Research Article - Interventional Cardiology (2023) Volume 15, Issue 4
The need for detailed institutional case analysis in assessing thirty-day unplanned readmission rate after Percutaneous Coronary Intervention (PCI): A quality assurance study
- Corresponding Author:
- Simon W. Rabkin
Division of Cardiology, Vancouver Hospital, Vancouver, Canada,
E-mail: simon.rabkin@ubc.ca
Received date: 07-Jun-2023, Manuscript No. FMIC-23-101727; Editor assigned: 09-Jun-2023, PreQC No. FMIC-23-101727(PQ); Reviewed date: 26-Jun-2023, QC No. FMIC-23-101727; Revised date: 03-Jul-2023, Manuscript No. FMIC-23-101727(R); Published date: 11-Jul-2023, DOI: 10.37532/1755- 5310.2023.15(4).742
Abstract
Background: Thirty-day unplanned readmission following PCI is recognized as an important quality metric because it is associated with poor outcomes. A national health information data bank (Canadian Institute of Health Information (CIHI)) reported an overall mean risk-adjusted 30-day all-cause unplanned readmission rate for PCI of 7.2%. We sought to compare this national metrics with a detailed analysis of local institutional data. Methods: A retrospective study of 30-day readmissions following PCI at Vancouver General Hospital during a three-year period from April 2015 to July 2018 to coincide with the CIHI report. Inclusion criteria were patients readmitted to any one of 5 hospitals within the region-Vancouver Coastal Health Authority (VCHA) or 12 hospitals within the adjacent Fraser Health Authority (FHA). Planned staged PCI procedures were excluded. The proportion of VCHA readmissions potentially related to poor PCI outcomes, angina pectoris or arrhythmia were determined. Results: There were 4,478 patients with PCI, of who had a 108 unplanned hospital readmission to VCHA and 50 to FHA, for a cumulative 3.5% readmission rate across the two largest health authorities in the province. Among the VCHA readmissions, a minority 21% (23 cases) were related to unstable angina/myocardial ischemia or arrhythmias. The majority of those cases had PCI on an urgent basis with drug-eluting stents. Conclusion: Thirty-day unplanned readmission rate after discharge from PCI at our tertiary hospital was low. These data underscore the importance of detailed case analysis to define true readmission rates, and questions the use of readmission rates as a sole metric of quality of care independent of detailed case review.
Keywords
Percutaneous coronary intervention • Hospital readmission • Quality assurance
Introduction
Percutaneous Coronary Intervention (PCI) is one of the most common revascularization modalities for the treatment of coronary artery disease [1,2]. Thirty-day unplanned readmission following PCI is recognized as an important quality metric in assessing PCI. Early readmission is associated with an increased risk of adverse events, poor outcomes, and healthcare costs [3,4]. Given the increasing number of patients who undergo PCI, reducing readmissions has become a priority for hospital systems, and strategies are now targeted to improve this metric [5,6].
Large data bases assess the quality of National health care based on computerized collection of hospital data. The Canadian Institute of Health Information (CIHI) has reported quality indicators for PCI across national centers [7]. These results from the CIHI administrative databases are updated annually by each Canadian cardiac care center. In 2018, the reported national mean rate for risk adjusted 30-day all-cause unplanned readmission after PCI was 7.2%, with an associated in hospital mortality of 2.2% [8]. Although Canada’s overall readmission rate has remained relatively stable over a three-year period, other data demonstrate that there is significant variability in readmission rates after PCI across hospitals [9]. Patient characteristics and comorbidities, procedural-related factors, as well as regional or geographic considerations may impact the inter-hospital comparability of results. Although CIHI takes this into consideration to provide risk-adjusted outcomes, there are potential limitations to the analysis, as studies have demonstrated differences in the availability of recording and the potential for inaccuracies in registry data and administrative databases [10,11]. Furthermore, it has been suggested that readmission data is not a good metric of procedural complication rates or other PCI quality measures. Detailed analysis using a quality assurance approach can provide a method to monitor clinical performance and develop strategies for improvement on an institutional level [12].
