Commentary - Interventional Cardiology (2013) Volume 5, Issue 5
The use of subintimal pathways to facilitate chronic total occlusion procedural success
- Corresponding Author:
- Julian W Strange
Cardiac Catherization Laboratory
Bristol Heart Institute, University Hospital Bristol
Bristol, BS2 8HW, UK
E-mail: julian.strange@uhbristol.nhs.uk
Abstract
The use of the subintimal space to facilitate chronic total occlusion (CTO) angioplasty has, over the years, caused a degree of controversy. Some experts recommend avoiding the subintmal space at all cost, whereas others place it squarely within an algorithm to help achieve an efficient, effective and safe CTO program. There is no doubt that the use of the subintimal space has improved CTO procedural success, defined as luminal continuity and thrombolysis in myocardial infarction grade III flow, with more operators reporting 95% success rates in unselected cases. However, the preferred techniques used to achieve this have evolved, with some becoming historical or a last resort. The debate over the role of the subintimal space and its long-term safety still continues. This article will aim to give insight into the anatomy, techniques and outcomes in subintimal CTO intervention.
Keywords
adventitia, angioplasty, antegrade, chronic total occlusion, dissection re-entry, retrograde subintimal
Subintimal space
The use of the subintimal space to facilitate chronic total occlusion (CTO) angioplasty has, over the years, caused a degree of controversy. Some experts recommend avoiding the subintmal space at all cost, whereas others place it squarely within an algorithm to help achieve an efficient, effective and safe CTO program. There is no doubt that the use of the subintimal space has improved CTO procedural success, defined as luminal continuity and thrombolysis in myocardial infarction grade III flow, with more operators reporting 95% success rates in unselected cases. However, the preferred techniques used to achieve this have evolved, with some becoming historical or a last resort. The debate over the role of the subintimal space and its long-term safety still continues. This article will aim to give insight into the anatomy, techniques and outcomes in subintimal CTO intervention.
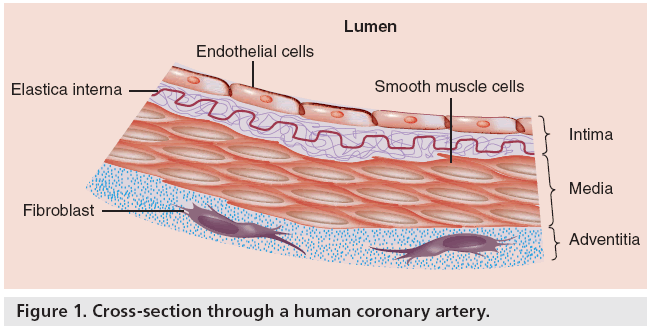
Anatomy of a coronary artery
The epicardial coronary artery wall contains smooth muscle cells and is, hence, a muscular artery allowing dilatation and constriction depending on physiological demands. Coronary arteries are rather unique; there is a specialized thick layer of longitudinal muscle and fibrous tissue bound to the internal elastic lamina, which enables the vessel to accommodate to the marked changes in length during the cardiac cycle. There are three main anatomical layers (Figure 1). The innermost layer is the intima; it consists of a single layer of endothelial cells supported by a thin subendothelial connective tissue layer organized longitudinally. Next, sandwiched between the internal and fenestrated external elastic lamina is the fibromuscular media, which has a circumferential organization of nonstriated myocytes with scattered elastic membranes and a few collagen fibers. The outermost layer is known as the adventitia and is composed of collagen and elastin fibers, which run predominantly in a longitudinal direction. The outer portion of the adventitia blends rather loosely with the fibroareolar tissue, allowing considerable movement between the artery and neighboring structures.
