Review Article - Neuropsychiatry (2017) Volume 7, Issue 2
Therapeutic Approach of Acupuncture for Sciatica: A Brief Review
- Corresponding Author:
- Fang-Pey Chen, M.D., Director
Center for Traditional Medicine, Taipei-Veterans General Hospital, Taipei, Taiwan, Associate Professor, Institute of Traditional Medicine, School of Medicine, National Yang-Ming University, Taipei, Taiwan, Republic of China
Tel: +886-2-2875-7454
Fax: +886-2-2875-7452
E-mail: fpchen@vghtpe.gov.tw
Abstract
Acupuncture has been proposed to treat various diseases including functional gastrointestinal disorder, mood disorder, and pain. Although the evidence-based clinical efficacy of acupuncture is uncertain, people are increasingly benefiting from the use of acupuncture to treat their diseases. Sciatica treatments involve nonsurgical and surgical management techniques; acupuncture, for its convenience and cheap cost, could be considered as a premedical or adjunctive therapy. Analysis of 14 studies published to treat sciatica with acupuncture revealed that meridians and acupoints chose is an essential issue to get better pain alleviating results. Sciatica through acupuncture treatments may include the use of the bladder and gall bladder meridians. However, for limited evidence of effectiveness in the relevant studies, a series of larger randomized controlled trials should be conducted on the efficacy of acupuncture in treating sciatica to provide further evidence.
Keywords
Acupuncture, Sciatica, Mood disorder, Spinal intervertebral disc herniation, Chinese medicine
Introduction
Sciatica is a common pain disorder that typically presents as lower back or gluteal pain which may radiate out to one leg in the form of motor or sensory disturbances [1,2]. Sciatica has recently drawn more attention worldwide as a public health concern for its disabling pain, high prevalence, and substantial medical and economic burden [3,4]. Diagnosis of sciatica involves physical and neurological examinations. Sciatica is characterized by radiating pain below the knee that follows dermatomal patterns at the L4, L5, or S1 nerve root distribution with or without neurological deficits. Magnetic resonance imaging (MRI) of the lumbosacral plexus is occasionally required to locate tumors and other causes of sciatic nerve or plexus compression [4-7]. Although the pathophysiology of sciatica has been considered to be caused by regional nerve root compression by spinal intervertebral disc herniation [2,5,6] other mechanical local processes have been identified that involve the spine and surrounding structure such as muscles, ligaments, periosteum, facet joints, nerves, and blood vessels [8]. The outcome of sciatica patients was not related to MRI findings regarding disc herniation; the prognostic outcome was even poorer when disabling back pain from sciatica coexisted with an absence of a herniated disc with nerve root compression as determined by MRI [9,10]. The prevalence of sciatica varies, from 1.2% to 43%; this may be due to different defined diagnoses and methodology for the data collection of specific populations [4].
In a study of lumbar disc herniation in a Chinese population, physical exercises and sleeping on a hard bed were determined to be possible protective factors and the family history of lumbar intervertebral disc herniation, lumbar load, and daily intensity of work were determined to be the major risk factors for sciatica [11].
Sciatica as a chronic pain has been the target of various treatments including mainstream and complementary therapies such as acupuncture. The latest Cochrane meta-analysis suggested that for patients with sciatica, little or no difference existed between patients resting in bed and those staying active [12]. A recent systemic review and meta-analysis of drugs for sciatica pain relief discovered that the primary care management of sciatica is still unclear [13]. Another study involving a network meta-analyses of the comparative clinical effectiveness of management strategies for sciatica demonstrated that for overall outcome, a statistically significant improvement was observed for disc surgery, epidural injections, non-opioid analgesia, manipulation, and acupuncture [14]. In other studies, surgical intervention had a similar outcome as conservative treatment did; however, the rates of pain relief and of perceived recovery were faster for patients assigned to early surgery [1,15,16].
