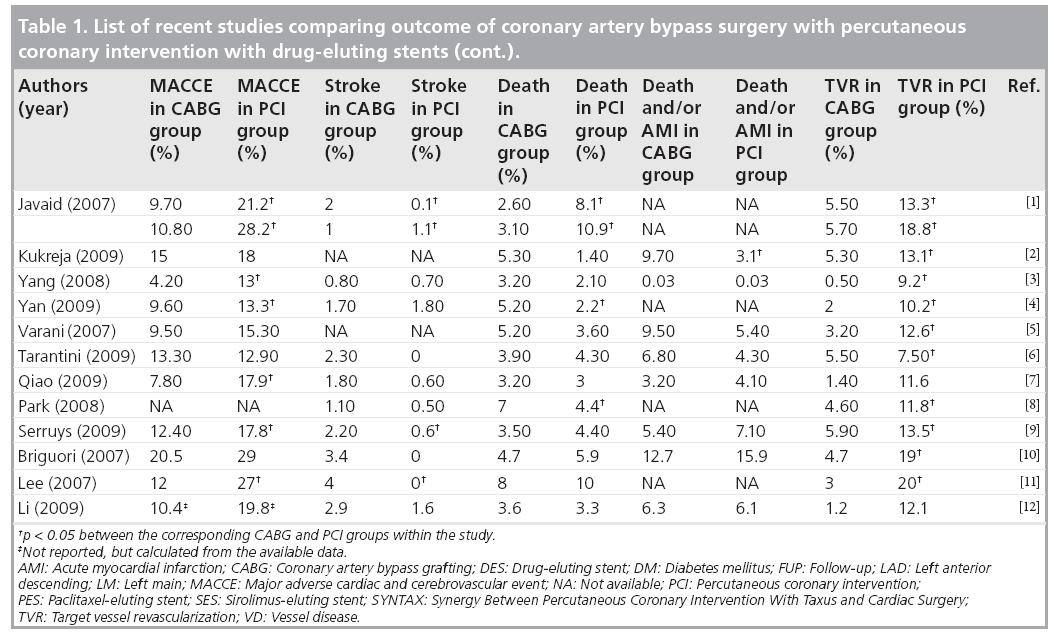
Table 1: List of recent studies comparing outcome of coronary artery bypass surgery with percutaneous coronary intervention with drug-eluting stents.
Table 1a: List of recent studies comparing outcome of coronary artery bypass surgery with percutaneous coronary intervention with drug-eluting stents (cont.).
Every trial has reported significant benefit in target lesion or vessel revascularization, similar or reduced mortality or acute myocardial infarction (AMI) rate, but also a significantly higher rate of stroke in the CABG groups. However, even if the composite of major adverse cardiac and cerebrovascular events (MACCE) is significantly lower after CABG, the consequences of repeat PCI (for the PCI arm) or stroke (for the CABG arm), regarding disability and quality of life, are different. While repeat revascularization is relatively benign, and generally treatable, stroke is one of the most feared complications by patients. Thus, the reduction of stroke occurrence with PCI compared with CABG is clinically relevant [13].
The risk of acute stent thrombosis with its eventually fatal consequence, or the still unknown very long-term outcome of implantation of DES (a drawback of DES), along with improved surgical techniques such as minimalinvasive or off-pump surgery, leads to a decision for bypass surgery in many patients. However, graft closure rates are approximately 35% for vein grafts and 8% for left internal mammary artery grafts after 1 year; thus, the clinical outcome can be as severe as the acute stent thrombosis, although most of the surgically related events remain asymptomatic [14].
Usefulness of registries adding complementary information to randomized trials
The key features of the prospective registries on multivessel disease are the inclusion of ‘all comers’, not excluding patients with post-PCI or post-CABG lesions. Typically for medical product device prospective randomized studies, the window of patient recruitment is generally narrow, with numerous restrictive inclusion and extensive exclusion criteria, resulting in enrollment of selected patients with a relatively lower risk for adverse events.
The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) randomized prospective trial employed an ‘all comers’ design [9]. However, Rastan et al. reported interesting insights from single-center enrolment in the SYNTAX study [15]. Within a certain screening period, a total of 694 patients presented three-vessel disease and/or significant left main (LM) lesion, of which 271 (39%) had previous CABG and 232 (33%) previous PCI treatment, which were the main exclusion criteria of SYNTAX, and only 9.7% of patients were definitively included at this site [15]. These rates are similar to previous randomized controlled trials of PCI versus CABG, in which randomization rates ranged between 2 and 12% [16,17].