Layer-specific mechanical properties
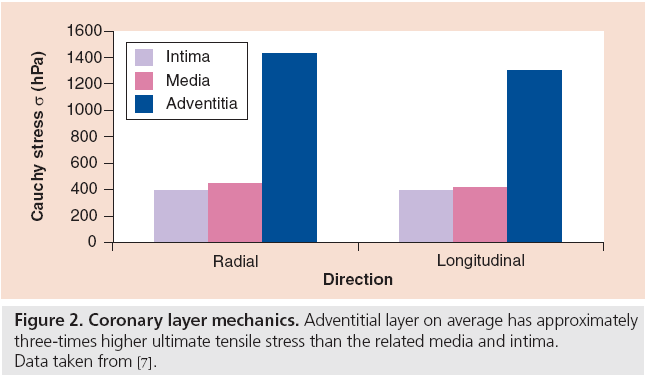
The different layers of the coronary artery display marked heterogeneity in their mechanical properties. It is the characterizing and understanding of the mechanical properties of the coronary artery that has enabled equipment and technique advancement. As percutaneous coronary intervention (PCI) operators, we vary our technique depending on the physical attribute of the whole vessel, whether this is the extent of atheroma, the degree of tortuosity or the level of calcification. When dealing with the different layers of the coronary artery, in this case luminal versus subintimal coronary intervention, adaption also needs to occur. Many of the arterial wall models are based upon a ‘single layer’ homogeneous wall structure or animal models and therefore these assume that the mechanical properties do not differ through the wall thickness. These coronary models are potentially flawed, especially as the intimal layer that develops throughout human life can exhibit considerable mechanical strength. This process of intimal development is not seen in nonatherosclerotic animals, while the different arterial tissue layers in human coronaries display marked mechanical heterogeneity.
Intima
The intima layer can thicken considerably with aging. Intimal cells, mainly myofibroblasts, proliferate concentrically and form, on average, 30% of the total wall thickness in middle-aged human coronaries. The intima has impressive load bearing capacity and strength.
Media
The media is the softest layer which, due to the orientation of fibers, deforms most at set levels of stretch.
Adventitia
At high levels of stretch, the adventitia, having initially deformed, becomes ‘jacket-like’ and prevents the artery from overstretch or rupture. Its tensile strength is over three-times that of the media or intima layers (Figure 2).
Subintimal space in CTO PCI
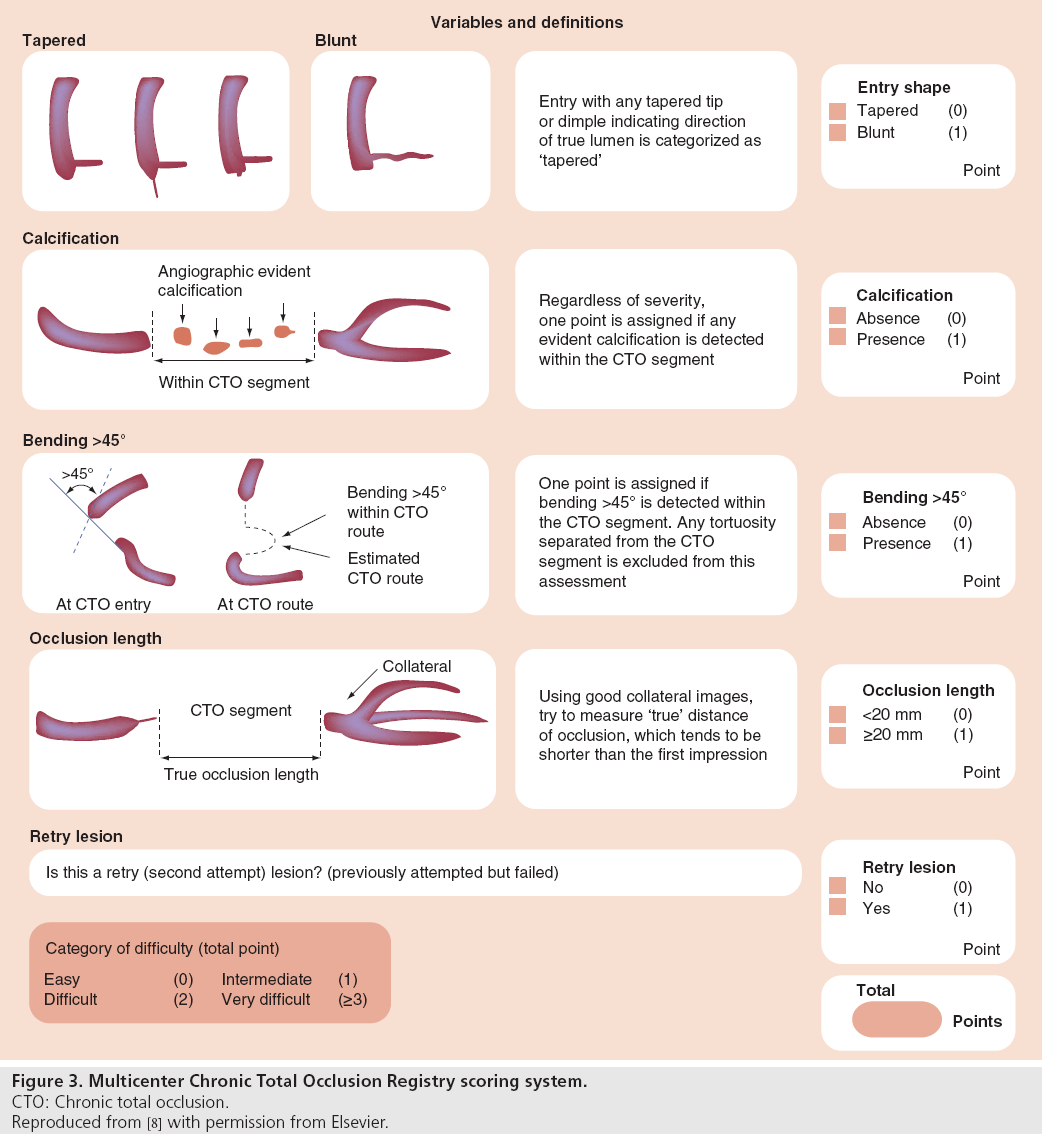
Historically the subintmal space, which lies between the intima and adventitia, has been feared by coronary interventionalists with the notion that the coronary wire should be steered within the true lumen along the length of a stenosis or occlusion. Failure of guidewire passage with subintimal tracking is recognized as the most common cause of PCI failure. However, the success of luminal