Case Report - International Journal of Clinical Rheumatology (2020) Volume 15, Issue 4
Think out of the box! Pediatric onset adult Sarcoidosis in a young child presenting as Pyrexia of unknown origin
- Corresponding Author:
- Sagar Bhattad
Department of Pediatrics
Aster CMI Hospital, Bangalore, India
E-mail: drsagarbhattad@gmail.com
Abstract
Sarcoidosis is a rare multi-systemic granulomatous disease that can have myriad of presentations in childhood. A five-year old female child presented with recurrent fever from two years of age and hepato-splenomegaly. She had no arthritis, rash or uveitis. She had been extensively investigated and yet, remained undiagnosed for a period of three years. Finally, a liver and lymph node biopsy yielded the diagnosis of sarcoidosis. In children presenting with pyrexia of unknown origin (PUO), when a thorough history, physical examination and initial investigations fail to provide direction, tissue biopsy must be considered. To the best of our knowledge, this is the first report of pediatric-onset adult sarcoidosis presenting at such a young age, from the Indian subcontinent. It aptly high-lights the need to consider sarcoidosis as a possibility in children presenting with PUO.
Keywords
rsarcoidosis • pediatric sarcoidosis • pyrexia of unknown origin
Introduction
Pediatric sarcoidosis is a rare disease characterized by presence of non-caseating granulomas in a variety of tissues and organ systems. The diagnosis of sarcoidosis in children is often delayed be-cause of wide variety of symptoms and a lack of awareness of the disease [1].
Case
A 5-year old female child, born of nonconsanguineous parentage, developmentally normal, presented with recurrent high grade fever for the past 3 years and abdominal distention for one year. There was no history of weight loss, rash, joint pain or swelling. She was active between periods of febrile episodes. She has been treated with several courses of antimicrobials empirically, with no relief. Six months prior, she had an episode of thrombocytopenia and was treated with Intravenous immunoglobulin (IVIg) elsewhere, considering a possibility of immune thrombocytopenia. She responded to the same and had normal platelet counts since then. Physical examination revealed a well-appearing child with normal anthropometry and mild pallor. She had hepato-splenomegaly with liver span being 13 cm and spleen enlarged 3 cm below left costal margin along the splenic axis. The remainder of the systemic examination was normal. There was no skin rash, joint swelling and ophthalmic examination ruledout uveitis.
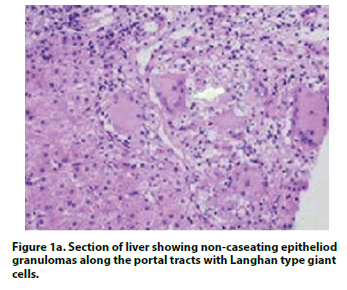
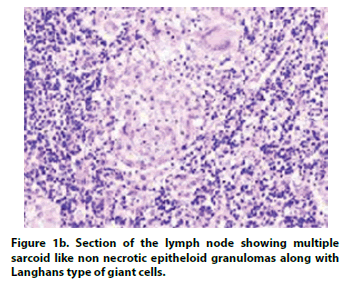
She was extensively evaluated complete blood counts, liver and renal functions were normal; blood and urine cultures were sterile. Work up for malaria, tuberculosis, brucellosis, hepatitis B, hepatitis C, Human Immunodeficiency and Epstein-Barr virus was negative. Anti-Nuclear Antibody (ANA) by immunofluorescence was negative. Serum ferritin and immunological screen (serum immunoglobulin’s, tests for chronic granulomatous disease, lymphocyte subsets) were normal. Bone marrow aspiration and biopsy excluded malignancy; and marrow cultures were sterile. Double negative T cells were within normal limits, excluding autoimmune lymphoproliferative syndrome. On further evaluation, serum Acetylcholine Esterase (ACE) was elevated (164; N:12- 68 U/L) while serum calcium was normal. Computed tomography of the thorax and abdomen (at one year of ill-ness) showed diffuse enlargement of liver with normal echo texture and normal spleen; mediastinal nodes were mildly enlarged. A liver biopsy was performed that showed epithelioid granulomas along the portal tracts with Langhans type giant cells, granulomatous hepatitis with confluent parenchymal necrosis with reparative fibrosis suggestive of sarcoidosis (Figure 1a). Left external iliac node biopsy showed multiple sarcoidlike non-necrotic epithelioid granulomas along with Langhans type of giant cells (Figure 1b). Ziehl-Neelsen staining for acid fast bacilli, gene Xpert and fungal stains of tissue biopsy were negative.
