Case Report - Interventional Cardiology (2024)
Thrombus aspiration in STEMI with heavy thrombus burden
- Corresponding Author:
- Abdelaziz Ahmed Abdelaziz
Department of Cardiology, Al- Azhar University, Cairo, Egypt,
E-mail: abdelaziz_1975@yahoo.com
Received date: 23-Jul-2024, Manuscript No. FMIC-24-142999; Editor assigned: 25-Jul-2024, PreQC No. FMIC-24-142999 (PQ); Reviewed date: 14-Aug-2024, QC No. FMIC-24-142999; Revised date: 21-Aug-2024, Manuscript No. FMIC-24-142999 (R); Published date: 28-Aug-2024, ![]()
Abstract
Introduction: Thrombus Aspiration (TA) rarely improves clinical outcomes in patients who undergo primary Percutaneous Coronary Intervention (PPCI) for ST-Segment Elevation Myocardial Infarction (STEMI). However, there is some doubt regarding the prospective benefits of TA in patients with a high Thrombus Burden (TB). This case report aimed to assess the advantages of TA in a patient with high TBSTEMI.
Patient concerns: A 59-year-old male patient had typical chest pain for the past 2 hours during the night. The electrocardiogram indicates an inferior STEMI and the echocardiography results show ischemic changes and abnormal regional wall motion.
Diagnoses: The findings of the coronary angiography showed complete occlusion of the Right Coronary Artery (RCA) from its ostium.
Interventions: PPCI was performed on the RCA using the insertion of two drugeluting stents following utilizing a TA device.
Outcomes: Successful PPCI to RCA using 2 DES.
Conclusion: TA in STEMI patients with high Thrombus Burden (TB) offers a better result.
Keywords
STEMI • Thrombus aspiration • Percutaneous coronary intervention • Thrombus burden
Abbrevations
DES: Drug-Eluting Stent; ECG: Electrocardiogram; HTN: Hypertension; LAD: Left Anterior Descending Artery; LCX: Left Circumflex Artery; LM: Left Main Artery; OM: Obtuse Marginal Branches; PPCI: Primary Percutaneous Coronary Intervention; RCA: Right Coronary Artery; TB: Thrombus Burden
Introduction
ST-elevation myocardial infarction is defined by the rupture of plaque and blockage of the infarct artery by a blood clot. Primary percutaneous coronary intervention is highly successful in restoring blood flow in the infarct artery, but a major drawback is the occurrence of distal embolization of the blood clot and blockage of the small blood vessels [1].
The relationship between microvascular perfusion in STEMI, as assessed by angiographic myocardial blush grade and electrocardiographic ST-segment resolution and mortality following PPCI has been well-established. Approximately 33% of patients who have undergone PPCI experience decreased microvascular perfusion, even after normal blood flow has been restored to the heart’s outer layer. This condition is associated with a much higher death rate. Moreover, there is a direct correlation between the amount of thrombus present during PPCI and the likelihood of mortality [2].
Thrombus Aspiration (TA) is a recognized therapy choice for patients with STEMI who are having PPCI. However, recent trials have yielded unsatisfactory outcomes, showing no decrease in mortality and maybe an elevated risk of stroke. The available information is primarily limited to people who seek medical attention during the first few hours after the beginning of symptoms. However, individuals who arrive at the hospital within 12 hours after experiencing symptoms may exhibit significantly elevated TB levels due to prolonged residence durations. Therefore, trans arterial TA may serve as a valuable addition to standard PCI in this specific group of patients [3].
Data on the efficacy of TA in the subgroup of patients with STEMI presenting late after symptom onset are scarce [4]. Therefore, this case report aimed to evaluate the benefit of TA among STEMI patients with high TB.
Case Presentation
A 59-year-old Egyptian patient was transported to the cardiology department of Teachers Hospital with a sudden onset of inferior STEMI. The patient had additional medical conditions, such as hypertension, non-insulin-dependent Diabetes mellitus, dyslipidemia and a history of Coronary Artery Bypass Graft (CABG) surgery 10 years earlier. The diagnosis of the case was verified using the ECG, which indicated an elevation of the ST segment in the inferior leads. In addition, the echocardiogram revealed a RWMA characterized by a substantial decrease in movement of the inferior wall and an EF of 29%.