In addition, patients enrolled into a randomized trial should be treated in accordance with the prespecified schema of the study. By contrast, the registries, with their real-world practice, mirror the diversity of treatment modalities between countries, as revealed by the run-in phase of the SYNTAX trial [18]. For example, in the USA, PCI for LM and/or threevessel disease was performed in 18% of the cases, while in Europe it was performed in 29% of the cases [18].
One of the main points of divergence is due to the fact that prospective randomized trials aim to create new treatment standards and guidelines, while registries are descriptive, calling attention to unrecognized phenomena.
The AUTAX registry
▪ Study design
The multicenter Austrian Taxus™ Multivessel (AUTAX) registry (ClinicalTrials.gov number NCT00738686) was a prospective academic nonrandomized Austrian study, including patients with multivessel disease in ‘real-world’ settings, treated solely with Taxus stents [19]. The study was conducted in eight Austrian medium- and high-volume PCI centers, with the objectives of 6‑month angiographic, and short- (30 days), medium- (6 months) and long-term (1 and 2 years) clinical outcomes. In contrast to the SYNTAX study and the PCI Registry, the AUTAX registry also included patients with previous PCI and/or bypass surgery.
Summary of methods
The main inclusion criteria were multivessel disease with two or more lesions in two or more different vessels and the possibility of complete revascularization by PCI. Complete revascularization was defined as restoration of Thrombosis In Myocardial Infarction flow grade 3 with residual stenosis of less than 30% to all myocardial territories. The main exclusion criteria were ST-segment elevation myocardial infarction within 48 h, cardiogenic shock, noncompliance with the study protocol or expected survival time of less than 2 years.
The clinical decision of treatment mode (PCI or CABG) was based on the individual patient’s clinical parameters and angiographic morphology, aiming for complete revascularization. CABG was indicated for patients with complex coronary anatomy or chronic total occlusion untreatable with PCI.
The primary end point of the registry was the occurrence of MACCE during the 2-year clinical follow-up. The secondary end points included the breakdown primary end point events, the acute, subacute and late thrombosis rates, and the angiographic end points, such as binary restenosis rate and late lumen loss per lesion.
Based on clinical considerations due to multivessel stenting, all patients were requested to return to angiographic follow-up at 6 months after PCI. Clinical control was performed at 30 days and at 1 year. All patients with clinical symptoms or positive exercise tests were controlled angiographically, and the standard post- PCI care was recommended, in accordance with the relevant guidelines [16,20]. A routine exercise test was performed at the discretion of the treating physician.
The SYNTAX score was calculated for lesions treated with PCI, and additionally, for significant lesions that were untreatable for any reason [21].
Summary of results
A total of 441 patients (mean age of 64 years, 78% male) with 1080 lesions were prospectively included in the registry. Diabetes mellitus, hypertension, hyperlipidemia and smoking were noted for 31.7, 81.2, 74.6 and 33.6% of patients, respectively. The indication for PCI was unstable angina/non-ST elevation myocardial infarction (UA/NSTEMI) in 34.9% of patients. Previous PCI or CABG were performed in 38.8 and 3% of patients, while 26.8% of these patients had restenotic lesions and were treated with complex PCI in the AUTAX registry.
The total 1080 lesions (2.45 ± 0.31 lesions/ patient) were treated with TAXUS stents (n = 1401, 3.18 ± 0.24 stents/patient). LM and ostial lesions (left and/or right) were treated in 6.8% and 10.2% of patients, respectively. PCI of bifurcation lesion, chronic total occlusion and of small vessels were performed in 19.0, 15.2 and 32.7% of patients, respectively. The number of patients with one or more, or two or more lesions for off-label indication was 80.1 and 59.3%, respectively. Lesion length over 100 mm was measured in 35.4% of patients.
The stent:lesion ratio was 1.3 ± 0.2, the implanted stent size 2.9 ± 0.4 mm, and the stent length was 25.8 ± 9.7 for a mean lesion length of 19.9 ± 12.6 mm. Type A, B1, B2 and C lesions were recorded in 11.8, 39.3, 31 and 17.9% of the lesions (n = 1080), respectively. The mean stent inflation pressure was 14.1 ± 2.9 atm. Predilation was performed in 24.8, 21.0 and 37.9% of the first, second and third lesions and postdilation in 26.8, 25.3 and 14.5% of the first, second and third lesions, respectively. However, control of stent apposition with intravascular ultrasound was not reported.