Understanding unplanned PCI readmissions has larger implications on overall health economics, in addition to assessing patient outcomes [13,14]. Unplanned PCI readmissions are associated with higher cumulative healthcare costs. For example, in a large multi-center analysis in the United States of America, 30-day PCI readmissions incurred 3% higher costs for the index hospitalization and 45% higher cumulative 30-day costs, after the sample was adjusted for differences in demographic, clinical, and hospital characteristics. Although such data suggest a substantial financial impact of PCI, it is important to understand the contextual factors of the causes and predictors of these readmissions to identify downstream implications of PCI on healthcare economics.
Recognizing the need to cross-validate administrative databases with in-depth case analysis [15], and the relative paucity of published data from individual hospital sites within the national database, we defined a clear attainable quality assurance metric for study. The objective was to evaluate the rate of 30-day unplanned readmissions following PCI after discharge from one of the largest hospitals in Canada, and to determine the proportion related to a poor PCI outcome, namely angina pectoris or arrhythmia. This was achieved by performing a detailed retrospective chart review of the administrative database to characterize the patient presentations and their clinical course during those readmissions.
Materials and Methods
Study design and patient selection
The database of Vancouver General Hospital (VGH) was queried by the Information Management Information Systems (IMIS) Department, for coronary angiogram cases that underwent PCI during the period of April 1, 2015 to July 26, 2018. The timeframe was selected for ease of computer access, because it corresponded to financial reporting quarters. Importantly, it encompasses the timeframe of the CIHI report. All elective and non-elective cases were assessed as to whether they were readmitted to hospital within 30-days of the procedure or hospital discharge, respectively. All patients who subsequently presented to a tertiary or affiliated community hospital within the Vancouver Coastal Health Authority (VCHA) or Fraser Health Authority (FHA) were eligible for inclusion. Planned staged PCI procedures were excluded in the analysis.
Vancouver Coastal Health and Fraser Health are both publicly funded regional healthcare authorities in British Columbia and deliver a wide range of health services to the province. The VCHA encompasses parts of Greater Vancouver and the Coast Garibaldi areas [16]. The major VCHA hospitals included in this study are VGH, St. Paul’s Hospital, Lion’s Gate Hospital, Richmond Hospital, and the University of British Columbia Hospital. Fraser Health is the province’s largest health authority and has the second largest cardiac capability after the VCHA [17]. It includes 12 acute-care hospitals, including 3 regional and 9 community hospitals. These FHA hospitals are Abbotsford Regional Hospital, Royal Columbian Hospital, Surrey Memorial Hospital, Burnaby Hospital, Chilliwack General Hospital, Delta Hospital, Eagle Ridge Hospital, Fraser Canyon Hospital, Langley Memorial Hospital, Mission Memorial Hospital, Peace Arch Hospital, and Ridge Meadows Hospital.
Substudy
Electronic chart records of the local Patient Care Information System (PCIS) of all patients who were readmitted to a VCHA hospital within 30-days of the hospital discharge or day of elective PCI were reviewed by one of us ECW, as per the Quality Improvement protocols. The records were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) procedure codes angina pectoris-unstable angina/acute coronary insufficiency/ischemic chest pain as well diagnostic codes for cardiac arrhythmias inclusive of atrioventricular and left bundle-branch block, other conduction disorders, cardiac arrest, paroxysmal tachycardia, atrial fibrillation, other cardiac arrhythmias, and abnormalities of heart beat. We limited our analysis to these diagnostic codes, as this was a quality assurance study, in which we were interested in cardiac readmissions that were most likely related to the index PCI.
Patient demographics (i.e. patient age, sex, comorbidities) were collected. Records of the coronary angiogram and PCI were reviewed for the following data: procedure indication, coronary stent characteristics (type, number, anatomical location of deployment), and complications. The hospital records from the subsequent readmission to a VCHA hospital were reviewed to assess the reason for readmission and relevant interventions, including the need for repeat angiogram and further revascularization.
Data analysis
Descriptive statistics were applied to determine the 30-day overall unplanned readmission rate following coronary angiogram and PCI, and the proportion related to angina pectoris or arrhythmia. The proportion of readmissions related to each cardiac cause and additional complications from the initial PCI was determined. The proportion of cases that underwent a repeat coronary angiogram and need for further PCI was determined, as well as the length of re-hospitalization and mortality when applicable.