Based on the clinical presentation, evidence of granulomas on tissue biopsy and elevated ACE levels, a diagnosis of sarcoidosis was made. She was treated with oral steroids (1 mg/kg/day) along with weekly methotrexate (15 mg/ m2) to which she responded promptly and was afebrile by one week. Her liver and spleen regressed over the next 6 months. Steroids were tapered and stopped by one year. At 1.5 years of follow-up, she continues to remain well, on weekly methotrexate therapy.
Discussion
Sarcoidosis is a rare, chronic granulomatous disease with multi-systemic involvement. The incidence of sarcoidosis is estimated to be around 0.22-0.27 per 100,000 children per year in children less than 15 years [2]. There is equal incidence among male and female children [2]. Childhood sarcoidosis is divided into early onset and classical juvenile sarcoidosis [3]. Early onset sarcoidosis presents with a triad of polyarthritis, uveitis and dermatitis and is associated with the nucleotide binding oligomerization domain 2 (NOD2) mutations. Familial form of early onset sarcoidosis is called Blau syndrome. Patients without NOD2 mutation present with visceral and systemic manifestations. Based on the clinical features, they are further divided into infantileonset panniculitis with systemic granulomatosis and pediatric-onset adult sarcoidosis [4]. Index case had an onset of the disease at the age of two, but did not have rash, arthritis or uveitis. She, however, had marked visceral involvement, thus qualifying for a diagnosis of pediatric onset adult sarcoidosis.
Thrombocytopenia is reported to occur in 1%-2% of patients with sarcoidosis [5] and is secondary to autoimmunity, hypersplenism and/or bone granulomas [6]. In the index case, thrombocytopenia responded promptly to IVIg and was likely immune mediated. Hypercalcemia and elevated ACE levels are useful markers of disease activity in sarcoidosis, though they are not specific. High ACE levels have been reported between 50% to 74% of children with sarcoidosis [7,8].
Enlarged mediastinal nodes were documented at oneyear of illness in the index child. Mediastinal node biopsy, an invasive procedure, was deferred by the treating team at that point of time, as the child was well-appearing. Visceral involvement has been reported in 40% of children with sarcoido-sis [7,9]. In the index case, liver biopsy showed granulomas consistent with diagnosis of sarcoido-sis. External iliac node also showed similar findings. Average delay in the diagnosis of sarcoidosis is 1.6-2.3 years in some studies [9,10]. Our patient underwent treatment at several hospitals for the past 3 years, before an appropriate diagnosis was made. Pediatric-onset adult sarcoidosis commonly presents in older children [10] and onset of this form of disease at the age of 2, is extremely un-common.
Conclusion
We hereby emphasize the role of tissue biopsy in children with pyrexia of unknown origin and the need to consider sarcoidosis as a differential in children with prolonged unexplained fever. This, to the best of our knowledge, is the first case of pediatric onset-adult sarcoidosis reported at this age.
References
- Shetty AK, Gedalia A. Childhood sarcoidosis: A rare but fascinating disorder. Pediatr. Rheumatol. 6(1), 16 (2008).
- Hoffmann AL, Milman N, Byg KE. Childhood sarcoidosis in Denmark 1979-1994: incidence, clinical features and laboratory results at presentation in 48 children. Acta. Paediatr. 93(1), 30–36 (2004).
- Cimaz R, Ansell BM. Sarcoidosis in the pediatric age. Clin. Exp. Rheumatol. 20(2), 231–237 (2002).
- Yasemin O, Cengiz Ali B, Ali D et al. Pediatric-on-set adult type sarcoidosis: A case report. Arch. Argent. Pediatr. 113(6), e336–e340 (2015).
- Kayar Y, Kayar NB, Unver N et al. Sarcoidosis Presenting with Severe Thrombocytopenia. Int. J. Resp. Pulm. Med. 3(5), 1–3 (2016).
- Mahévas M, Chiche L, Uzunhan Y et al. Association of Sarcoidosis and Immune Thrombocytopenia: Presentation and Outcome in a Series of 20 Patients. Medicine (Baltimore). 90(4) (2011).
- Milman N, Hoffmann AL. Childhood sarcoidosis in Denmark 1979-1994: long-term follow-up of 46 children. Eur. Respir. J. (2007).
- Gedalia A, Khan TA, Shetty AK et al. Childhood sarcoidosis: Louisiana experience. Clin. Rheumatol. 35(7), 1879–1884 (2016).
- Gunathilaka PK, Mukherjee A, Jat KR et al. Clinical Profile and Outcome of Pe-diatric Sarcoidosis. Indian. Pediatr. 56(1), 37–40 (2019).
- Al-Mayouf SM, Al-Sonbul A, Al Jumaah S et al. Sarcoidosis: a delayed or missed diagnosis in children. Ann. Saudi. Med. 26(3), 220–223 (2006).