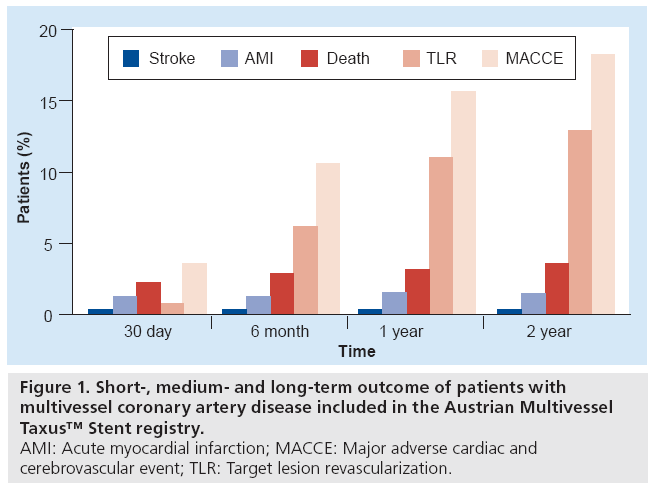
Complete revascularization could be achieved in 90.5% of patients. LM PCI was performed in 6.8% of the cases. The stent:patient ratio was 3.18 ± 0.24. Control angiography at 6 months was performed in 78% of patients, which revealed mainly in-stent restenosis with isolated (without in-stent) edge peri-stent restenosis in 1.6% of lesions, and a binary restenosis rate of 10.8%. Clinical control at 2 years was carried out in 95.7% of included patients. The acute, subacute and late thrombosis rates were 0.7, 0.5 and 0.5% respectively. Even if the stent thrombosis was not defined in the original AUTAX paper, all of the stent thromboses (three acute, two subacute and two late thromboses) were treated with target lesion revascularization (TLR), therefore all stent thromboses were definitive, as verified by angiography [22]. Figure 1 presents the 30‑day, the 6‑month, and the 1- and 2‑year follow-up composite MACCE of the study. Patients with LM PCI (n = 30) had a somewhat higher MACCE rate compared with patients without LM PCI (30 vs 16.5%, statistically nonsignificant difference).
Figure 1: Short-, medium- and long-term outcome of patients with multivessel coronary artery disease included in the Austrian Multivessel Taxus™ Stent registry.
AMI: Acute myocardial infarction; MACCE: Major adverse cardiac and cerebrovascular event; TLR: Target lesion revascularization.
Calculated SYNTAX score showed skewed distribution. Due to the lack of guidelines, the scores for stenosis of bypass vessels or restenotic lesions, or for vessels with previous successful PCI could not be calculated. The range of the cumulative SYNTAX score was 12.0–56.5 (median 23.0). SYNTAX score did not predict TLR or MACCE, probably due to the lack of restenotic or bypass stenoses (29.8%) scores, or to the underscoring of the right coronary artery lesions at right coronary dominance. Receiver operator characteristic analysis of SYNTAX score could not identify a clear cut-off value predictive of TLR or MACCE occurrence.
The multivariate Cox regression model resulted in significant predictors of 2‑year MACCE, including age over 70 years and UA or NSTEMI at the clinical presentation in the AUTAX registry. Previous PCI/CABG and incomplete revascularization exhibited a time dependence for prediction of MACCE. Diabetes mellitus and previous PCI showed a borderline significance in predicting MACCE. Furthermore, Cox analysis identified UA or NSTEMI and incomplete revascularization as significant variables for mortality.
The SYNTAX score
The SYNTAX score is a classification system created for detailed description of the anatomical severity of coronary artery disease as an aid to decision making for selection of patients for PCI or for CABG [21]. The SYNTAX study demonstrated significantly higher postprocedural MACCE rates for PCI patients with SYNTAX scores greater than 33 [9]. Van Gaal et al. reported further prognostic importance of the SYNTAX score for periprocedural infarction, with increasing predictive value as the score rises [23]. By contrast, the SYNTAX score failed to predict the outcomes in the AUTAX registry, and no cut-off value could be found predicting MACCE. The AUTAX registry revealed many important failures of the present scoring system, such as failing to score post-PCI lesions and restenotic or bypass lesions. Furthermore, the TLR of a left anterior descending or right coronary artery lesion is equivalent, but the original right coronary artery lesion had a much lower SYNTAX score. Bearing these facts in mind, it is understandable that the patients with a relatively low SYNTAX score (between 19 and 23) had a similar MACCE rate as did patients with the highest scores of more than 29.0 [19].
