Research Article - Clinical Investigation (2020) Volume 10, Issue 3
The knowledge of oral hygiene and oral hygiene habits during pregnancy and puerperium
Submitted: 21 April 2020; Accepted: 30 April 2020; Published online: 28 April 2020
Abstract
OBJECTIVES. We wanted to explore the knowledge and attitudes of pregnant women and women after giving birth to oral health. Likewise, we wanted to determine whether there was any awareness of oral hygiene during pregnancy in the aforementioned population. Our aim was to establish the correlation between oral hygiene habits in relation to age, level of education and place of residence (urban / rural) and to determine the importance of the role of experts in further education of the patient. STUDY DESIGN. A cross-sectional study. PATIENTS AND METHODS. The subjects were patients admitted to the department of maternal and puerpera in the maternity ward of the General Hospital Zabok and Croatian veterans in the period from 1 December 2016 till 15 February 2017. Data for statistical analysis were obtained on the basis of an anonymous questionnaire of 15 questions. RESULTS. Nearly half of pregnant women and women after delivery (49%) believe that oral hygiene does not affect the outcome of pregnancy. In Planned Parenthood pregnancy 70% of women with the lowest levels of education are not going to control dental examinations. Over 90% of highly educated respondents used additional oral hygiene products, while only 20% of women with low levels of education used additional products. The results showed that 71% of women thought they had not received enough oral health information from their doctor. Also, in 60% of respondents, primary data on oral hygiene and health were not received by health professionals but from other sources. CONCLUSION. The obtained data show that almost half of the respondents did not develop the habit of awareness of the need for oral hygiene. The prevalence of monitoring the level of education but are weaker indicators correlate with low skill levels. The emphasis of the modern approach to the prevention of, and given that over half of the surveyed women does not the necessary knowledge of oral health opens space for continuing education and the promotion of information programs by the health system.
Keywords
Caries • Gingivitis • Oral health • Oral knowledge • Pregnancy
Introduction
In spite of the great efforts in preserving oral health, one of the most common oral diseases, dental caries, still occupies the first place among the most extensive form of diseases, both in Croatia and in the whole world. If we take the fact that the good health of the population is one of the main objectives of the State policy of social welfare, it is more than obvious that the prevention of caries and periodontal disease should be a priority. One of the key measures in promoting oral health is a measure of informing and educating the population. Oral health is an integral part of general health and an important factor in the overall quality of life. Only a healthy cavity provides nutrition, speech, and social contact without any difficulty. Optimal maternal oral hygiene in an induced perinatal period can reduce the number of oral bacteria and inflammatory mediators who disseminate with the blood through the placental on embryo or fetus [1-6].
Caries is a chronic infectious disease with a lack of tooth substance. At the same time, it is a place of entry of the infection in the pulp of teeth, periodontal structures, and ultimately in the whole organism [7,8]. Periodontal disease is one of the most common chronic disorders of infective origin. According to some authors, the prevalence in adults varies by up to 60%, depending on the diagnostic criteria. The cause is dental plaque and bacteria in plaque [9]. During pregnancy, the risk of caries is increased. One of the risk factors is the presence of gastric acid in the oral cavity, as a consequence of vomiting that occurs in earlier stages of pregnancy while in the later stages of pregnancy occurs as a result of esophageal reflux due to the increased intraabdominal pressure. Although pregnancy is a physiological status, it is also often the first time that the body experiences a state of “metabolic stress”. However, apart from physiological changes, there is a possibility of the occurrence of pathological conditions induced by altered hormonal status during pregnancy. Progesterone level during pregnancy reaches 10 times and estrogen 30 times higher value than in the normal reproductive cycle [9-12].
In order to set up the foundations of good oral health, we must maintain the oral structure healthy and motivate the patients to cooperate and encourage them for the use of dental services. The aim of control examinations is individually-focused education, making and correcting oral-hygiene habits, the determination of the index of plaque, ambulance analysis of the composition of saliva, and caries risk assessment. Pregnancy is a specific moment when most women are motivated to adopt healthy behaviors, eager for knowledge and insights. The education of patients involves providing information and guidelines for maintaining oral health. It is focused on the patient, but also on the other members of the dental team, the gynecologic infirmary and patronage service. The relationship of all stakeholders should be based on mutual trust. Education is carried out through all available channels: a personal conversation with the patient, educational brochures, online forums, social networks, and pregnancy courses. In order to have results, education should be high quality vertically and horizontally designed but also available and individually adjusted [4-7].