Results
During the study period, there were 4,478 patients who underwent a coronary angiogram and attempted PCI at Vancouver General Hospital. Based on administrative records, 108 patients had an unplanned hospital readmission to a VCHA hospital within 30- days during this timeframe. Data was also available for patients who were readmitted to a FHA hospital within 30-days after discharge from their initial PCI from April 1, 2015 up to March 1, 2018, inclusive. There were an additional 50 readmissions across FHA hospitals. Overall, the total number of readmissions across the two largest provincial health authorities was 158, for a cumulative 3.5%, 30-day readmission rate after index PCI.
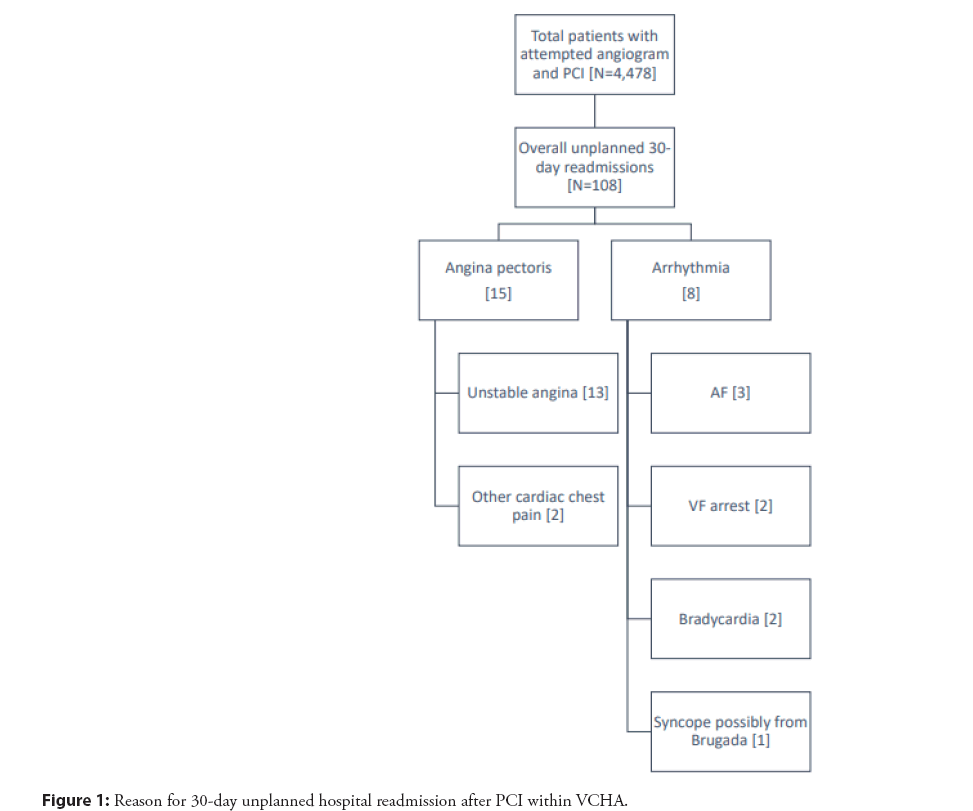
Among the 108 cases readmitted to VCHA (Table 1), 23 cases had a readmission due to either angina pectoris or arrhythmia, representing 21% of all-cause readmissions (Figure 1). These cases met the inclusion criteria for further chart review. The mean age was 69.1 ± 14.3 (SD) years. 25% were female. The majority of patients had dyslipidemia (78%) and hypertension (65%), while a smaller proportion had a previous myocardial infarction (22%), history of heart failure (30%), atrial fibrillation (30%), or valvular disease (22%). The majority of patients did not have previous revascularization from PCI (only 39% had previous PCI) or coronary artery bypass grafting (CABG) (only 26% had a previous CABG).