Acupuncture, which has a long history in ancient China as a traditional treatment modality in Chinese medicine, has been increasingly used in diverse pain alleviation applications in the Western world since the 1970s. Regarding treating sciatica patients through acupuncture, some observational studies have revealed benefits, [17-23] and some remained inconclusive [2,5,14,24]. Therefore, in this review, we discuss the history of acupuncture, its progressively extensive use in treating clinical pain syndrome, observational studies about and strategies for treating sciatica with acupuncture, and the selection of acupoints. Finally, the current therapeutic effectiveness of acupuncture treatment for treating sciatica is discussed.
Historical Background
▪ 1920s – 1970s
Sciatica has long been considered a problem requiring sophisticated treatment. A study in 1921 described the recovery of a mild case of sciatica after bed rest or sedative application; however, more severe cases required comprehensive pharmacological management [25]. An author first introduced the electrical acupuncture method with a galvanic battery based on induced hyperemia to relieve pain [25]. An improvised apparatus for applying acupuncture to treat sciatica and neuritis, such as trigeminal neuralgia, was also mentioned [26,27]. Attention to the analgesic effect of acupuncture has increased since the 1970s, when American visitors to China began discovering acupuncture for its considerable anesthetic effect in major surgical operations [28]. Once acupuncture became mainstream of Complementary and Alternative Medicine (CAM) in America, manifesting as “a flood of laudatory descriptions of the achievements of acupuncture” [29] debate about and challenges to the therapeutic effect of acupuncture began, as well as inquiry into whether acupuncture could actually treat diseases. Experts of that time considered that acupuncture was a type of hypnosis, psychotherapy, and operant conditioning [29]. However, some practical acupuncturists maintained that the differences between acupuncture therapy and analgesia should be clarified [30]. For the aforementioned reasons, scientific approaches have been increasingly executed to investigate the physiological background of acupuncture for pain relief. In a clinical observational study, acupuncture was suggested to obtain the best responses in patients with musculoskeletal disorders, degenerative osteoarthritis, and headaches [31]. Kwasucki, et al. used a modification of acupuncture associated with chemical stimulation in 144 patients with painful radicular syndromes and headaches, including 57 sciatic pain patients, and observed that pain disappeared in approximately 40% of cases of radicular syndromes and in 62% of cases of headaches [32].
▪ 1980s – 2000s
On the basis of the experience derived from treating acute attacks of lumbar sciatic pain, Collier concluded that acupuncture or local injection of analgesic solution can hasten pain remission [33]. In June 1979, the World Health Organization (WHO) conducted a symposium on acupuncture in Beijing, China, and created a list of 43 diseases that might benefit from acupuncture, and sciatica is one of these diseases [34]. The official report on the effectiveness of acupuncture that is based on data from controlled clinical trials before the end of 1998 was published in 2003 [35]. The results suggested that acupuncture was an effective treatment of sciatica.
Methods
The search strategy as used both medical subject headings (MeSH) and key words in article titles and abstracts in PUBMED with ‘sciatica’, ‘acupuncture’, a total of 97 literatures were searched. Non-target studies were excluded base on the following criteria: papers with nonhuman studies, papers with case report, treat with non-manual or non-electroacupuncture , review, non-English or non-Chinese literature, non-clinically officious assessment and nontarget to sciatica were all be excluded and 14 literature were identified.