antegrade wiring diminishes rapidly with increase in the Multicenter CTO Registry score (Figure 3); long occlusion, an ambiguous (poorly visualized) proximal cap and calcification all having a negative impact on wire passage. Subintimal passage of guidewires is not rare even in successfully wired CTO cases, despite the operator’s belief that antegrade (or retrograde) wire passage has been luminal. Reported intravasular ultrasound studies of successful CTO cases have confirmed subintimal passage in a high percentage of cases [1,2]. The publication of these data has improved our understanding of guidewire course in CTO and has challenged the mistaken acceptance that antegrade wire passage through a long coronary occlusion is within the true lumen throughout its length.
Figure 3: Multicenter Chronic Total Occlusion Registry scoring system.
CTO: Chronic total occlusion.
Reproduced from [8] with permission from Elsevier.
Subintimal tracking was first described in the peripheral circulation in 1989 by Bolia et al. with the report of successful recanalization of 26 femoropopliteal occlusions by the subintimal route [3]. The aim of subintimal angioplasty is to create a channel between the intima and the media by means of an intentional dissection. Several specific techniques use the subintimal angioplasty approach, with both antegrade and retrograde approaches having been described. Below is a description of the most commonly used techniques for treating CTOs, which rely on subintimal or commonly created subintimal passage of guidewires.
Antegrade wiring
There is a commonly held misconception that antegrade wiring of a CTO does not involve the subintimal space. Several studies have looked, with the aid of intravascular ultrasound, at wire passage in antegrade wired CTOs. Mohandes et al. [1] and Fujii et al. separately describe intramural hematoma in successfully wired CTOs [2]. This intramural hematoma represents wire passage into the subintimal space. In these unselected cases, in a total of 90 patients, subintimal passage occurred 26% and 34% of the time in the respective reports. The incidence of intramural passage increased significantly with long calcified lesions in the small arteries. These two studies also demonstrate the safety of subintimal balloon predilation and stent implantation in achieving successful CTO PCI.