Materials and Methods
The subjects
The survey included a total of 133 women who were received in the General Hospital Zabok and Croatian Veterans hospital in the period from 1 December 2016 till 15 February 2017. The subjects are the patient admitted to the department of maternal and puerpera in the maternity ward of the General Hospital Zabok and Croatian Veterans hospital due to pathological changes in pregnancy and/or finishing the birth at the time of the survey.
Methods
The measuring instrument is a questionnaire constructed for the purpose of research on oral health, composed of fifteen questions about existing knowledge and attitudes about oral hygiene and oral hygiene habits of pregnant women and puerpera. The first part of the questionnaire (of 1-4 issues) includes questions about the age, educational status, and place of residence. The second part of the questionnaire refers to information about oral health during pregnancy and puerperium.
The way of testing - research was conducted on the anonymous survey. The Ethics Committee of Zabok General Hospital and Croatian Veterans hospital and the Ethics Commission of Faculty of Dental Medicine and Health in Osijek, the Josip Juraj Strossmayer University of Osijek, have approved the implementation of the research.
Statistical methods
Categorical data is represented by absolute and relative frequencies. Numerical data are described with arithmetic mean and standard deviation in the case of a distribution that follows the normal, and in other cases, with median and the limits of interquarterly range. Comparison analysis between categorical variables was tested with the Chi-square Test, and if necessary with Fisher’s Exact Test. The differences of normally distributed numerical variables between two independent groups have been tested with Student’s T-Test. All P values were two-sided and the significance level was set at 0.05. For statistical analysis was used MedCalc statistical software (version 15.11.4, Ostend, Belgium).
Results
In this study, there was a total of 133 pregnant women in the age of 29.5 ± 5.7 (arithmetic mean ± SD). The youngest woman was 17 and the oldest woman was 41 years old. Most of them (60.2%) had high school education (p<0.001, Chi-square Test) and were from the city or suburb (60.9%, p=0.07, Chi-square Test). To most women, this was not the first pregnancy (85.5%, p < 0.001, Chi-square Test).
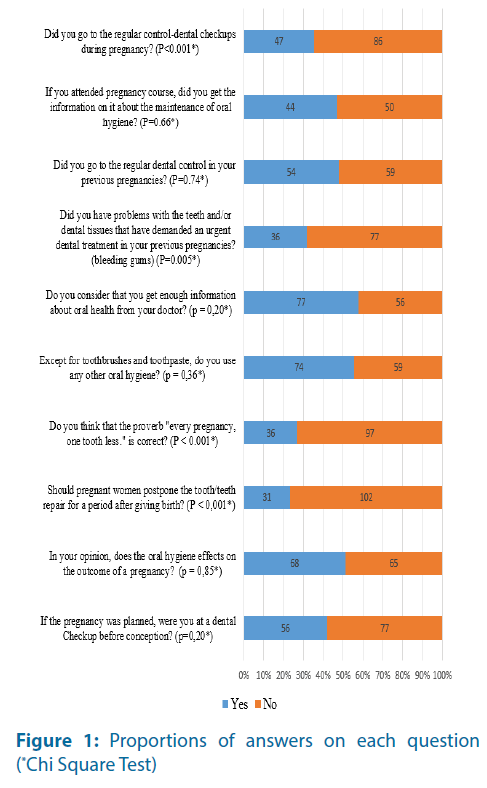
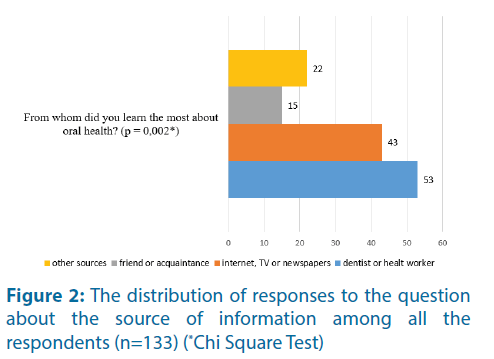
The distribution of the responses to individual issues is shown graphically (Figures 1 and 2).