Results
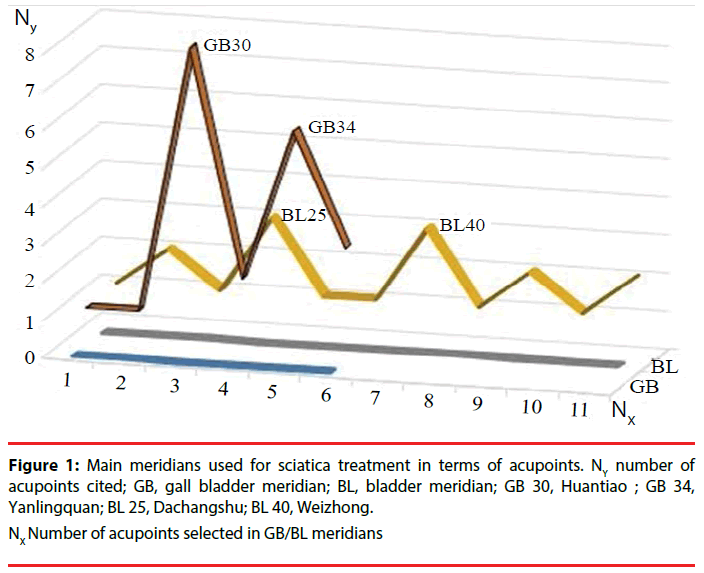
There were 8 observational and 6 randomized controlled trials. Almost all of these studies were through manual acupuncture, except 2 for electroacupuncture and one for mixed with catgut implantation. Patients with chronic sciatica had drawn more attention than with acute sciatica in acupuncture treatment. The treatment session varies; form one session to 30 or 50 sessions. Nevertheless, nearly 40% sciatic patients cured after acupuncture treatment and one study revealed only 28% of analgesic effect persistently (Table 1). The most of all studies chose bladder (BL) meridian and gall bladder (GB) meridians for treating sciatic and, GB 30 and GB 34 were both higher selected accupoints. Generally, the acupoints selected from GB meridian were concentric and less in number, yet through BL meridian, were more extensively and more in number (Table 2 and Figure 1).
| Authors | Design | Intervention | Age | Case number, M:F | Duration | Treatment session | Therapeutic effect | |
|---|---|---|---|---|---|---|---|---|
| Leung, 1973 [54] | observation | MA | 30-60 | 56, 27:29 | NA | 1-6 | 94.5% of improvement after 4 treatment | |
| Domzal, et al. 1980 [55] | observation, | MA | NA | 107, NA | NA | NA | persistent analgesic effect 28% | |
| Duplan, et al. 1983 [47] | randomly, | EA | NA | 15, NA | NA | NA | statistically significant improved | |
| Jiang, et al. 1984 [17] | observation | MA | 21-70 | 106, NA | 2d-3 years | 3-50 | 50% cured, 35.5% marked improved | |
| Qi, et al. 1985 [16] | observation | MA | NA | 145, NA | NA | 15 | 42.7% cured, total effective rate 95.7% | |
| Li, et al. 1989 [18] | observation | MA | 23-70 | 101, 63:38 | 1.95-2.13 years | 2-10 | 63.3% cured, 16.7% marked improved | |
| Pei, et al. 1994 [19] | observation | MA | 23-67 | 84, 52:32 | 1-3 years | 1-3 | 72.6% cured, 7.1% marked improved | |
| Wehling, et al. 1997 [53] | observation, | MA | NA | 230, NA | > 3 month | NA | improved the pain in average of 62% | |
| Wang, et al. 2003 [22] | observation, | MA | 15- 51 years. | 50, 27:23 | 7d-5 years | 20 | 40% cure, 30% markedly effective | |
| Tang, et al. 2007 [23] | randomly, | MA, catguts | 35-64 yeas | 72, 43:29 | 5 month -4 years | 1-3 | 52% cure, 44% markedly effective | |
| Wang, et al. 2009 [48] | randomly | EA | NA | 70, NA | NA | NA | 41.4% cure | |
| Chen, et al. 2009 [43] | randomly, | MA | 28- 40 yeas | 30, 22:8 | 2-8 years | 30 | 57% cure, 33% markedly effective | |
| Zhao, et al. 2011 [42] | randomly, | MA | NA | 30, NA | NA | 5 | The total effective rates were 100.0% | |
| Lee, et al. 2015 [44] | randomly | MA | NA | 20, NA | 4 weeks-6 month | 8 | NA (proposal) | |
Table 1: Summary of reviewed studies.