| Total patients with initial angiogram and attempted PCI | 4,478 |
|---|---|
| 30-day all-cause readmissions-no. (%) | N=108(2.4) |
| Admissions related to angina pectoris or arrhythmia-no. (%) | N=23(21) |
| Status of initial PCI-no. (%) | |
| Successful PCI | 22(96) |
| Attempted PCI | 1(4) |
| Urgency of initial angiogram and PCI-no. (%) | |
| Elective | 4(17) |
| Non-elective | 19(83) |
| Emergent (at time of hospital presentation) | 9 |
| Urgent (during hospitalization but non-emergent) | 10 |
| Indication of initial angiogram and PCI-no. (%) | |
| Stable angina | 4(17) |
| Acute coronary syndrome | 16(70) |
| Unstable angina | 3 |
| NSTEMI | 7 |
| STEMI | 6 |
| Ventricular tachycardia/fibrillation arrest | 3(13) |
| Indication for readmission-no. (%) | |
| Angina pectoris | 15(65) |
| Unstable angina | 13 |
| Other cardiac chest pain | 2 |
| Arrhythmia | 8(35) |
| Atrial fibrillation | 3 |
| Ventricular fibrillation arrest | 2 |
| Bradycardia | 2 |
| Syncope from Brugada | 1 |
| Age-mean ± SD | 69.1 ± 14.3 |
| Sex-no. (%) | |
| Male | 11(48) |
| Female | 12(52) |
| Comorbidities-no. (%) | |
| Dyslipidemia | 18(78) |
| Hypertension | 15(65) |
| Diabetes mellitus | 8(35) |
| Peripheral artery disease | 3(13) |
| Chronic kidney disease | 5(22) |
| Chronic pulmonary disease | 4(17) |
| Atrial fibrillation | 7(30) |
| Valvular disease | 5(22) |
| History of heart failure | 7(30) |
| Previous myocardial infarction | 5(22) |
| Previous PCI | 9(39) |
| Previous CABG | 6(26) |
| Length of hospital readmission (days) | |
| Median ± IQR | 3 ± 2 |
| Mean ± SD | 4 ± 3.3 |
| Status of hospital readmission-no. (%) | |
| Discharged alive Died | 21(91) 2(9) |
| Hospital site of readmission-no. (%) | |
| Tertiary hospital (PCI-capable) Community hospital | 16(70) 7(30) |
Table 1: Characteristics of PCI patient population readmitted to hospital within VCHA.
The majority of cases (22) reported successful single or multi- vessel PCI, with one case of unsuccessful PCI attempt. Cases (19) were not elective procedures and consisted of 9 emergent cases requiring invasive angiography at the time of presentation, and 10 urgent cases undergoing angiography within a few days after hospitalization. The most common indication for coronary angiogram was acute coronary syndrome in 16 cases, followed by 4 cases for stable angina, and 3 cases for ventricular tachycardia or fibrillation arrest (Table 2).
| Total PCIs-no. (%) | N=38 |
|---|---|
| Drug-eluting stent | 37(97) |
| Bare-metal stent | 1(3) |
| Total PCIs per patient case-no. (%) | 23 |
| Drug-eluting stent | 21(91) |
| Bare-metal stent | 1(4) |
| Unsuccessful PCI | 1(4) |
| Mean no. PCI per patient case | 1.7 |
| Location of target vessel for PCI-no. (%) | |
| Right Coronary Artery (RCA) | 11(29) |
| Proximal | 7 |
| Middle | 3 |
| Distal | 1 |
| Left Anterior Descending (LAD) | 21(55) |
| Proximal | 7 |
| 1st diagonal | 2 |
| Middle | 11 |
| Distal | 1 |
| Left Circumflex (LCx) | 4(11) |
| Proximal | 3 |
| Middle | 1 |
| Distal | 0 |
| Left Main (LM) | 1(3) |
| Ramus Intermedius (RI) | 1(3) |
| Complications per patient case-no. (%) | |
| None | 20 |
| Immediate | 2 |
| Delayed | 1 |
Table 2: Result of index coronary angiogram among 30-day unplanned readmissions for angina pectoris or arrhythmias within VCHA.
Among the 22 cases that underwent successful PCI, 21 had at least one drug-eluting stent and 1 had a bare-metal stent. Considering the results of the index coronary angiograms, there was a total of 38 PCIs, with a mean number of PCIs per patient case of 1.7. Among the epicardial vessels, there were 21 PCIs deployed in the Left Anterior Descending (LAD) (55%), 11 PCIs in the Right Coronary Artery (RCA) (29%), 4 PCIs in the left circumflex (11%), and 1 PCI each in the left main and ramus intermedius (3%). The most common revascularized lesions were the proximal LAD and proximal RCA (7 PCIs each).
