Case Report - Interventional Cardiology (2022) Volume 14, Issue 3
Therapeutic management of VA-ECMO support for cardiogenic shock: Two case reports
- Corresponding Author:
- Hongfeng Yang
Department of Intensive Care Unit, Affiliated People’s Hospital of Jiangsu University, Zhenjiang, China,
E-mail: feng102220@163.com
Received date: 13-Apr-2022, Manuscript No. FMIC-22-60605; Editor assigned: 15-Apr-2022, PreQC No. FMIC-22-60605 (PQ); Reviewed date: 02-May-2022, QC No. FMIC-22-60605; Revised date: 09-May-2022, Manuscript No. FMIC-22-60605 (R); Published date: 16-May-2022, DOI: 10.37532/1755-5310.2022.14(3).501
Abstract
Introduction: Cardiogenic shock is considered a serious stage of heart disease, and there is no better way to treat this. Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO) is a well-established technology that can be used as potential life-saving measures in patients who present with cardiac arrest or severe hemodynamic instability by improving organ perfusion and oxygenation. However, it is usually complex and needs individualized decisions in a multidisciplinary approach to manage patients receiving extracorporeal membrane oxygenation, as defined clinical condition’s protocols are still lacking.
Case presentation: One patient was a 44-year-old man with out-of-hospital ventricular fibrillation was transferred to our hospital after initial cardiopulmonary resuscitation. In the emergency department, he presented with ST-segment elevation extensive anterior wall myocardial infarction and cardiogenic shock with paroxysmal ventricular tachycardia. After transfer to intensive care unit, VA-ECMO was implanted due to worsening cardiogenic shock and recovered slowly thereafter. Another patient was a 58-year-old woman presented refractory hypotension. As a bridge-therapy, VA-ECMO support was implanted and then the patient was taken to the cardiac catheterization laboratory where she experienced Percutaneous Coronary Intervention (PCI) and implanted a drug-eluting stent in the right coronary artery. Due to acute kidney injury, continuous renal replacement therapy was given to facilitate the control of fluid access balance, the removal of inflammatory media.
Conclusion: VA-ECMO is not only used as a temporary treatment strategy for cardiogenic shock, but also as a bridge-therapy. It is important to focus on improve the success rate of VA-ECMO treatment and avoid complications.
Keywords
Cardiogenic shock • Extracorporeal membrane oxygenation • Continuous renal replacement therapy
Abbreviations
VA-ECMO: Veno-Arterial Extracorporeal Membrane Oxygenation; CRRT: Continuous Renal Replacement Therapy; ROSC: Return Of Spontaneous Circulation; PEEP: Positive End Expiratory Pressure; ELSO: The Extracorporeal Life Support Organization; APTT: Activated Partial Thromboplastin Time; LVEF: Left Ventricular Ejection Fraction
Introduction
Cardiogenic shock, a life-threating state of low cardiac output with systemic hypoperfusion, is often related to myocardial infarction, refractory arrhythmia or acute myocarditis, which often require maximal doses of an inotrope medication and optimal loading [1]. The management of cardiogenic shock has long been and is still a challenging issue. As a rescue maneuver, Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO) can supply circulatory support for patients with cardiogenic shock [2]. However, it is usually complex and needs individualized decision-making in a multidisciplinary approach to manage patients undergoing ECMO, as defined clinical condition’s protocols are still lacking. Here, we presented two cases of cardiogenic shock secondary to acute myocardial infarction and chronic total occlusion of coronary artery, respectively. Both patients recovered with favorable outcome via VA-ECMO support.
Cases Presentation
Clinical data
Case 1: A 45-year-old male experienced retrosternal compression pain with radiation to the back, and then lost consciousness. Immediately, the patient was performed chest compressions and transported to our emergency room by ambulance. The patient had any conventional cardiovascular risk factor (smoking, high cholesterol and obese). A physical exam showed an unconsciousness, disappearance of aortic fluctuations and unresponsive dilated pupils, and then advanced cardiovascular life support continued. Electrocardiogram showed ST-segment over the extensive frontal wall (V1-V5); And biochemical indices (CK-MB, TnI) was in accordance with acute myocardial infarction. After 45 min of cardiac massage, Return Of Spontaneous Circulation (ROSC) occurred. The patient needed vasoactive therapy and expansive fluid volume substitution in post cardiac arrest syndrome after transfer to our department. After evaluation, he was connected to VA-ECMO (Femoro-femoral) within 45 min in the ward upon arrival. Furthermore, mild therapeutic hypothermia (34-36℃) was applied to the patient. Within the first day, the clinic status of patient ameliorated significantly with improvement of blood pressure. And then the blood lactate level gradually decreased. VAECMO was successfully weaned on hospital day 3. The patient’s cardiovascular status remained stable and he was pain-free. On hospital 10 days, he was transferred to department of cardiology and discharged after 15 days in hospital (Figure 1).