| Authors | Intervention | Meridians | lateralization | Acupoints |
|---|---|---|---|---|
| Leung, 1973 [54] | MA | GB, BL | NA | GB 25, GB 30, GB 31, BL 23, BL 36 |
| Domzal, et al. 1980 [52] | MA | NA | NA | NA |
| Duplan, et al. 1983 [47] | EA | NA | NA | NA |
| Jiang, et al. 1984 [17] | MA | GB, BL, SP, ST | NA | GB 30, GB 31, GB 34, GB 39, BL 23, BL 54, BL 57, BL 60, SP 6, ST 36 |
| Qi, et al. 1985 [16] | MA | GB, BL | NA | GB 30, GB 34,GB 39, BL 23, BL 25, BL 26, BL 52, BL 57, BL 60, |
| Li, et al. 1989 [18] | MA | GB, BL | NA | GB 30, GB 34, GB 39, BL 25, BL 32, BL 37, BL 40, BL 54, BL 60 |
| Pei, et al. 1994 [19] | MA | GB, BL | NA | GB 34, BL 40, BL 54, BL 60, Ashi points |
| Wehling, et al. 1997 [53] | MA | NA | NA | NA |
| Wang, et al. 2003 [22] | MA | BL | Both | GB 20, BL 2, |
| Tang, et al. 2007 [23] | MA, catguts | GB, BL | NA | GB 30, BL 36, BL 54, BL 57, Ashi points |
| Wang, et al. 2009 [48] | EA | GB, BL | NA | BL 24, BL 25, BL 26 |
| Chen, et al. 2009 [43] | MA | GB, BL | NA | GB 30, BL 23, BL 25, BL 40, BL 60, |
| Zhao, et al. 2011 [42] | MA | GB, BL | affected side | GB 30, GB 34, BL 37, BL 40, BL 57, BL 58, BL 60, |
| Lee, et al. 2015 [44] | MA | GB, BL | affected side | GB 30, GB 34, BL 23, BL 25, BL 40, |
BL: bladder meridian, GB: gall bladder meridian
Table 2: Summary of reviewed studies of meridians, acupoints, and lateralization.
Discussion
▪ Meridians and lateralization
Acupuncture has been practiced to treat various diseases for over 2000 years in China; the strategy for treatment is based on the meridian selection and the choice of which acupoints to focus on along the meridian. The therapeutic effects of the selection of specific meridians and acupoints on certain diseases have been confirmed through recent studies [36-41]. However, scant randomized controlled clinical trials have been conducted to study acupuncture as a treatment for sciatica. Sporadic observational studies and expert opinions were reviewed in this study. Table 1 outlines some observational and a few clinical trials about acupuncture treatment for sciatica.
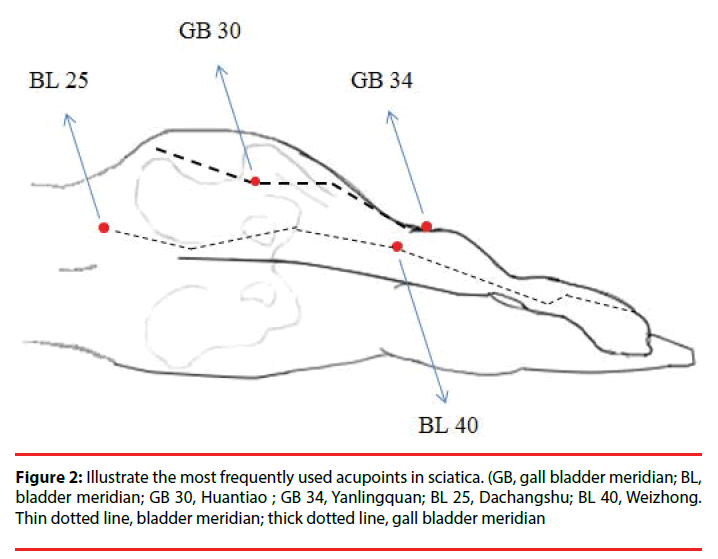
Sciatica in ancient China might be compatible with the description in ancient Chinese medicine of “ frank and leg pain “ or “arthromyodynia,” which means that people think of this disease as caused by waist sprain, strain, trauma, and other injuries of the resulting Qi–blood stasis [42]. Jing Yue Quan Shu said “Bi means closed, with Qi and blood restricted by evil Qi and not being allowed to pass, thus producing pain”. Some acupuncturists consider the foot Shaoyang gall bladder meridian (GB) and the foot Taiyang bladder meridian (BL) as the major meridians for treating sciatica, because both meridians are distributed along the sciatica dermatome. Almost all of the discussed observational studies have selected the BL and GB meridians for treating sciatica [23,42-44]. Zhang claimed that the acupoints for treating sciatica should be selected mainly in the lumbosacral region to promote the free flow of Qi and blood by removing blood stasis from the channels and collaterals and to induce diuresis to alleviate edema and stop pain [45]. Acupoint of Dachangshu (BL 25) at the level of the lower border of the spinal process of the 4th lumbar vertebrae with 1.5 cun lateral to GV meridian, might be considered as a local acupoint in treating pathological change in the lumbar vertebrae [46]. Wang, et al. used Zanzhu (BL 2) and Fengchi (GB 20) in an attempt to regulate the Qi in these two meridians, and this partially alleviated patients’ sciatica [22]. Zhao, et