There were a total of 3 complications directly attributed to PCI, all of which were bleeding related. Two of these complications were immediate and related to access-site hematoma, of which one was minor and the other was severe, requiring intermittent vasopressors and inotropes for further hemodynamic support. There was one case of delayed pulmonary hemorrhage, thought to have been related to the earlier PCI.
The readmission data was summarized. The median length of re-hospitalization was 3 days, with an interquartile range of 2 days. Within the VCHA, most cases were readmitted to a PCI- capable center, with 16 cases to a tertiary hospital, and 7 cases to a community hospital. There were 15 cases readmitted for angina pectoris, with most being unstable angina, and 8 cases for arrhythmia. Among the arrhythmias, there were 3 cases of atrial fibrillation with rapid ventricular response, 2 cases of bradycardia, 2 cases of ventricular fibrillation arrest, and 1 case of syncope thought to be related to Brugada syndrome. There were two deaths during the rehospitalization period, both in the setting of ventricular fibrillation arrest.
A repeat coronary angiogram was performed in 12 of the 23 cases during the hospital readmission. Among these, only 2 cases underwent further revascularization with PCI. No intervention (i.e. conservative management) was pursued for the other 10 cases, with 7 of these showing patent stents with no new obstructive lesion for PCI, while the other 3 showed potential angiographically- significant lesions but were not amenable for further PCI. In one case, revascularization of the residual lesion was considered, but would have required a long stent. In another case, an occluded small apical branch of the left anterior descending artery was found. In the third case, the decision was made against another PCI as the procedure was considered not to be feasible, because it required stenting of the proximal intermedius that risked damage to the left main artery.
Discussion
This quality assurance study found that among 4,478 patients who underwent a coronary angiogram and PCI at a tertiary hospital, only a small proportion (3.5%) had an unplanned hospital readmission within 30-days to any hospital in our region or in any of the adjacent regional hospitals. The Vancouver Coastal and Fraser Health regions represent a total population of over 3 million residents. Our readmission rate was less than one-half of the reported readmission rates of 7.2% from the CIHI data. Importantly, only one-fifth of local readmissions were related to a metric of PCI quality, specifically angina pectoris (unstable angina/ acute coronary insufficiency/ischemic chest pain) or arrhythmia.
The majority of cases of readmission were for unstable angina, and had initially been admitted to hospital for acute coronary syndromes requiring urgent PCI that employed drug-eluting stents. From our data, nearly half underwent a repeat coronary angiogram during the readmission, but only a smaller proportion required further revascularization. In the 30-day timeframe, there were no readmissions related to stent thrombosis, a serious complication of PCI [18].
The low proportion of 30-day unplanned readmission for angina pectoris (unstable angina/acute coronary insufficiency/ischemic chest pain) or arrhythmia in this study suggests the majority of readmissions are likely not due to a poor PCI outcome. We had defined a pre-specified set of readmission criteria to focus on potential cardiac reasons related to the index PCI, in which readmissions for heart failure, staged procedures or other non- cardiac reasons were excluded from further detailed analysis. In comparison to CIHI’s national metrics, this furthermore suggests that a vast proportion of overall unplanned PCI readmissions at our institution are non-cardiac related. This finding is consistent with other studies which have similarly identified that a majority of readmissions after PCI are due to non-cardiac reasons, with only a small proportion having major bleeding complications [19].Taken together these data support the contention that although a reason for presentation after PCI is for evaluation of recurrent chest pain or angina, only a minority are diagnosed with myocardial infarction requiring hospital readmission.
Potential reasons for our lower overall readmission rate in comparison to CIHI 8 are likely multifactorial. First, patients re- presenting to the emergency department with stable angina and reassuring investigations are often discharged from the emergency department to undergo non-invasive testing with an expedited follow-up. This would imply that some other Canadian centers might have a lower threshold for hospital readmission. Second, the majority of patients discharged from our tertiary hospital after myocardial infarction with PCI are discharged with suggested routine outpatient cardiology follow-up within 2-3 months, thus possibly deferring an unplanned emergency department visit.