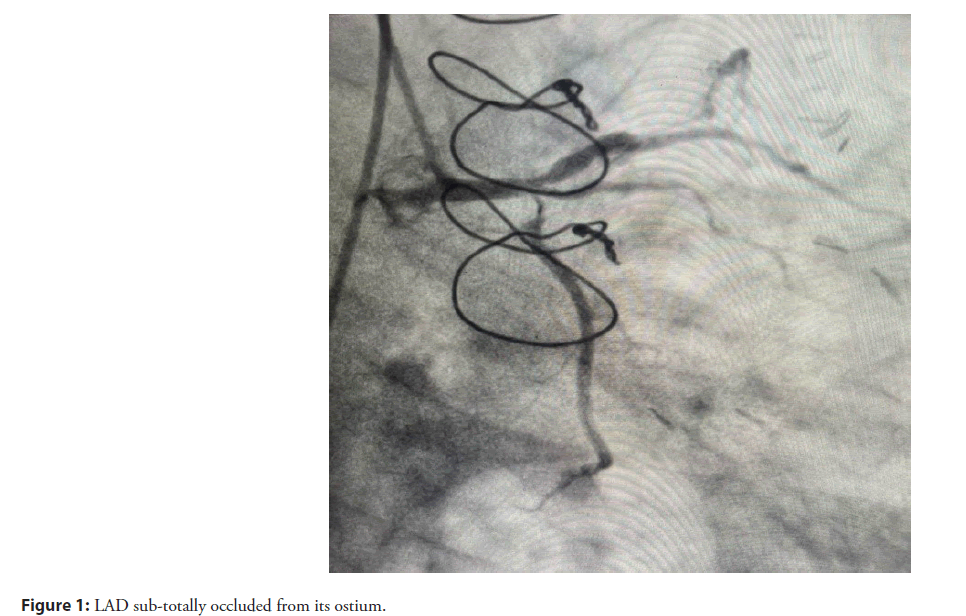
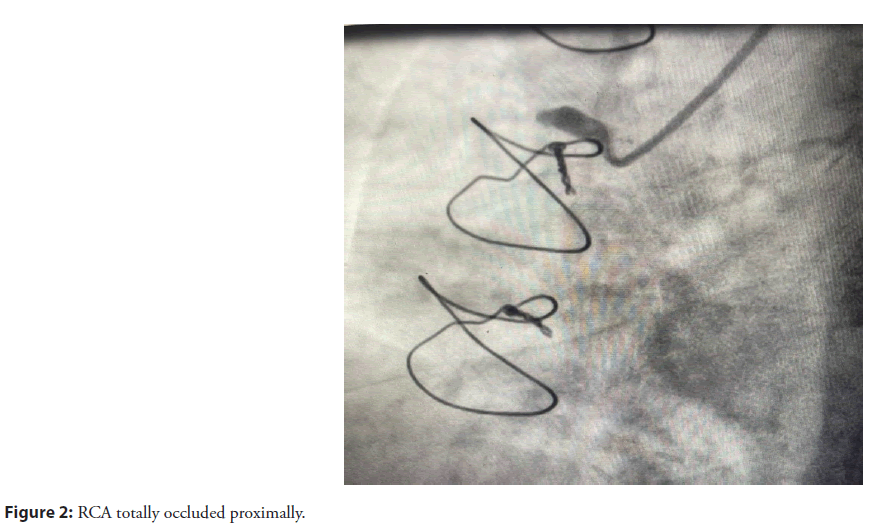
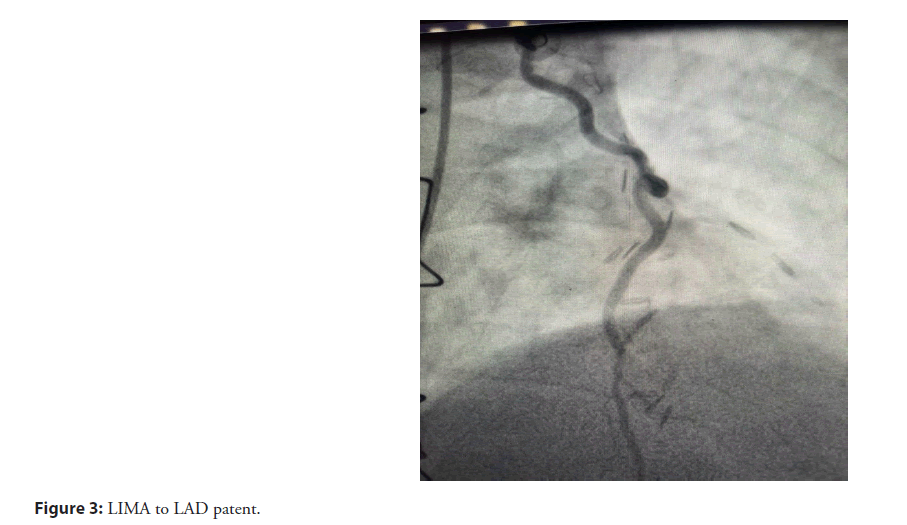
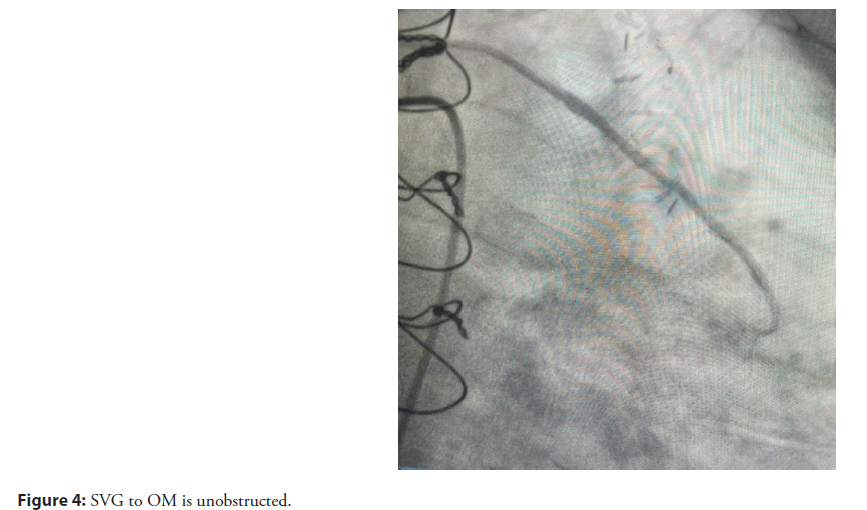
A trans-femoral technique was used to do the coronary angiography, which showed that the LM artery had a normal size and divided into the LAD and LCX arteries. The LM artery had a 50% blockage at its distal end. The LCX exhibited a near-complete blockage at its origin, while the high OM had a notable