al. attempted to treat sciatica by using proximal needling at the Huantiao (GB 30) and obtained a rapid and obvious therapeutic effect on sciatica [42]. In addition to the BL and GB meridians, the Governor Vessel (GV) meridian governs the collateral channel, whereas the kidney meridian (KI) dominates the bone, and as we know from western medicine that sciatica mainly results from intervertebral disc lesions. Therefore, the KI, GV, and BL meridians should never be ignored when applying traditional Chinese medicine to treating sciatica [47]. Figure 2 depicts the most used acupoints BL 25, BL 40, GB 30 and GB 34 in sciatica treatment (based on http://www. zentofitness.com/lower-extremity-acupuncturepoints). One observational study mentioned the thought of lateralization. This means sciatic pain on one side of leg revealed that the cause of pain is on the same side of body. Another study considered treatment by using both sides of the meridian, regardless of the affected side. Three studies have focused on treating sciatica in the affected side of one leg or both legs [42,44,45]. Manual acupuncture was performed in all but 2 of the studies surveyed. For example, Duplan, et al. treated acute sciatica with 5 sessions of electroacupuncture and achieved a significant improvement compared with the results from a placebo group [48]; Wang, et al. reported that the therapeutic effect of electroacupuncture on senile radical sciatica was significantly more favorable than that of transcutaneous electrical nerve stimulation [49].
▪ Acupoints selection and dosage differences
The Basic Research on Acupoint Specificity Based on Clinical Efficacy Report was approved by the Chinese government in 2006, and concluded that each acupoint has its specificity and features meridian-propagated, persistent, and conditional treatment effects [50]. In the treatment of sciatica, the ideal choices of acupoints have been identified as Shenshu (BL 23) and Yaoyangguan (GV 3) for the promotion of blood circulation and tonification of the Kidney Qi; Huantiao (GB 30), Fengshi (GB 31), Yanlingquan (GB 34), and Xuanzhong (GB 39) for the promotion of free flow in the channels and collaterals to stop pain; Weizhong (BL 40) for the alleviation of waist and back pain; and Taixi (KI 3) for the enhancement of the tonification of the KI [23,43,45,47,51]. The use of Ashi point was proposed as an effective treatment method in only one study [23]. A summary of recruited studies on acupuncture for treating sciatica is provided in Table 2.
In general, the dose–effect relationship of acupuncture comprises the 3 components, namely depth, intensity of stimuli, and treatment-repeat time interval [50,52]. In recent years, a study applied functional brain MRI scans to investigate acupuncture treatment in knee osteoarthritis. The author assigned 6 acupoints to a high-dose acupuncture group and 2 to a low-dose acupuncture group. Although acupuncture might achieve its therapeutic effect on knee osteoarthritis pain by preventing cortical thinning, no difference in clinical outcome was observed between the high-dose and low-dose acupuncture groups [53]. In addition to dose difference, the combination of acupoints is an essential element in acupuncture treatment strategies. A synergistic effect can be obtained through applying an appropriate combination of acupoints; however, an inappropriate combination can result in an antagonistic effect [50]. In conclusion, for treating sciatica, it is better to choose the BL and GB meridians, with the GV and KI meridians as possible additions to nourish the patient’s Qi [54].