Subintimal antegrade wire positioning is described and used in the ‘parallel wiring’ technique, where the initial wire is used as a marker of subintimal passage and another wire is selected to steer into the purported true lumen. ‘See-saw’ wiring involves switching between the guidewires to work through the occlusion segment. These techniques often require the use of stiff penetrative guidewires that run the risk of vessel perforation and do not provide predictable entry into the distal true lumen. It is evident that very long true lumen passage of a guidewire for its entire course is unlikely in CTO PCI. This is reflected in modern CTO algorithms that suggest alternatives to antegrade wiring when the occluded segment is longer than 20 mm [4].
Controlled antegrade and retrograde subintimal tracking technique
The controlled antegrade and retrograde subintimal tracking (CART) technique requires the simultaneous use of antegrade and retrograde approaches. The principle is to create a subintimal dissection at the site of the CTO. It was described in 2006 by Surmely et al., and involves the passage of antegrade wire to the proximal cap where it is advanced into the subintimal space [5]. A retrograde wire, via an appropriate collateral and supported on a microcatheter to facilitate wire movement and protect the retrograde channel, is then passed at the distal cap of the CTO and then subintimally. A retrograde low-profile balloon is then inflated at the CTO site and this allows relatively easy communication of the antegrade wire with the distal true lumen. The retrograde balloon is left in place to keep the subintmal space open and to communicate with the distal true lumen while antegrade passage occurs.
Reverse CART
Reverse CART utilizes a similar approach with both antegrade and retrograde wires. However, the subintimal channel is enlarged by advancing and inflating an antegrade balloon in order to create a communication of the two subintimal spaces. The retrograde wire is then advanced into the proximal true lumen. This retrograde wire is externalized through the guiding catheter and is used as a rail for subsequent antegrade angioplasty and stenting.
Subintimal tracking and re-entry technique
Subintimal tracking and re-entry was the first reported antegrade dissection re-entry technique. It involves the forceful advancement of a knuckled polymeric guidewire within the subintimal space, past the CTO, towards the distal branches of the occluded vessel to create a communication between true and false lumens. This technique has fallen out of favor owing to both poor short- and long-term results. The short-term issues are the unpredictable nature of the technique, the lack of control over the reentry point and the potential loss of important side branches and possible difficulty in gaining access into the true distal lumen. Long-term results are compromised owing to the morbidity associated with the probable ongoing ischemia, the relatively long length of stent required and poor drainage into small coronary side branches. This technique was felt to be most appropriate for the right coronary artery owing to the relative lack of important side branches. Despite all these disadvantages, it did effectively demonstrate that blunt dissection through the subintimal space allowed rapid traversal of occluded segments without perforation of the adventitia. This, in turn, stimulated the development of controlled subintimal dissection.
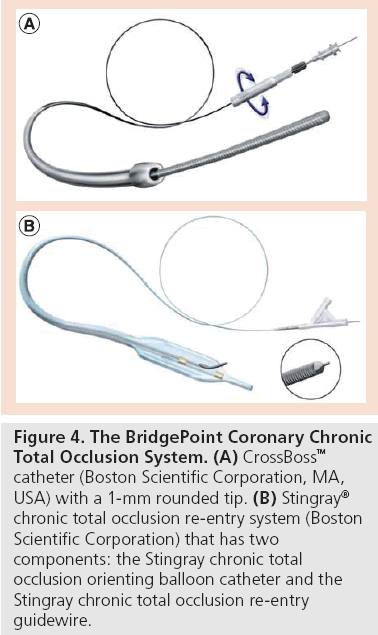
Antegrade dissection and re-entry techniques
Antegrade dissection and re-entry offers an alternative to antegrade wiring and retrograde techniques. It can be used when retrograde options are limited or anatomy is unfavorable for antegrade wiring. It may also be used as an alternative primary strategy to the retrograde technique in selected cases. Controlled re-entry is achieved through control of the subinitimal dissection plane, visualization of the distal vessel using contralateral injections with subsequent planned and carefully positioned true lumen re-entry. The technique has been previously described as the limited antegrade subintimal tracking technique in which either a stiff Confianza Pro 12 wire (Asahi Intecc Co., Aichi, Japan) or a Pilot 200 wire (Abbot Vascular, CA, USA) is used to form a 90° distal bend. A more predictable dedicated system has recently been designed to facilitate this technique increasing success rates. This BridgePoint System (Boston Scientific Corporation, MA, USA) consists of a microcatheter (CrossBoss™) that rapidly traverses the subintimal space, a balloon catheter (Stingray®) with a flat design and bilateral side ports and a dedicated stiff penetrative (Stingray wire) wire (Figure 4). The short- and mediumterm safety and efficacy of this system has been demonstrated in complex CTO patients, and provides a unique solution in patients with long occlusions.