Figure 1: Blood pressure, heart rate and pulse oximetry were significantly improved in patients with acute myocardial infarction after ECPR was administered.
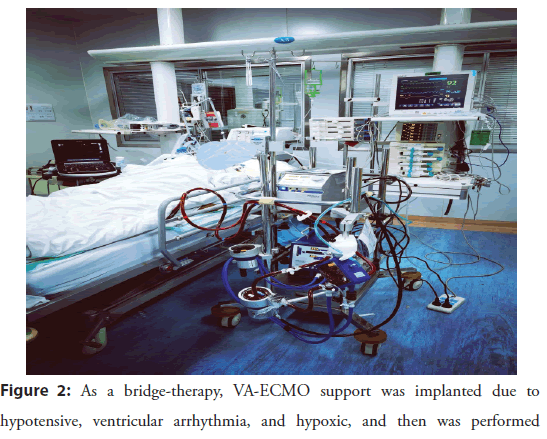
Case 2: a 58-year-old woman, admitted to hospital with a chief complaint of “Palpitation, syncope”. She had a medical history of diabetes mellitus, hypertension, and documented implant of drug stent in the right coronary artery. In addition, ICD was implanted due to reduced Left Ventricular Function (LVEF 35%). Vital signs and lung examination was normal. Heart auscultation revealed a regular cardiac rhythm with murmurs. ECG showed sinus tachycardia accompanied occasional premature ventricular beats. During hospitalization, she had a recurrent ventricular arrhythmic (ventricular arrhythmia storms) and required electrical defibrillations, even injected anti-arrhythmic drugs (amiodarone, propatonone, and lidocaine). In addition, her blood pressure needed to be maintained by norepinephrine intravenously. Thus, she underwent intubation. At present, with hypotensive, ventricular arrhythmia, and hypoxic, it was necessary to perform coronary angiography. As a bridge-therapy, VA-ECMO support was implanted, and then she was taken to the cardiac catheterization laboratory and implanted a drug-eluting stent in the right coronary artery due to totally occlusion of proximal right coronary artery. Continuous Renal Replacement Therapy (CRRT) was attributed to acute renal failure. Accompanied with normalization of conduction and improvement of blood pressure, the clinic status ameliorated. After evaluation, VA-ECMO was weaned successfully on hospital day 5. On day 16, the patient was transferred to the Department of Cardiology and discharged after 30 days in hospital (Figure 2).
ECMO management
(1) The use of VA-ECMO was based on the following criteria: Refractory cardiogenic shock in the setting of maximum inotropic support (dobutamine >15 mg/kg/min with norepinephrine >0.2 mg/kg/min); recurrent of witnessed cardiac arrest with successful cardiopulmonary resuscitation; (2) Before cannulation, a prophylactically 6-Fr catheter (TERUMO 6Fr, Radifocus, Inc., Japan) were implanted to ensure the anterograde perfusion of lower extremities and the cannulas were strengthened with reinforced purse-string sutures; (3) A continuously intravenous heparin was administrated to achieve an activated partial thromboplastin time (50-70 s); (4) During VA-ECMO support, a protective lung ventilation strategy established with a plateau pressure of less than 25 cm H2O and/or a maximum PEEP of 12 cm H2O [3]; (5) Bedside transthoracic ultrasound was performed daily to evaluate aortic valve opening, biventricular function, right ventricular unloading and left ventricular distension, and inferior vena cava; (6) The weaning criteria include: LVEF ≥ 35% with an aortic time–velocity integral >10 cm, absence of left heart distension, central venous oxygen saturation ≥ 70%, blood lactate levels<1.5 mmol/L, and urine output ≥ 0.5 ml/kg/h.
Results and Discussion
Cardiogenic shock is usually caused by acute myocardial infarction, acute myocarditis, refractory arrhythmias, or cardiac allograft dysfunction. Because medical therapy may be insufficient to overcome the extent and progression of acute heart failure, mechanical circulatory support is strongly recommended in the presence of Refractory Cardiogenic Shock (RCS). In temporary mechanical circulatory support systems, VA-ECMO is increasingly employed in patients with acutely cardiac dysfunction due to pulmonary and biventricular support. In particular, VA-ECMO is used to bridge the first critical days until the patient recovers or establishes target therapy.