▪ Current therapeutic effectiveness
Acupuncture therapy was introduced to American medicine in 1972. A relatively large study (328 patients), which discussed the clinical response of various diseases to acupuncture treatment, including lumbar pain with radiation and isolated sciatica, was published in 1975 [55]. The study obtained satisfactory responses from approximately 60% of patients for a 3-week treatment duration without any complications. However, even after 40 years, the efficacy of acupuncture for treating sciatica is still considered to be uncertain [2,14,24]. Ernst et al. overviewed systematic reviews of acupuncture treatment for rheumatic pain syndrome and concluded that evidence sufficiently supported by acupuncture therapy was for only osteoarthritis, lower back pain, and lateral elbow pain [56]. Notably, two recent systemic review and meta-analysis studies have assessed current evidence on the effectiveness of acupuncture for treating sciatica. First is Ji, et al. they comprehensively searched 8 databases for studies published until April 2015, surveying a total of 12 studies involving 1842 participants; they concluded that acupuncture was more effective than conventional Western medicine in terms of outcome effectiveness (RR 1.21, 95% CI: 1.16–1.25) [57]. Second is Qin, et al. they investigated a total of 11 randomized controlled trials and determined that the use of acupuncture was more effective than drugs and may enhance the effect of drugs for patients with sciatica. However, because of the insufficient number of relevant and rigorous studies, the evidence is limited [58].
Conclusions
Acupuncture can be used to treat various diseases; however, sufficient evidence to support the clinical efficacy of acupuncture is lacking. Nevertheless, numerous observational studies have revealed therapeutic benefits of acupuncture in sciatica treatment, highlighting the strategy of concentrating on the BL and GB meridians. In the future, a series of larger randomized controlled trials using rigorous methodology, appropriate treatment sessions, and clinically relevant outcomes should be performed.
References
- Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. N. Eng. J. Med 356(22), 2245-2256 (2007)
- Valat JP, Genevay S, Marty M, et al. Sciatica. Best pract. Res. Clin. Rheumatol 24(2), 241-252 (2010).
- van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in The Netherlands. Pain 62(2), 233-240 (1995).
- Konstantinou K, Dunn KM. Sciatica: review of epidemiological studies and prevalence estimates. Spine 33(22), 2464-2472 (2008).
- Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ (Clinical research ed) 334(7607), 1313-1317 (2007).
- Golob AL, Wipf JE. Low back pain. Med. Clin. North America 98(3), 405-428 (2014).
- Vroomen PC, de Krom MC, Wilmink JT, et al. Lack of effectiveness of bed rest for sciatica. N. Eng. J. Med 340(6), 418-423 (1999).
- Atlas SJ, Nardin RA. Evaluation and treatment of low back pain: an evidence-based approach to clinical care. Muscle & nerve 27(3), 265-284 (2003).
- el Barzouhi A, Vleggeert-Lankamp CL, Lycklama a Nijeholt GJ, et al. Magnetic resonance imaging in follow-up assessment of sciatica. N. Eng. J. Med 368(11), 999-1007 (2013).
- el Barzouhi A, Vleggeert-Lankamp CL, Lycklama a Nijeholt GJ, et al. Influence of low back pain and prognostic value of MRI in sciatica patients in relation to back pain. PLoS. one 9(3), e90800 (2014).
- Zhang YG, Sun Z, Zhang Z, et al. Risk factors for lumbar intervertebral disc herniation in Chinese population: a case-control study. Spine 34(25), E918-22 (2009).
- Hagen KB, Hilde G, Jamtvedt G, et al. Withdrawn: Bed rest for acute low-back pain and sciatica. Coch. Database. Syst. Rev 2010(6), Cd001254 (2010).