In addition, a SYNTAX score threshold of 34 identified a cohort of patients with LM disease who can benefit most from surgical revascularization, as indicated by decreased mortality [24,25]. By contrast, Lemesle et al. reported the failure of the SYNTAX score in the prediction of clinical outcome after CABG [26]. Furthermore, patients of the SYNTAX study with higher SYNTAX score in the CABG Registry arm (mean score: 37.8) did not experience higher mortality or combined end point rate compared with the patients randomized to CABG (mean score: 29.1) [9].
The SYNTAX score is based on a purely morphological description of the lesions, without evaluation of the functional status of the lesion and the morbidity of the patient (e.g., older age, diabetes mellitus, low ejection fraction, pulmonary and renal diseases, procedural factors and UA/NSTEMI), which are known to be strong predictors of cardiovascular events after CABG or PCI [27–30]. These predictors should be simultaneously used with the SYNTAX score and should have an additive value to the risk evaluation of patients with multivessel disease.
Successful PCI leads to a decreased SYNTAX score, correctly indicating an improved outcome postrevascularization. A reasonable procedure to identify patients with unresolved high risk of MACCE would be the re-evaluation of SYNTAX scores after PCI or CABG [31]. However, no score system exists for post-PCI or post-CABG lesions, or for lesions with unsuccessful coronary interventions. The SYNTAX score system leaves several unresolved questions, for example, how should a native lesion after CABG be scored, if the bypass surgery was successful, if the bypass vessel gets occluded and the original lesion to be treated with PCI.
Conclusions: what does AUTAX add to the present practice of multivessel PCI?
A total of 441 of the 1012 screened patients (43.6%) were included in the AUTAX registry, which is a much higher rate than the previously presented registries [19,32–36]. This is mainly due to the inclusion of patients with previous coronary procedures, such as 38.8% with previous PCI and 3% with CABG. Moreover, restenosis at least in one vessel should have been treated in 26.8% of all patients. This presents the real-life practice in catheterization laboratories; that is, many patients with multivessel coronary lesions have already undergone previous coronary procedures. Indeed, the rapid increase in the number of PCI procedures changes the anatomy of coronary lesions continuously, resulting in a complex morphology of coronary artery disease with restenosis, remodeling and phenotypic modulation of intima post-stenting [19,37,38]. Previous PCI or CABG exhibited time dependence for prediction of MACCE. Accordingly, the AUTAX registry shows that lesions subsets, other than de novo, should also be included in prospective randomized trials, as these anatomic features will dominate the multivessel coronary procedures in the very near future.
Unstable angina/NSTEMI at clinical presentation predicted the 2‑year MACCE, and was also a predictor for all-cause mortality or mortality and AMI, which calls attention to the high-level care of these patients.
The AUTAX registry included only patients with possible complete revascularization, with the selection bias of excluding patients with nontreatable lesions for PCI, while offering CABG, and including patients with an a priori assumed high angiographic success rate. A predictable failure for complete revascularization by PCI was an indicator for CABG. Therefore, even if the selection of patients for PCI in the AUTAX trial appears biased, it still mirrors the real-world decision and patient selection, considering that a multivessel disease is still an absolute indication for CABG. Despite the initial intention, complete revascularization could be performed in 90.5% of patients. The reasons for revascularization failure (9.5% of patients) were procedural complications, such as 3.6% side-branch occlusion, vessel dissection and/or closure, a nonsatisfactory result of PCI (0.4%), or nontreatment of a significant stenosis (5.5%) due to the discovery of poor anatomical location of the lesion during PCI. On the one hand, the high rate of complete revascularization mirrors on one hand the correct choice of patients in accordance with the inclusion criteria, and on the other hand, the current real-world situation, with an almost 10% failure of complete revascularization in multivessel disease. Incomplete revascularization predicted mortality and the combined end point of death or myocardial infarction with high certainty. Bearing in mind that incomplete revascularization has been reported as a significant predictor for death both in other PCI and CABG studies [39,40], the AUTAX registry calls attention to the intention to treat all significant lesions when and where possible. A relatively short time interval for staging procedures may also be suggested, as incomplete revascularization resulted in significantly higher rate of AMI and/or death in the in-hospital phase.