Figure 2: The distribution of responses to the question about the source of information among all the respondents (n=133) (*Chi Square Test)
Significantly more subjects considered a proverb “every pregnancy, one toothless” being true, while significantly more subjects considered that one should not put off repairing teeth after giving birth (Figure 1).
A significant majority of the respondents said that in previous pregnancies had no problems with their teeth or tissues that have demanded an urgent dental treatment (Figure 1).
An equal number of the subject said that have, and that have not received information about the oral hygiene on pregnancy courses (Figure 1).
A total of 74 of the subject (55.6%) declared that they used something else than a toothpaste. Predominantly they used dental floss, 32 of them (43.2%), while mouthwash is used by 24 (32.4%) and both by 18 (24.3%) subjects. The significantly small number of subjects doesn’t go to the regular controldental checkups during the pregnancy (Figure 1).
It is a large and statistically significant difference in the number of subjects that used, as a source of information on oral health during pregnancy, the internet, TV, newspaper, friend, or health professional (Figure 2).
The average birth weight of the child for the subjects that were given birth (n=105) is 3460 ± 441 grams (the arithmetic mean ± standard deviation) in the range from 2017 to 4560 grams. There was no significant association between the birth weight of the child and bad oral-hygienic habits and knowledge. Only one of the respondents who gave birth (0.95%), was born before the term and it was not possible to analyze the association of gestation and poor oral hygiene habits and knowledge (Table 1).
| Questions | Aritmetic mean (SD) | P* | |
|---|---|---|---|
| Yes | No | ||
| The age of the respondents | |||
| Control dental examination? | 30.4 (5.2) | 28.8 (6.0) | 0.11 |
| Regular dental examinations in previous pregnancies? | 30.1 (5.0) | 29.8 (5.9) | 0.77 |
| Does oral hygiene affect the outcome of pregnancy? | 29.3 (5.6) | 29.6 (5.8) | 0.78 |
| Problems with teeth for emergency dental treatment? | 29.7 (5.6) | 30.0 (5.4) | 0.81 |
| Should you delay the repair teeth? | 29.6 (6.5) | 29.4 (5.5) | 0.90 |
| If it's true the proverb "every pregnancy, one tooth less"? | 29.1 (6.4) | 29.5 (5.4) | 0.69 |
| If you use other means of oral hygiene apart from toothbrushes and toothpaste? | 30.5 (5.0) | 28.2 (6.2) | 0.02 |
| The child's birth weight in grams | |||
| Are you going to the control of the regular dental checkups? | 3366 (358) | 3450 (493) | 0.77 |
| Are you in previous pregnancies went to the regular dental checkups? | 3458 (433) | 3513 (401) | 0.54 |
| Does oral hygiene on the outcome of a pregnancy? | 3445 (341) | 3479 (540) | 0.78 |
| Have you had problems with your teeth for emergency dental treatment? | 3505 (357) | 3486 (440) | 0.85 |
| Should you delay the repair teeth? | 3528 (450) | 3441 (439) | 0.40 |
| If it's true the proverb "every pregnancy, one tooth less"? | 3360 (368) | 3501 (464) | 0.14 |
| If you use other means of oral hygiene apart from toothbrushes and toothpaste? | 3466 (410) | 3454 (487) | 0.89 |
Table 1. Relation between oral-hygiene habits with mothers’ age and children’s weigh
There is a significant connection between the degree of professional qualifications with the opinion that oral hygiene can affect the outcome of the pregnancy and with the use of additional oral hygiene products, besides toothbrushes and toothpaste (Table 2). A higher level of education assumes a greater awareness of the potential impact of oral hygiene on the outcome of pregnancy. Also, a higher degree of education means frequent and significant use of additional oral hygiene products.