First, careful attention should be paid to the VA-ECMO and ventilator setting. For a set pump flow rate, the primary determinants of inflow are the size of the venous cannula and blood volume. And the position of the tip of venous cannula in the right atrium is optimal. Likewise, it is important to highlight the interactions between VA-ECMO and mechanical ventilation. Because heart failure patients receiving VA-ECMO often have abnormal lung function. Although the Extracorporeal Life Support Organization (ELSO) suggested that higher PEEP levels may be more appropriate if increased alveolar strain and alveolar over-distension are considered [4], higher PEEP may affect left and right ventricular load in VA-ECMO and then reduce cardiac output [5,6]. Therefore, with frequent cardiac echography monitoring, we believe that a PEEP levels of less than 12 cm H2O is recommended. Second, Haemorrhage is well-documented and this risk may be attributed to heparin bolus, cannulation strategy, patient variables [7-9]. However, the optimal anticoagulation strategy for ECMO has not been established. Compared with the higher APTT target, lower APTT target appeared to have less bleeding but similar thromboembolic events [9]. Therefore, we adopted a conservative anticoagulation initiation (60 u/ kg) and therapeutic range (maintaining APTT between 1.5-2.0 times normal). At least, lower anticoagulation target may be appropriate for shorter VA-ECMO runs (3 days and 5 days of VA-ECMO support respectively, in both cases). Another dreadful complication of VA-ECMO treatment is distal limb ischemia. Almost 20% of peripheral VA-ECMO patients have some degree of distal limb ischaemia. Thus, placement of reperfusion catheter in the ipsilateral superficial femoral artery is recommended [10]. In conclusion, as the use of VA-ECMO increases, future studies are urgently needed to determine best practice for ECMO and its impact on patient-centered outcomes.
Conclusion
VA-ECMO is not only used as a temporary treatment strategy for cardiogenic shock, but also as a bridging therapy. ECMO support is an appropriate technique for the short-term treatment of refractory low cardiac output after surgery, despites its complications. With the increasing use of VA-ECMO, it is important to focus on the improve the success rate of VA-ECMO treatment and avoid complications.
Acknowledgments
Not applicable.
Authors’ Contributions
HFY wrote the manuscript, while JY performed the literature search. ZCJ reviewed the case and provided insightful additions to the case presentation. All authors read and approved the final manuscript.
Funding
Zhenjiang Social Development R&D Program (SH2019066).
Availability of Data and Materials
Please contact author for data requests.
Ethics approval and consent to participate
Not applicable.
Competing Interests
All the authors declare that they have no conflicts of interest.
References
- Berg DD, Bohula EA, van Diepen S, et al. Epidemiology of shock in contemporary cardiac intensive care units. Circ Cardiovasc Qual Outcomes. 12(3): e005618 (2019).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Rao P, Khalpey Z, Smith R, et al. Venoarterial extracorporeal membrane oxygenation for cardiogenic shock and cardiac arrest. Cardinal considerations for initiation and management. Circ Heart Fail. 11(9): e004905 (2018).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Singh G, Hudson D, Shaw A. Medical optimization and liberation of adult patients from VA-ECMO. Can J Cardiol. 36(2): 280-290 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Dembinski R, Hochhausen N, Terbeck S, et al. Pumpless extracorporeal lung assist for protective mechanical ventilation in experimental lung injury. Critical Care Medicine. 35(10): 2359-2366 (2007).
[CrossRef] [Google Scholar] [PubMed]
- Zhou L, Cai G, Xu Z, et al. High positive end expiratory pressure levels affect hemodynamics in elderly patients with hypertension admitted to the intensive care unit: A prospective cohort study. BMC Pulm Med. 19(1): 224 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Pinsky MR. Cardiopulmonary interactions: Physiologic basis and clinical applications. Ann Am Thorac Soc. 15(Suppl 1): S45-S48 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Berg DD, Barnett CF, Kenigsberg BB, et al. Clinical practice patterns in temporary mechanical circulatory support for shock in the critical care cardiology trials network (CCCTN) registry. Circ Heart Fail. 12(11): e006635 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Tsangaris A, Alexy T, Kalra R, et al. Overview of Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO) support for the management of cardiogenic shock. Front Cardiovasc Med. 8: 686558 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Sy E, Sklar MC, Lequier L, et al. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: A systematic review and meta-analysis. J Crit Care. 39: 87-96 (2017).
[CrossRef] [Google Scholar] [PubMed]
- Foley PJ, Morris RJ, Woo EY, et al. Limb ischemia during femoral cannulation for cardiopulmonary support. J Vasc Surg. 52(4): 850-853 (2010).
[CrossRef] [Google Scholar] (All versions) [PubMed]