narrowing. The LAD exhibited a near-complete blockage at its origin (Figure 1). The RCA is blocked immediately after its origin (Figure 2). The Left Internal Mammary Artery (LIMA) to the mid-LAD is open and unobstructed, as shown in (Figure 3). The Saphenous Vein Graft (SVG) to the OM is unobstructed (Figure 4).
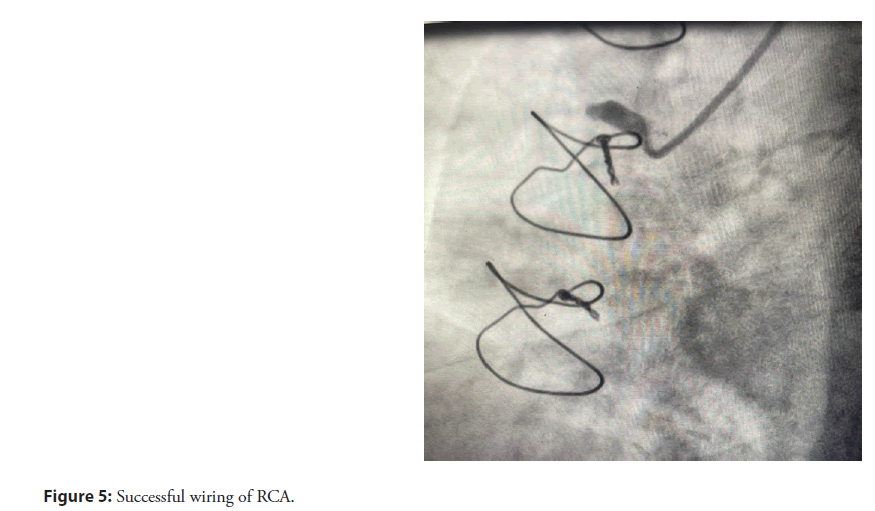
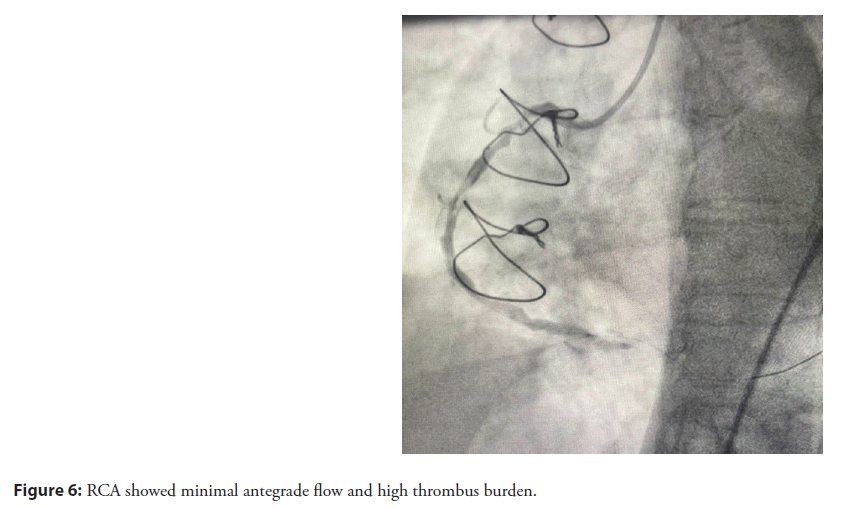
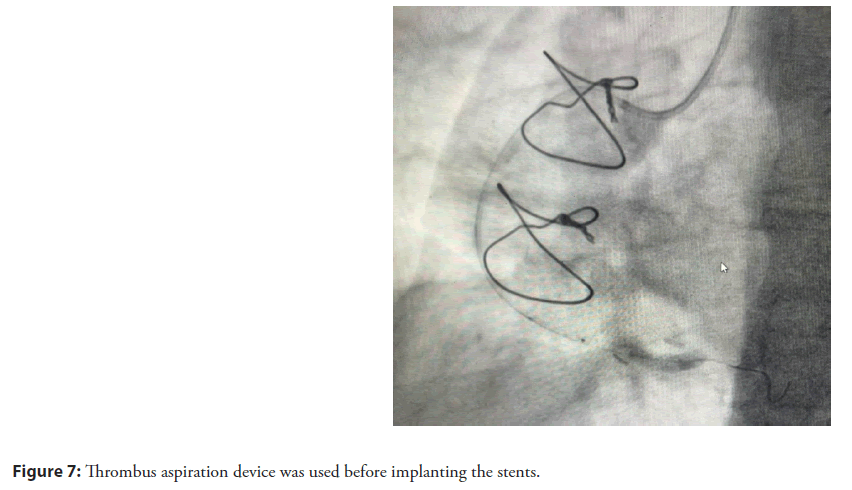
The RCA was accessed with a JR 3.5 guiding catheter. The RCA complete blockage was successfully traversed using a PT2 MS wire, which was then positioned in the distal area (Figure 5). Upon successful crossing of the wire to the lesion, the RCA exhibited weak forward flow with significant TB, indicating a lengthy lesion in the RCA (Figure 6). TA device was utilized prior to stenting the lengthy lesion in the RCA in order to reduce the occurrence of noreflow and distal embolization (Figure 7).