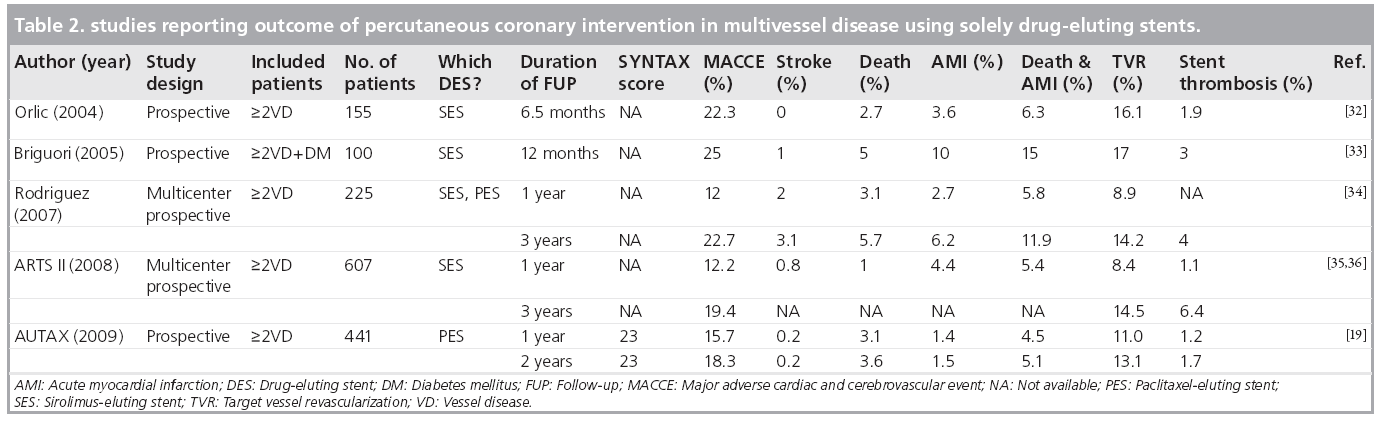
The 2‑year MACCE rate was relatively low in the AUTAX registry, compared with other registries (Table 2). The rate of routine and clinically driven control angiography was 78% at the 6‑month follow-up. Low rates of stent thrombosis or myocardial infarction were also recorded, suggesting the possible preventive role of control angiography in multivessel coronary artery disease, even if the oculo–stenotic reflex triggers repeat revascularization in otherwise asymptomatic patients. However, this hypothesis has been confirmed by the data of previously published registries on patients with higher rates of AMI and death, where the post-stenting control angiography rate was lower [41].
The SYNTAX score is the first attempt to combine more available scoring systems with a very good success rate, identifying patients for either PCI or CABG with de novo lesions. It is clear that the diversity of the individual coronary morphology, a priori, does not allow a perfect scoring system with a predictive role for MACCE either after PCI or CABG. Compared with other studies, even though the number of patients included is relatively small, the AUTAX registry provided important information for the further improvement or precision of the scoring system, from which a case for PCI or CABG can be made with high confidence.
Future perspective
The optimal treatment for patients with multivessel coronary artery disease is still a subject of debate, which is expected to be solved with fairly designed, prospective, randomized data reflecting current practice. Development of new DES will further decrease stent thrombosis and restenosis. DES use could also overcome the increased rate of repeat revascularization in multivessel disease. Patients with LM disease and those with diabetes and three‑vessel disease are of particular interest. Among improved CABG techniques, the more frequent off-pump surgery and the use of more arterial grafts aim to increase success rates, preserve patency of grafts and prevent stroke. Combined SYNTAX score with patient and procedural predictors for restenosis and MACCE may better discriminate patients with the possibility to benefit more from CABG or PCI. Long-term cost analysis of CABG and PCI with DES will demonstrate the economic rationale of both treatment options.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ The considerable difference in coronary lesion anatomy treated by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) results in a biased comparisons of long-term outcomes of the two treatment arms, and is based mainly on retrospective data analysis or prospective registries, with only a limited number of prospective randomized trials. These trials have demonstrated superior long-term outcome in CABG compared with PCI with drug-eluting stents, recommending CABG as the gold-standard treatment for multivessel disease.