| Question | Number (%) of | P | Number (%) of | P | ||||
|---|---|---|---|---|---|---|---|---|
| Prims | Second | BA | MA/PhD | Village | City | |||
| Did you go to the regular control-dental checkups during pregnancy? | ||||||||
| Yes | 3 (30.0) | 31 (38.8) | 11 (50.0) | 11 (52.4) | 0.49* | 23 (44.2) | 33 (40.7) | 0.69 * |
| No | 7 (70.0) | 49 (61.3) | 11 (50.0) | 10 (47.6) | 29 (55.8) | 48 (59.3) | ||
| Did you go to the regular dental control in your previous pregnancies? | ||||||||
| I do | 4 (40.0) | 32 (48.5) | 11 (52.4) | 7 (43.8) | 0.91* | 24 (49.0) | 30 (46.9) | 0.82* |
| No | 6 (60.0) | 34 (51.5) | 10 (47.6) | 9 (56.3) | 25 (51.0) | 34 (53.1) | ||
| Does the oral hygiene effects on the outcome of a pregnancy? | ||||||||
| I do | 3 (30.0) | 38 (47.5) | 10 (45.5) | 17 (81.0) | 0.02* | 26 (50.0) | 42 (51.9) | 0.84* |
| No | 7 (70.0) | 42 (52.5) | 12 (54.5) | 4 (19.0) | 26 (50.0) | 39 (48.1) | ||
| Have you had problems with your teeth for emergency dental treatment? | ||||||||
| I do | 6 (60.0) | 17 (25.8) | 7 (33.3) | 5 (31.3) | 0.14† | 13 (26.5) | 23 (35.4) | 0.31* |
| No | 4 (40.0) | 49 (74.2) | 14 (66.7) | 11 (68.8) | 36 (73.5) | 42 (64.6) | ||
| Should you delay the repair teeth? | ||||||||
| I do | 4 (40.0) | 21 (26.3) | 3 (13.6) | 3 (14.3) | 0.28† | 13 (25.0) | 18 (22.2) | 0.71* |
| No | 6 (60.0) | 59 (73.8) | 19 (86.4) | 18 (85.7) | 39 (75.0) | 63 (77.8) | ||
| Do you think that the proverb "every pregnancy, one tooth less." is correct? | ||||||||
| I do | 3 (30.0) | 24 (30.0) | 5 (22.7) | 4 (19.0) | 0.73* | 13 (25.0) | 23 (28.4) | 0.67* |
| No | 7 (70.0) | 56 (70.0) | 17 (77.3) | 17 (81.0) | 39 (75.0) | 58 (71.6) | ||
| Except for toothbrushes and toothpaste, do you use any other oral hygiene? | ||||||||
| I do | 2 (20.0) | 38 (47.5) | 15 (68.2) | 19 (90.5) | <0.001* | 20 (38.5) | 54 (66.7) | 0.001* |
| No | 8 (80.0) | 42 (52.5) | 7 (31.8) | 2 (9.5) | 32 (61.5) | 27 (33.3) | ||
†Fisher's Exact Test
Table 2. Correlation between oral-hygiene habits in relation to the degree and in relation to a dwelling place
The subjects that live in the city or in the village considerably more often use additional oral hygiene products (Table 2).
Slightly more than half (57.9%) of them believe that have received enough information about oral health from their doctor. In the table, there is the result of the analysis of the connection according to the examined demographic parameters (Table 3).
| Compared parameters | Number (%) of examinees | P | |
|---|---|---|---|
| That received enough information | Didn’t received enough information | ||
| School education subject | |||
| Elementary school | 7 (9.1) | 3 (5.4) | 0.42† |
| Secondary school | 48 (62.3) | 32 (57.1) | |
| BA | 9 (11.7) | 13 (23.2) | |
| MA | 10 (13.0) | 5 (8.9) | |
| PhD | 3 (3.9) | 3 (5.4) | |
| The place of residence of the | |||
| Village | 31 (40.3) | 21 (37.5) | 0.75* |
| Town or city | 46 (59.7) | 35 (62.5) | |
| Do you think that is the correct proverb "every pregnancy, one tooth less"? | |||
| I do | 15 (19.5) | 21 (37.5) | 0.02* |
| No | 62 (80.5) | 35 (62.5) | |
| From whom did you learn the most about oral health? | |||
| Your dentist or health professional | 45 (58.4) | 8 (14.3) | <0.001* |
| Internet, TV or newspapers | 15 (19.5) | 28 (50.0) | |
| Friend or acquaintance | 7 (9.1) | 8 (14.3) | |
| Other sources of | 10 (13.0) | 12 (21.4) | |
| Should pregnant women postpone repair teeth? | |||
| Yes | 13 (16.9) | 18 (32.1) | 0.04* |
| No | 64 (83.1) | 38 (67.9) | |
| In your opinion does oral hygiene on the outcome of pregnancy? | |||
| Yes | 45 (58.4) | 22 (39.3) | 0.03* |
| No | 32 (41.6) | 34 (60.7) | |
| Are you going to the regular control-dental checkups during pregnancy? | |||
| Regularly | 37 (48.1) | 10 (17.9) | <0.001* |
| If necessary, | 35 (45.5) | 34 (60.7) | |
| Not at all | 5 (6.5) | 12 (21.4) | |
| A total of | 77 (100.0) | 56 (100.0) | |
†Fisher’s Exact Test
Table 3. Comparing demographic parameters, knowledge, and attitude with a question regarding receiving enough information about oral health
Subjects who feel that they have received enough oral health information from their physician significantly less believe in the popular proverb “Every pregnancy, one toothless”. The most commonly received information from a dentist or a healthcare professional, would not delay the tooth repair during pregnancy, at a higher percentage know that oral hygiene can affect the outcome of the pregnancy and at a significantly lower percentage avoid regular control-checkups during pregnancy (Table 3).