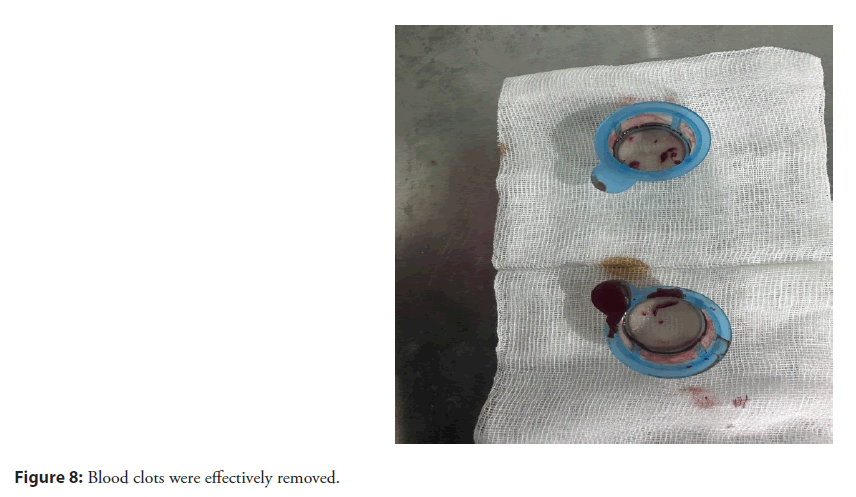
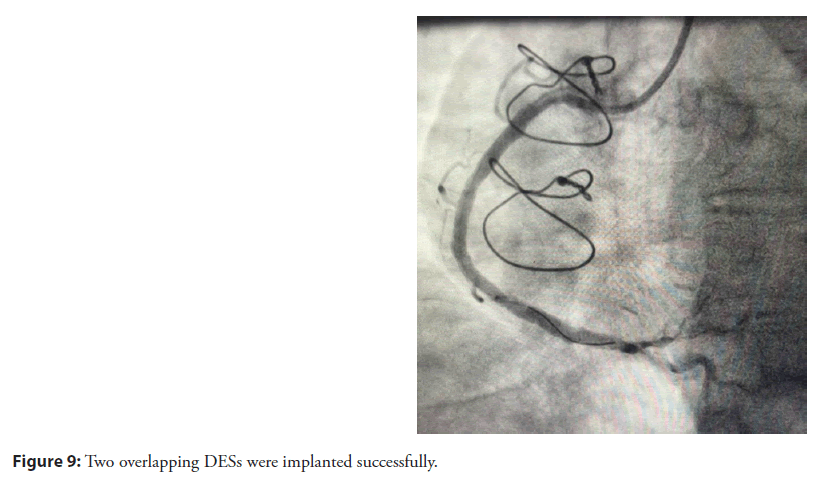
Several blood clots were effectively removed (Figure 8). Subsequently, two DES were inserted, specifically the Xience Xpedition 3 x 48 mm and Xience Xpedition 3.5 x 48 mm, with one stent placed on top of the other in an overlapping manner. Following this, a post-dilation procedure was performed using an NC Force 4 x 20 mm balloon. Ultimately, the patient departed from the catheter laboratory with an optimal TIMI III flow (Figure 9) with no complications.
The patient was followed up in the clinic with the improvement of his symptoms and the echocardiography showed improvement of his EF to 46% and mild RWMA in the inferior wall.
Results and Discussion
Over the past few years, the management of STEMI has seen significant advancements. PPCI has emerged as the preferred treatment. Nevertheless, there exist several impediments to attaining effective cardiac reperfusion. One of the prominent challenges is the presence of high TB in a substantial number of patients. Manipulating wires and dilating balloons, as well as placing stents in the affected blood vessels, can lead to the release of thrombus particles and debris from atherosclerotic plaques. This impairs the blood flow to the heart muscle, resulting in worse short-term and long-term outcomes, such as heart failure and death [5].
TA devices are highly effective tools designed to remove blood clots from the blocked artery. They are used as additional treatment to prevent the spread of blood clots to smaller blood vessels.
A prior study has shown that regular TA in patients having PPCI for STEMI does not enhance clinical outcomes. Nevertheless, there is still doubt regarding the potential advantage in patients with high TB, despite the existence of a biological reason for a bigger benefit.
Based on the reported case, the patient had a medical background of hypertension, diabetes, dyslipidemia and a prior coronary artery bypass graft CABG. The patient came with an acute inferior STEMI. The coronary angiography showed complete blockage of the RCA and almost complete blockage at the origin of the LCX and LAD. The TA and stenting procedure was carried out to treat the lesion in the RCA, which resulted in achieving optimal blood flow with a TIMI III rating. The follow-up assessment revealed an enhanced EF of 46%.
Multiple studies have failed to demonstrate a significant advantage in the regular use of MAT after initial PCI. Interestingly, aspiration thrombectomy was found to be linked with a notable decrease in cardiovascular mortality among a certain subset of patients with large TB. This implies that MAT can be considered as a viable treatment choice for certain patients. MAT, recommended by clinical guidelines, is a commonly ued procedure for thrombectomy in cases of intracoronary thrombi during AMI. However, there are few viable alternative techniques available when MAT is unsuccessful in treating AMI, despite advancements in the MAT approach [6].