- Pinto RZ, Maher CG, Ferreira ML, et al. Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ (Clinical research ed) 344(1), e497 (2012).
- Lewis RA, Williams NH, Sutton AJ, et al. Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. Spine. J 15(6), 1461-1477 (2015).
- Jacobs WC, Arts MP, van Tulder MW, et al. Surgical techniques for sciatica due to herniated disc, a systematic review. Eur. Spine. J 21(11), 2232-2251 (2012).
- Qi LY, Duan SJ, Liao WJ. Acupuncture treatment of sciatica and a preliminary study of the analgesic mechanism. J. Tradition. Chinese. Med 5(3), 179-184 (1985).
- Jiang YG, Mu JS, Zhang XY, et al. Clinical observation on acupuncture treatment of 106 cases of trunk-sciatica. J. Tradition. Chinese. Med 4(3), 183-185 (1984).
- Li Q, Lu S, Luo JM, et al. An observation on the therapeutic effect of acupuncture in the treatment of sciatica. J. Tradition. Chinese. Med 9(2), 90-92 (1989).
- Pei J. Treatment of sciatica by acupuncture at jiaji points-a report of 168 cases. J. Tradition. Chinese. Med 14(4), 266-268 (1994).
- Chu Z, Bai D. Clinical observation of therapeutic effects of wrist-ankle acupuncture in 88 cases of sciatica. J. Tradition. Chinese. Med 17(4), 280-281 (1997).
- Xu M, Chen W. One hundred cases of sciatica treated by surrounding puncture. J. Tradition. Chinese. Med 20(2), 128-129 (2000).
- Wang C, Ma J, Xiao L. Treatment of 50 cases of sciatica by needling zanzhu and fengchi. J. Tradition. Chinese. Med 23(1), 51-52 (2003).
- Tang J, Liao L. Seventy-two cases of sciatica treated by catgut point-embedding therapy. J. Tradition. Chinese. Med 27(1), 28-30 (2007).
- Ropper AH, Zafonte RD. Sciatica. N. Eng. J. Med 372(13), 1240-1248 (2015).
- Goulden EA. The Treatment of Sciatica by Galvanic Acupuncture. Br. Med. J 1(3145), 523-524 (1921).
- Wolffenbuttel E. An improvised apparatus for acupuncture in therapy of sciatica. Revista. Brasileira. de medicina 14(10), 759-760 (1957).
- Domogarova OV. Experience with the use of acupuncture in chronic recurrent neuralgia (neuritis) of the trigeminal nerve. Voprosy. Psikhiatrii. i nevropatologii 7(1), 268-273 (1961).
- Veith I. Acupuncture in traditional Chinese medicine. An Historical review. California. Med 118(2), 70-79 (1973).
- Editorial: Does acupuncture work? Can. Med. Assoc. J 110(3), 257 (1974).
- Lehrnbecher W, Bischko J. Letter: Acupuncture. Can. Med. Assoc. J 111(3), 213-passim (1974).
- Yamauchi N. The results of therapeutic acupuncture in a pain clinic. Can. Anaesthetists' Soc. J 23(2), 196-206 (1976).
- Kwasucki J, Zaleska B, Gierczak J. Modified acupuncture in the treatment of pain. Neurologia. i neurochirurgia. polska 12(3), 229-234 (1978).
- Collier BB. Treatment for lumbar sciatic pain in posterior articular lumbar joint syndrome. Anaesthesia 34(2), 202-209 (1979).
- Wu GC, Cao XD. History and causes of acupuncture advancing towards the world. J. Tradition. Chinese. Med 1(4), 247-251 (2003).
- Xie ZF. Summary of conference on homonization of traditional Chinese medicine and modern medicine held by WHO for the 2nd time. Tradition. Chinese. Med 23(12), 950-951 (2003).
- Linde K, Streng A, Jurgens S, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA 293(17), 2118-2125 (2005).
- Assefi NP, Sherman KJ, Jacobsen C, et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann. Internal. Med 143(1), 10-19 (2005).