Figure 4: The BridgePoint Coronary Chronic Total Occlusion System. (A) CrossBoss™ catheter (Boston Scientific Corporation, MA, USA) with a 1-mm rounded tip. (B) Stingray® chronic total occlusion re-entry system (Boston Scientific Corporation) that has two components: the Stingray chronic total occlusion orienting balloon catheter and the Stingray chronic total occlusion re-entry guidewire.
Outcomes and conclusion
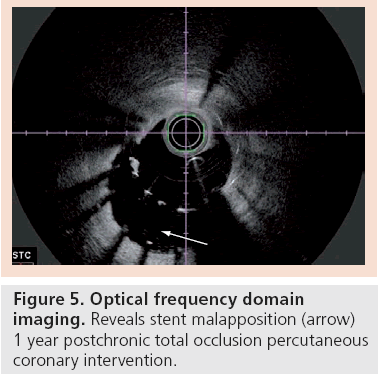
The range of subintimal dissection and re-entry techniques has been employed more frequently as the hybrid approach to PCI for CTO continues to evolve [4]. The consequences of subintimal dissection, whether it be antegrade or retrograde, and stent insertion in the subintimal space remain unclear; in particular, it remains to be established as to whether more aggressive PCI strategies with greater degrees of subintimal disruption are more likely to develop stent malapposition, which may be a risk factor for stent thrombosis (Figure 5). Certainly, the shortand medium-term patient benefit can be demonstrated, with 95% success rates for an increasing number of CTO operators [6]. Little is known about the long-term outcomes and consequences of stent insertion in the subintimal space. In addition, it is yet to be established whether more aggressive strategies with substantial subintimal disruption are more likely to cause problems, such as stent malapposition (early or late), and whether such malapposition is a risk factor for clinical events such as stent thrombosis. Stent malapposition is not uncommon after PCI for CTOs where subintimal dissection featured as part of the initial procedure and appears to be worse at sites in the vessel where more aggressive strategies are employed. The implications for long-term clinical outcomes remain unclear and warrant further investigation.
Financial and competing interests disclosure
JW Strange has received proctorship fees from Abbott Vascular and Boston Scientific Corporation for teaching and training in chronic total occlusions. The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Mohandes M, Guarinos J, Sans J, Bardaji A. Intravascular ultrasound in percutaneous coronary intervention for chronic total occlusion. Int. Cardiovasc. Res. J. 4(3), 101–106 (2010).
- Fujii K, Ochiai M, Mintz GS et al. Procedural implications of intravascular ultrasound morphologic features of chronic total coronary occlusions. Am. J. Cardiol. 97(10), 1455–1462 (2006).
- Bolia A, Brennan J, Bell PR. Recanalisation of femoro-popliteal occlusions: improving success rate by subintimal recanalization. Clin. Radiol. 40(3), 325 (1989).
- Brilakis ES, Grantham JA, Rinfret S et al. A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc. Interv. 5(4), 367–379 (2012).
- Surmely JF, Tsuchikane E, Katoh O et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J. Invasive Cardiol. 18, 334–338 (2006).
- Smith EJ, Strange JW, Hanratty CG, Walsh SJ, Spratt JC. Percutaneous intervention for chronic total occlusion: integrating strategies to address an unmet need. Heart 99(20), 1471–1474 (2013).
- Holzapfel GA, Sommer G, Gasser CT, Regitnig P. Determination of layer-specific mechanical properties of human coronary arteries with nonatherosclerotic intimal thickening and related constitutive modeling. Am. J. Physiol. Heart Circ. Physiol. 289(5), H2048–H2058 (2005).
- Morino Y, Abe M, Morimoto T, Kimura T et al.; J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc. Interv. 4(2), 213–221 (2011).