▪ The key features of the prospective registries on multivessel disease are the inclusion of ‘all comers’, not excluding patients with post- PCI or post-CABG lesions. However, one of the main points of divergence between the randomized trials and prospective registries is the fact that the prospective randomized trials aim to create new treatment modalities and guidelines, while registries are descriptive, calling attention to unrecognized phenomena. The Austrian Multivessel Taxus™ Stent (AUTAX) registry showed significant predictors of 2‑year major adverse cardiac and cerebrovascular events (MACCE), including age over 70 years and unstable angina/non-ST elevation myocardial infarction (UA/NSTEMI) at clinical presentation. Diabetes mellitus and previous PCI showed a borderline significance in predicting MACCE. Furthermore, UA/NSTEMI and incomplete revascularization proved to be significant variables for mortality.
▪ The Synergy Between Percutaneous Coronary Intervention With Taxus and Cardiac Surgery (SYNTAX) score is the first attempt to combine more available scoring systems with a good success for patient selection for PCI or CABG in patients with de novo lesions.▪ The AUTAX registry shows that post-PCI or post-CABG lesions should also be included in prospective randomized trials, as these anatomic features will dominate multivessel coronary procedures in the very near future. The AUTAX registry calls attention to the intention to treat all significant lesions when and where possible. The AUTAX registry suggests a possible preventive role of control angiography in multivessel coronary artery disease.
▪ Among other studies, the AUTAX registry revealed important information for the further improvement or precision of the lesion scoring system, from which a decision for PCI or CABG can be justified.
References
Papers of special note have been highlighted as:
▪ of interest
- Javaid A, Steinberg DH, Buch AN et al.: Outcomes of coronary artery bypass grafting versus percutaneous coronary intervention with drug-eluting stents for patients with multivessel coronary artery disease. Circulation 116, I-200–I-206 (2007).
- Kukreja N, Serruys PW, De Bruyne B et al.: Sirolimus-eluting stents, bare metal stents or coronary artery bypass grafting for patients with multivessel disease including involvement of the proximal left anterior descending artery: analysis of the Arterial Revascularization Therapies study part 2 (ARTS-II). Heart 95, 1061–1066 (2009).
- Yang JH, Gwon HC, Cho SJ et al.: Comparison of coronary artery bypass grafting with drug-eluting stent implantation for the treatment of multivessel coronary artery disease. Ann. Thorac. Surg. 85, 65–70 (2008).
- Yan Q, Changsheng M, Shaoping N et al.: Percutaneous treatment with drug-eluting stent vs bypass surgery in patients suffering from chronic stable angina with multivessel disease involving significant proximal stenosis in left anterior descending artery. Circ. J. 73, 1848–1855 (2009).
- Varani E, Balducelli M, Vecchi G, Aquilina M, Maresta A: Comparison of multiple drug-eluting stent percutaneous coronary intervention and surgical revascularization in patients with multivessel disease. J. Invasive. Cardiol. 19, 469–475 (2007).
- Tarantini G, Ramondo A, Napodano M et al.: PCI versus CABG for multivessel coronary disease in diabetics. Catheter Cardiovasc. Interv. 73, 50–58 (2009).
- Qiao Y, Ma C, Nie S et al.: Twelve-month clinical outcome of drug-eluting stents implantation or coronary artery bypass surgery for the treatment of diabetic patients with multivessel disease. Clin. Cardiol. 32, E24–E30 (2009).
- Park AW, Yun SC, Lee SW et al.: Long-term mortality after percutaneous coronary intervention with drug-eluting stent implantation versus coronary artery bypass surgery for the treatment of multivessel coronary artery disease. Circulation 117, 2079–2086 (2008).
- Serruys PW, Morice MC, Kappetein AP et al.: Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360, 961–972 (2009).
- Briguori C, Condorelli G, Airoldi F et al.: Comparison of coronary drug-eluting stents versus coronary artery bypass grafting in patients with diabetes mellitus. Am. J. Cardiol. 99, 779–784 (2007).
- Lee MS, Jamal F, Kedia G et al.: Comparison of bypass surgery with drug-eluting stents for diabetic patients with multivessel disease. 123, 34–42 (2007).