- Foster NE, Thomas E, Barlas P, et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. BMJ (Clinical research ed) 335(7617), 436 (2007).
- Li Y, Liang F, Yang X, et al. Acupuncture for treating acute attacks of migraine: a randomized controlled trial. Headache 49(6), 805-816 (2009).
- Liu CZ, Xie JP, Wang LP, et al. Immediate analgesia effect of single point acupuncture in primary dysmenorrhea: a randomized controlled trial. Pain. Med (Malden, Mass) 12(2), 300-307 (2011).
- Zeng F, Qin W, Ma T, et al. Influence of acupuncture treatment on cerebral activity in functional dyspepsia patients and its relationship with efficacy. Am. J. Gastroenterol 107(8):1236-47 (2012).
- Zhao Y, Wang GL. Randomized controlled study on proximal needling for sciatica. Chin. Acupuncture. Moxibustion 31(5), 425-42 (2011).
- Chen MR, Wang P, Cheng G, et al. The warming acupuncture for treatment of sciatica in 30 cases. J. Tradition. Chinese. Med 29(1), 50-53 (2009).
- Lee J, Shin JS, Lee YJ, et al. Effects of Shinbaro pharmacopuncture in sciatic pain patients with lumbar disc herniation: study protocol for a randomized controlled trial. Trials 16(1), 455 (2015).
- Zhang P. Essentials for the acupuncture treatment of radicular sciatica. J. Tradition. Chinese. Med 23(3), 237 (2003).
- Yuan Q LG. Chinese-English Explanation of Jin’3 Needle Technique. Shanghai: Shanghai Scientific & Technologic Literature Publishing House, China (2004).
- Hu J. Acupuncture treatment of sciatica. J. Tradition. Chinese. Med 20(4), 314-316 (2000).
- Duplan B, Cabanel G, Piton JL, et al. Acupuncture and sciatica in the acute phase. Double-blind study of 30 cases. La semaine des hopitaux : organe fonde par l'Association d'enseignement medical des hopitaux de Paris 59(45), 3109-3114 (1983).
- Wang ZX. Clinical observation on electroacupuncture at acupoints for treatment of senile radical sciatica. Chin. Acupuncture. Moxibustion 29(2), 126-128 (2009).
- Zhao L, Chen J, Liu C-Z, et al. A Review of Acupoint Specificity Research in China: Status Quo and Prospects. Evid. Complement. Alternat. Med 2012(1), 16 (2012).
- Chen MR, Wang P, Cheng G, et al. Effect of warming needle moxibustion on pain threshold in the patient of sciatica. Chin. Acupuncture. Moxibustion 25(12), 831-833 (2005).
- White A, Cummings M, Barlas P, et al. Defining an adequate dose of acupuncture using a neurophysiological approach-a narrative review of the literature. Acupuncture in medicine. J. Br. Med. Acupunct. Soc 26(2), 111-120 (2008).
- Chen X, Spaeth RB, Retzepi K, et al. Acupuncture modulates cortical thickness and functional connectivity in knee osteoarthritis patients. Scientific. Rep 4(1), 6482 (2014).
- Leung SJ. Acupuncture treatment for pain syndrome. I. Treatment for sciatica (report on 90 cases). Am. J. Chinese. Med 1(2), 317-326 (1973).
- Domzal T, Kwasucki J, Zaleska B. Acupuncture in headache and radicular syndromes. Neurologia. i. neurochirurgia. polska 14(3), 259-262 (1980).
- Ernst E, Lee MS. Acupuncture for rheumatic conditions: an overview of systematic reviews. Rheumatology (Oxford, England) 49(10), 1957-1961 (2010).
- Ji M, Wang X, Chen M, et al. The Efficacy of Acupuncture for the Treatment of Sciatica: A Systematic Review and Meta-Analysis. eCAM 2015 192808 (2015).
- Qin Z, Liu X, Wu J, et al. Effectiveness of Acupuncture for Treating Sciatica: A Systematic Review and Meta-Analysis. eCAM 2015 425108 (2015).