Discussion
Most of the surveyed women have high professional qualifications, just as many of them are from the urban environment, and to most of them, this is not the first pregnancy. Although pregnancy is not the cause of caries, tooth decay is easier to develop in pregnancy. In Croatia, there is a saying that says that in each pregnancy mother loses one tooth, which was explained with the increased need for calcium due to the construction of the skeletal system of the baby. It is true that after the fifth month of the growing, the need for calcium in teeth is increased, but in teeth, it is in a stable compound, so once embedded, it can no longer be digested from the tooth except by the action of bacteria and decay. In other words, an embryo or a fetus could not “draw” calcium from tooth [13].
Most of the women surveyed say they consider that repairing teeth should not be put off and do not believe that will lose a tooth in a pregnancy. It is still a large percentage, a quarter of them that means that. Especially bad is an indicator that nearly half the women consider that oral hygiene does not affect the outcome of the pregnancy.
During pregnancy twenty dairies and four permanent molars are formed [7]. In conclusion, pregnancy is a time for the prevention of the health of teeth offspring and is the best time to teach pregnant women to teach about basic preventive protective dental-health measures in an infant [5].
Most of the subjects in previous pregnancies had no problems with teeth or tissues such that they require urgent dental treatment, but also don’t have a habit of a preventive dental examination.
While the world dental medicine Federation- FDI (Federation Dentaire Internationale) is just adopting a strategy of action up to the year 2020 on strengthening capacity and efficiency and the availability of the health system, the Republic of Croatia with almost 2000 teams has a remarkably widespread network of dental protection of the population. However, we cannot boast good statistical indicators of oral health of the nation. Moreover, only Bulgaria has worse epidemiological results from all the Member States of the European Union [3].
Although the inflammation of the gums during pregnancy is the frequent state, if oral hygiene is good and there is no food deposits and plaque, gingivitis will not develop because the only action of hormones is not enough to develop inflammation [12]. Regular check-up and professional teeth cleaning will reduce and slow down the progression of initial carious lesions, while those large lesions, which can worsen and cause other complications, need to be restored as soon as possible. In case of a need for more complex dental procedures that must be performed prior to delivery, the doctor of dental medicine in consultation with the gynecologist will choose the best way and time of treatment, which will not be harmful to a pregnant woman or even fetus [5]. Accordingly, pregnant women should be educated that oral health effects on general health and that delaying treatment can get to more complex problems.
Research conducted on knowledge and attitudes about oral hygiene in Spain in 201 on a sample of 337 pregnant women, talks about the significant correlation between the high level of self-assessment of oral health in pregnant women and low levels of dental caries and low periodontal index [14].
In this study, more than half of the women did not go to the examination before pregnancy, even though it was planned, nor went on regular controldental checkups in previous pregnancies. Only onethird of the subject went to the regular control-dental checkups during pregnancy, while others didn’t go at all, or they went only if they needed to. Almost half of the respondents for oral hygiene used only the toothbrush and toothpaste. The remaining surveyed women most commonly used dental floss, mouthwash, or both.