- Li Y, Zheng Z, Xu B et al.: Comparison of drug-eluting stents and coronary artery bypass surgery for the treatment of multivessel coronary disease. Three-year follow-up results from a single institution. Circulation 119, 2040–2050 (2009).
- Gulati R, Rihal CS, Gersh BJ: The SYNTAX trial – a perspective. Circ. Cardiovasc. Intervent. 2, 463–467 (2009).
- Hamada Y, Kawachi K, Yamamoto T et al.: Effect of coronary artery bypass grafting on native coronary artery stenosis. Comparison of internal thoracic artery and saphenous vein grafts. J. Cardiovasc. Surg. (Torino) 42, 159–164 (2001).
- Rastan AJ, Boudriot E, Falk V et al.: Frequency and pattern of de-novo three-vessel and left main coronary artery disease; insights from single center enrolment in the SYNTAX study. Eur. J. Cardiothoracic Surg. 34, 376–383 (2008).
- Eagle KA, Guyton RA, Davidoff R et al.: American College of Cardiology; American Heart Association, ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation 110, E340–E437 (2004).
- Hoffman SN, Tenbrook JA, Wolf MP et al.: A meta-analysis of randomized controlled trials comparing coronary artery bypass graft with percutaneous transluminal coronary angioplasty: one- to eight-year outcomes. J. Am. Coll. Cardiol. 41, 1293–1304 (2003).
- Kappetein AP, Dawkins KD, Mohr FW et al.: Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease: insights from the SYNTAX run-in phase. Eur. J. Cardiothorac. Surg. 4, 486–491 (2006).
- Gyöngyösi M, Christ G, Lang I et al.: 2-year results of the Austrian Multivessel TAXUS-Stent (AUTAX) registry. Beyond the SYNTAX study. JACC Cardiovasc. Interv. 2, 718–727 (2009).
- King SB 3rd, Smith SS Jr, Hirshfeld JW et al.: 2007 Focused Update of the ACC/ AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention. A Report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines. Circulation 117, 261–295 (2008).
- Sianos G, Morel MA, Kappetein AP et al.: The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroInterv. 1, 219–227 (2005).
- Mauri L, Hsieh W, Massaro JM et al.: Stent thrombosis in randomized clinical trials of drug-eluting stents. N. Engl. J. Med. 356, 1020–1029 (2007).
- Van Gaal WJ, Ponnuthurai FA, Selvanayagam J et al.: The SYNTAX score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int. J. Cardiol. 135, 60–65 (2009).
- Capodanno D, Capranzano P, Di Salvo ME et al.: Usefulness of syntax score to select patients with left main coronary artery disease to be treated with coronary artery bypass graft. JACC Cardiovasc. Interv. 2, 731–738 (2009).
- Birim Ö, van Gameren M, Bogers AJJC et al.: Complexity of coronary vasculature predicts outcome of surgery for left main disease. Ann. Thorac. Surg. 87, 1097–1105 (2009).
- Lemesle G, Bonello L, de Labriolle A et al.: Prognostic value of the syntax score in patients undergoing coronary artery bypass grafting for three-vessel coronary artery disease. Cath. Cardiovasc. Interv. 73, 612–617 (2009).
- Boodhwani M, Rubens FD, Wozny D et al.: Predictors of early neurocognitive deficits in low-risk patients undergoing on-pump coronary artery bypass surgery. Circulation 114(1 Suppl.), I461–I466 (2006).
- Costa MA, Carere RG, Lichtenstein SV et al.: Incidence, predictors, and significance of abnormal cardiac enzyme rise in patients treated with bypass surgery in the arterial revascularization therapies study (ARTS). Circulation 104, 2689–2693 (2001).
- Hillis GS, Zehr KJ, Williams AW et al.: Outcome of patients with low ejection fraction undergoing coronary artery bypass grafting: renal function and mortality after 3.8 years. Circulation 114(1 Suppl.), I414–I419 (2001).
- Brooks MM, Jones RH, Bach RG et al.; for the BARI Investigators: Predictors of mortality and mortality from cardiac causes in the bypass angioplasty revascularization investigation (BARI) randomized trial and registry. Circulation 101, 2682–2689 (2000).
- Wijns W: The AUTAX (Austrian Multivessel TAXUS™-stent) registry: another useful registry on stented angioplasty for multivessel disease? J. Am. Coll. Cardiol. Int. 2, 728–730 (2009).