Our findings further emphasize the importance of quality assurance through a retrospective chart review to provide further context on readmission rates, compared to administrative data alone. This has been similarly identified in other studies, in which registry data may not be inclusive of all comorbidities and complications that may impact readmission [20]. Meanwhile, patient characteristics derived from electronic medical records can be more predictive of hospital readmission after PCI [21]. Our study reinforces the message that healthcare administrators must seek to validate administrative records with detailed case analysis in order to understand the true disease burden and readmission rates within its population. Reliance on CIHI’s metrics alone without comparison to individual cardiac centers may be insufficient in understanding contextual factors of the causes and predictors of unplanned PCI readmissions. This has further downstream implications on resource management within the system.
We found that readmission occurred mainly in those who had urgent PCI. Hospitals can potentially reduce short-term readmission rates by stratifying patients according to their individualized risk for an early readmission after PCI. Focus should be on this group to minimize readmission rates. Risk prediction scores and models have been developed by institutions to estimate the risk of readmission using clinical factors present at the time of PCI [22]. Patients with higher-risk features, such as those with significant residual coronary disease left untreated following the index PCI, should be prioritized for earlier follow-up.1 Furthermore, interventions as part of comprehensive discharge planning including robust medication and symptom counselling, home and rehabilitation supports, as well as the role for telemonitoring and self-management-focused education programs have been validated in other settings. A multidimensional approach using a validated questionnaire to identify patients at higher risk for readmission after PCI, followed by subsequent targeted interventions, produced a 4.3% decline in readmissions over a 4-year period [23]. Implementation of a uniform regional-based algorithm for patients re-presenting to the emergency department following recent PCI may further guide risk stratification to help with clinical decision making and prevent potentially unnecessary readmissions across all hospital sites.
This study should be interpreted in the context of several potential limitations. First, there are general limitations of retrospective analysis; given the possibility for reporting bias. Second, this was largely a single-center quality assurance study, in which the generalizability of the results to other hospital and healthcare systems needs further investigation. Third, readmissions to other hospitals outside these health regions are possible. However, this would likely not meaningfully alter our results as the vast majority of patients live within the VCHA and FHA regions. Further these two regions constitute about 60% of the entire population of the province. Two other regions of the province have PCI centers so that patients in those regions would have had their PCI done there and not at VCHA. Fourth, detailed information regarding other patient medical comorbidities, for example frailty, a measure which has been shown to affect PCI outcomes [24], was not included in this analysis. Lastly, the scope of this study could not provide a parallel health economics analysis. The financial costs of readmission, including the potential need for repeat angiogram or PCI, contribute to overall cumulative costs of the initial procedure. There is a need for further research examining the cost analysis and longer-term patient outcomes of unplanned PCI readmissions, and its preventability within the healthcare system.
Conclusion
In this quality assurance study, the overall 30-day unplanned readmission rate after discharge from PCI at a tertiary care hospital is much lower than the nationally reported mean. Furthermore, only a small percentage, about one-fifth, of readmissions were due to angina pectoris (unstable angina/acute coronary insufficiency/ ischemic chest pain) or arrhythmia which are a potential quality metric for assessment of PCI. Detailed case analysis is necessary to define true readmission rates, as well as the causes of readmission. Readmission was almost exclusively in patients who were initially admitted for an acute coronary event, suggesting the need to focus attention on these individuals prior to discharge. Accurate quality assurance data can help guide resource allocation and planning at discharge.
References
- Kwok CS, Rao SV, Potts JE, et al. Burden of 30-day readmissions after percutaneous coronary intervention in 833,344 patients in the United States: Predictors, causes, and cost: Insights from the nationwide readmission database. JACC Cardiovasc Interv. 11(7):665-674 (2018).
- Kalra A, Shishehbor M, Simon D, et al. Percutaneous coronary intervention readmissions: Where are the Solutions? JACC Cardiovasc Interv. 11(7):675-676 (2018).