In neighboring Hungary, the results are similar. In a survey conducted in 2011 on a sample of 275 pregnant women, even 70% of them declared that have visited the dentist during pregnancy, but only one-third used additional oral hygiene products [15].
Prematurely children constitute a significant public health problem because birth weight is one of the most important factors in the growth, development, and survival of the infants [2].
In a study conducted on a sample of 124 pregnant women, it has been shown that the premature childbirth children with small birth weight are seven times more common in pregnant women with periodontal diseases it is a bigger risk factor than smoking, consumption of alcohol and the age of the mother [13]. Measuring the levels of C-reactive protein(as a measure of the degree of systemic inflammation) in the blood is also interesting. According to one survey, in periodontal disease the level of CRP is increased, and after periodontal therapy decreased [9,10]. That is exactly what can be interpreted as a link between periodontal disease and systemic health [2,16].
The other or additional oral hygiene products are more used by elderly pregnant women where a statistically significant difference was found. Nearly one-third of primary and secondary educated women consider that in every pregnancy they will lose one tooth.
A significant connection is found between the degree of professional qualifications with the opinion that oral hygiene can affect the outcome of the pregnancy and with the use of additional oral hygiene products other than toothbrushes and toothpaste. In the already mentioned study in Hungary, a statistically significant correlation between the level of education and the use of dental floss was found [15]. According to these results, we can conclude that a higher level of education correlates with a higher awareness of oral hygiene.
This research showed that the subjects from the urban environment significantly more often use additional oral hygiene products.
Slightly less than half of the surveyed women believe that have not received enough information about oral health from their doctor. The remaining women statistically significantly less believe in the folk proverb “every pregnancy, one toothless” and they would not postpone repairing teeth during pregnancy.
However, more significant is the fact that 50 of 94 subjects, which have attended pregnancy courses, responded that they didn’t get information on oral health there.
Primary information about oral health needs to be given by a dentist or other health professional. On the trail of this, there is a devastating fact that only 53 of that kind of information is received from a health professional. The reasons could be found in systematic and continuous negligence of preventive programs and thus imposes the need for updating the guidelines and practices of health care.
In the empirical research conducted in Poland in 2015, from 1380 pregnant women only 40% of them provide the right answers to questions about dental problems. More than 70% of pregnant women developed gingivitis or periodontitis, and Poland is trying to implement a European principle of treatment of pregnant women as a vulnerable group of dental patients [17].
In order to get comparable indicators with an average “old” EU Member States, you need a symbiosis of primary, secondary and tertiary levels of the health system. Specialists for preventive dental medicine are needed. However, where they exist they do a polyvalent job and the system does not recognize or does not use their knowledge [3].
Pregnancy course, where pregnant women should educate themselves about oral health, is attended by 94 of 133 subjects. In conclusion, over a quarter of the women did not even have a chance to get the complete information oriented towards reducing the fear and the building of positive attitudes.
Similarly, research conducted in Poland in 2016, shows how knowledge of future parents starts on pregnancy courses is not satisfactory, however at the same time most of them are ready to take part in organized lectures on a given topic [18].
Oral health is to be maintained throughout the entire life span of women, and also during pregnancy. In dental medicine, the protection of pregnant women, according to experts of the World Health Organization for medical priorities comes immediately after protecting children of school and preschool-age children, old people, and chronic patients. If we know how most oral diseases can be prevented, it is obvious that the system we have now is not preventive. If we are aware of the fact that the cost of curative is greater than prevention, it is obvious that a change is necessary. The ability to reply to oral health threats requires a system of rapid detection, quick reactions, adequate responses, and communication about the threats. A precondition for the functioning of the system is the organizational network and corresponding action plans [2-6].
The state of oral health in the Republic of Croatia indicates an infinite scale of damage that has occurred by eliminating the network of specialist children’s and preventive dental medicine, and whose results are twenty years ago pointed to the improvement of the same. Today, the Government is trying to implement the existing specialists to participate in the planning, implementation, and control of prevention programs. In conclusion, the Government of the Republic of Croatia in early 2015 has proposed the adoption of a document with the name: a strategic plan to promote and protect the oral health for the period from 2012 to 2020 [4].