TA is a conceptually attractive procedure, but its effectiveness has produced mixed findings in randomized clinical studies. As a result, this therapy is only recommended at a level IIa, with a level of evidence B, according to the European Guidelines of 2008. In the European Guidelines of 2017, it is given a class III recommendation.
Several small-scale or single-center studies, together with one metaanalysis of 11 small trials, have indicated potential advantages of implementing routine MAT during primary PCI.
Elfekky et al., study demonstrated a notable reduction in cardiovascular mortality among patients in the TA group, with only 2.7% experiencing this outcome, compared to 11.8% in the conventional PCI group [7]. There was no significant difference between the two groups in terms of additional sequelae such as stroke, non-fatal MI and target vessel revascularization.
A previous retrospective cohort study by Bin et al., reported that when comparing conventional PPCI with PPCI and TA, it was found that PPCI with TA had significant benefits for patients with STEMI and a large TB [8]. These benefits included a higher rate of achieving postprocedural TIMI 3 flow, a lower corrected thrombolysis in MI score and a larger post procedural vessel diameter. However, PPCI with TA did not reduce the risk of Major Adverse Cardiac and Cerebrovascular Events (MACCE) during the 1 yr follow-up period.
Conclusion
Thrombus aspiration in patients with high thrombus burden can decrease TB, lower rates of distal embolization, improve thrombolysis in myocardial infarctionâ3 flow, reduce the incidence of no reflow, improve microvascular perfusion and consequently improve clinical outcomes. Thrombus aspiration therapy improves outcome of PPCI in a STEMI patient with high TB without causing stroke and should be considered in selected patients with high TB. As such, routine thrombus aspiration during primary PCI is not recommended by guideline committees (class III, 2021 American College of Cardiology/American Heart Association guidelines or 2017 European Society of Cardiology guidelines) and selective or bailout use is given a class IIb recommendation only by the Japanese Cardiological Society.
References
- Takahata M, Ino Y, Kubo T, et al. Prevalence, features, and prognosis of arteryâtoâartery embolic STâsegment-elevation myocardial infarction: An optical coherence tomography study. J Am Heart Assoc. 9:e017661 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Birdal O, Topçu S, TanboÄa Ä°H, et al. The relationship between clinical outcomes and calculated thrombus burden before and after initial flow in patients with ST-segment elevation myocardial infarction. Eurasian J Med. 54(2):145 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Bianchini E, Lombardi M, Buonpane A, et al. Impact of thrombus aspiration on left ventricular remodeling and function in patients with ST-segment elevation myocardial infarction: A meta-analysis of randomized controlled trials. Int J Cardiol. 397:131590 (2024).
[CrossRef] [Google Scholar] [PubMed]
- Moxham R, Džavík V, Cairns J, et al. Association of thrombus aspiration with time and mortality among patients with ST-segment elevation myocardial infarction: A post hoc analysis of the randomized TOTAL trial. JAMA network open. 4(3):e213505 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Alyamani M, Campbell S, Navarese E, et al. Safety and efficacy of intracoronary thrombolysis as adjunctive therapy to primary PCI in STEMI: A systematic review and meta-analysis. Can J Cardiol. 37(2):339-346 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Leivo J, Anttonen E, Jolly SS, et al. The high-risk ECG pattern of ST-elevation myocardial infarction: A substudy of the randomized trial of primary PCI with or without routine manual thrombectomy (TOTAL trial). Int J Cardiol. 319:40-45 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Elfekky EM, Penjameen MN, Nassar AI, et al. Outcome of manual thrombus aspiration for patients undergoing primary PCI for acute STEMI showing large thrombus burden. Egypt Heart J. 73:1-7 (2021).
[CrossRef] [Google Scholar] [PubMed]
- Bin N, Zhang F, Song X, et al. Thrombus aspiration during primary percutaneous coronary intervention improved outcome in patients with STEMI and a large thrombus burden. J Int Med Res. 49(5):03000605211012611 (2021).
[CrossRef] [Google Scholar] [PubMed]