- Kwok CS, Hulme W, Olier I, et al. Review of early hospitalisation after percutaneous coronary intervention. Int J Cardiol. 227:370-377 (2017).
- Spitzer E, Frei M, Zaugg S, et al. Rehospitalizations following primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction: Results from a multi-center randomized trial. J Am Heart Assoc. 6(8): e005926 (2017).
- Vidula MK, McCarthy CP, Butala NM, et al. Causes and predictors of early readmission after percutaneous coronary intervention among patients discharged on oral anticoagulant therapy. PLoS One. 13(10):1-15 (2018).
- Strom JB, Yeh RW. Should we care about short-term readmissions after percutaneous coronary intervention? Circ Cardiovasc Interv. 10(12):20-22 (2017).
[CrossRef][Google Scholar][PubMed]
- Canadian Institute for Health Information. (2017).
- Welsh RC, MacFarlane K, Quraishi A ur R, et al. Canadian cardiovascular society and canadian institute of health information public reporting of percutaneous coronary intervention quality indicators. Can J Cardiol. 34(12):1539-1540 (2018).
- Tripathi A, Abbott JD, Fonarow GC, et al. Thirty-day readmission rate and costs after percutaneous coronary intervention in the United States: A national readmission database analysis. Circ Cardiovasc Interv. 10(12):19 (2017).
- Corbellini C, Andreoni B, Ansaloni L, et al. Reliability and validity assessment of administrative databases in measuring the quality of rectal cancer management. Tumori. 104(1):51-59 (2017).
- Zhu K, Lou Z, Zhou J, et al. Predicting 30-day hospital readmission with publicly available administrative database: A conditional logistic regression modeling approach. Methods Inf Med. 54(6):560-567 (2015).
- Donabedian A. An Introduction to quality assurance in health care. (2002).
- Yost GW, Puher SL, Graham J, et al. Readmission in the 30 days after percutaneous coronary intervention. JACC Cardiovasc Interv. 6(3):237-244 (2013).
- Wasfy JH, Strom JB, O’Brien C, et al. Causes of short-term readmission after percutaneous coronary intervention. Circ Cardiovasc Interv. 7(1):97-103 (2014).
- Yao RJR, Andrade JG, Deyell MW, et al. Sensitivity, specificity, positive and negative predictive values of identifying atrial fibrillation using administrative data: A systematic review and meta-analysis. Clin Epidemiol. 11:753-767 (2019).
- Burden of 30-day readmissions after percutaneous coronary intervention in 833,344 patients in the United States: Predictors, causes, and cost: Insights from the nationwide readmission database
- Fraser Health. About Fraser Health: Our Communities. (2021).
- Torrado J, Buckley L, Durán A, et al. Restenosis, Stent thrombosis, and Bleeding complications: Navigating between scylla and charybdis. J Am Coll Cardiol. 71(15):1676-1695 (2018).
- Kwok CS, Narain A, Pacha HM, et al. Readmissions to hospital after percutaneous coronary intervention: A systematic review and meta-analysis of factors associated with readmissions. Cardiovasc Revasc Med. 21(3):375-391 (2020).
- Fanari Z, Elliott D, Russo CA, et al. Predicting readmission risk following percutaneous coronary intervention at the time of admission. Cardiovasc Revasc Med. 18(2):100-104 (2017).
- Wasfy JH, Singal G, O’Brien C, et al. Enhancing the prediction of 30-day readmission after percutaneous coronary intervention using data extracted by querying of the electronic health record. Circ Cardiovasc Qual Outcomes. 8(5):477-485 (2015).
- Minges KE, Herrin J, Fiorilli PN, et al. Development and validation of a simple risk score to predict 30-day readmission after percutaneous coronary intervention in a cohort of medicare patients. Catheter Cardiovasc Interv. 89(6):955-963 (2017).
- Tanguturi VK, Temin E, Yeh RW, et al. Clinical interventions to reduce preventable hospital readmission after percutaneous coronary intervention. Circ Cardiovasc Qual Outcomes. 9(5):600-604 (2016).
- Murali-Krishnan R, Iqbal J, Rowe R, et al. Impact of frailty on outcomes after percutaneous coronary intervention: A prospective cohort study. Open Heart. 2(1):e000294 (2015).