Comparison of knowledge and behavior of children and parents in the maintenance of oral hygiene, in a survey conducted in Croatia in 2016, it was found that children whose parents regularly maintain oral hygiene have better oral-hygienic habits compared to children whose parents do not wash their teeth regularly [19]. As well as all other health habits, oral hygiene is adopted in an environment of family, and the future mother is the one who should teach her child the correct adoption of hygienic habits [5].
Thus we raise awareness of oral health and we encourage and develop the principle of selfresponsibility, and it is a long-lasting and continuous process of the multidisciplinary approach [3].
The possible lack of this research is the lack of strengths to evaluate the causal relationship. One of the main conclusions of the work is repeated education and accordingly, one of the guidelines of some the following research could be a comparison between “educated” and “not educated” pregnant women and puerpera with specific risk factors or the connection between oral hygiene and systematic health.
In spite of this, the visible data show us that almost half of the patients haven’t developed habits nor awareness of oral hygiene. The prevalence follows the degree of education levels so the worse indicators are correlated with a lower education degree. The emphasis of the contemporary approach is prevention, and according to the fact that over half of surveyed women don’t have the necessary knowledge about oral health, opens a space for continuous education and promoting the informative program by the health system.
Conclusion
The obtained data show that almost half of the respondents did not develop the habit of awareness of the need for oral hygiene. The prevalence of monitoring the level of education but are weaker indicators correlate with low skill levels. The emphasis of the modern approach to the prevention of, and given that over half of the surveyed women do not the necessary knowledge of oral health opens space for continuing education and the promotion of information programs by the health system.
References
- Petričević N, Čelebić A, Baučić Božić M, et al. Oral health and quality of life: The foundation of the modern approach. Medix 75: 62-66 (2008).
- Terlević Dabić D. Connection of oral and general health. Dent Med Her 24: 16-18 (2016).
- Ministry of Health of the Republic of Croatia. Proposal of strategic plan for the promotion and protection of oral health, (2017).
- Koch G, Poulsen S. Pedodonti clinical approach. Publishing Slap (2004).
- Vidović N. Protection of oral health in pregnancy. Mojstomatolog (2014).
- Committee Opinion No. 569: Oral health care during pregnancy and through the lifespan. Obstet Gynecol 122: 417-422 (2013).
- Vodanović M, Brkić H, Savić Pavičin I. Basics of dentistry. Jastrebarsko: Naklada Slap (2015).
- Juhas I. Knowledge of oral health and health behavior of parents and children of school age. Bjelovar High School of Technical School, (2016).
- Pezelj Ribarić S. Oral health condition for general health. Univ Rijeka (2013).
- Bukvić L. Changes in oral mucous membranes and skin during pregnancy. Univ Zagreb (2015).
- Bullon P, Jaramillo R, Santos Garcia R, et al. Relation of periodontitis and metabolic syndrome with gestational glucoseal metabolism disorder. JPeriodontol 85: e1-8 (2014).
- Lindhe J, Karring TH, Lang NP. Clinical periodontal and dental implantology. Zagreb: Publishing Institute Globus (2004).
- Croatian chamber of dental medicine. Pregnancy (2015).
- Martínez-Beneyto Y, Vera-Delgado MV, Pérez L, Maurandi A. Self-reported oral health and hygiene habits, dental decay, and periodontal condition among pregnant European women. Int J Gynaecol Obstet 114: 18-22 (2011).
- Battancs E, Gorzó I, Pál A, et al. Pregnant women's oral hygiene knowledge and habits after the second millennium in South-East Hungary. Fogorv Sz 104: 75-79 (2011).
- Brekalo Pršo I, Kuiš D, Prpić J, et al. Determination of inflammatory mediators PGE2 and TXB2 from gingicular sulcular fluid in patients with chronic periodontitis. Med Flum 52: 257-261 (2016).
- Gaszyńska E, Klepacz-Szewczyk J, Trafalska E, et al. Dental awareness and oral health of pregnant women in Poland. Int J Occup Med Environ Health 28: 603-611 (2015).
- Wapniarska K, Buła K, Hilt A. Parent's pro-health awareness concerning oral health of their children in the light of survey research. Przegl Epidemiol 70: 59-63 (2016).
- Beljan M, Puhatić Z, Žulec M, et al. Knowledge of oral health and health behavior of parents and children of school age. Acta Med Croatica 70: 165-171 (2016).