- Orlic D, Bonizzoni E, Stankovic G et al.: Treatment of multivessel coronary artery disease with sirolimus-eluting stent implantation: immediate and mid-term results. J. Am. Coll. Cardiol. 43, 1154–1160 (2004).
- Briguori C, Colombo A, Airoldi F et al.: Sirolimus-eluting stent implantation in diabetic patients with multivessel coronary artery disease. Am. Heart J. 150, 807–813 (2005).
- Rodriguez AE, Maree AO, Mieres J: Late loss of early benefit from drug-eluting stents when compared with bare-metal stents and coronary artery bypass surgery: 3 years follow-up of the ERACI III registry. Eur. Heart J. 28, 2118–2125 (2007).
- Serruys PW, Ong ATL, Morice MC et al.: Arterial Revascularization Therapies Study part II – sirolimus-eluting stents for the treatment of patients with multivessel de novo coronary artery lesions. EuroInterv. 1, 147–156 (2005).
- Serruys PW, Daemen J, Morrice MC et al.: Three-year follow-up of the ARTS-II – sirolimus-eluting stents for the treatment of patients with multivessel coronary artery disease. EuroInterv. 3, 450–459 (2008).
- Hao H, Gabbiani G, Camenzind E et al.: Phenotypic modulation of intima and media smooth muscle cells in fatal cases of coronary artery lesions. Atheroscler. Thromb. Vasc. Biol. 26, 326–332 (2006).
- Farhan S, Hemetsberger R, Matiasek J et al.: Implantaiton of paclitaxel-eluting stent impairs the vascular compliance of arteries in porcine coronary stenting model. Atherosclerosis 202, 144–151 (2009).
- Hannan EL, Wu C, Walford G et al.: Drug-eluting stents vs. coronary-artery bypass grafting in multivessel coronary disease. N. Engl. J. Med. 358, 331–341 (2008).
- Alamanni F, Dainese L, Naliato M et al.: On- and off-pump coronary surgery and perioperative myocardial infarction: an issue between incomplete and extensive revascularization. Eur. J. Cardiothorac. Surg. 34, 118–126 (2008).
- Gyöngyösi M, Khorsand A, Sperker W et al.; on behalf of the Palmaz-Schatz, AVE, AMULET I, AMULET II and Carbo Stent Registry Groups: Short- and long-term clinical outcome after various stent implantation: overview of the results of uni- and multicenter stent registries. Catheter Cardiovasc. Interv. 62, 331–333 (2004).
▪ The SYNTAX study compared percutaneouss coronary intervention (PCI) and coronary artery bypass grafting (CABG) for treating patients with de novo three-vessel disease and/ or left main (3-VD/LM) coronary artery disease. Rates of major adverse cardiac and cardiovascular events at 12 months were significantly higher in the PCI group owing to an increased rate of repeat revasculariz-ation; as a result, the criterion for non-inferiority of PCI was not met. At 12 months, the rates of death and acute myocardial infarction were similar between the two groups. Stroke was significantly more likely to occur with CABG. The SYNTAX study concluded that CABG remains the standard of care for patients with 3-VD or LM coronary artery disease.
▪ A total of 694 patients with 3-VD or LM lesions were screened for participation in the SYNTAX trial. Of the patients, 271 had previous CABG and 232 previous PCI, so were not screened for SYNTAX. Of the 191 patients with de novo 3-VD or LM, 87 presented exclusion criteria (AMI or concomittant disease) for SYNTAX. Of the remaining patients, 13 refused to participate, ten presented with uncertain protocol adherence and six were already participating in other cardiovascular trials. A total of 67 patients were enrolled in the SYNTAX study, representing 9.7% of 3-VD or LM and 35.1% of all screened patients.
▪ Among other scoring systems such as the Gensini score, the American Heart Association/American College of Cardiology and Society for Cardiovascular Angiography and Intervention classifications, the SYNTAX score had the highest predictive value for prediction of periprocedural infarction after multivessel PCI.
▪ Consecutive patients with three 3-VD coronary artery disease were divided into tertiles according to the SYNTAX score. Unlike for PCI, the SYNTAX score proved to be of poor prognostic value for severe cardiovascular events in patients undergoing CABG. The study suggested that other risk scores should be used to predict the outcome of this population.