Research Article - Interventional Cardiology (2021)
Time to maximal vasodilator effect of intracoronary nitroglycerin administration in coronary angiography
- Corresponding Author:
- Sanitpong Fongjunsom
Department of Internal Medicine, Excellence Cardiac Center, Surin Hospital, Surin Province, Thailand
E-mail: sanitpongfongjunsom@gmail.com
Received date: May 06, 2021; Accepted date: May 20, 2021;Published date: May 27, 2021
Abstract
Background: Nitroglycerin (NTG) is frequently used to evaluate coronary vessel size from coronary angiography (CAG). However, the timing of the maximal vasodilatory effect of NTG while performing CAG is not well established. This study aims to determine the timing of the maximal vasodilatory effect of intracoronary NTG (IC NTG) administration.
Methods: This prospective study enrolled 40 consecutive patients scheduled for CAG and/or Percutaneous Coronary Intervention (PCI) in Surin hospital. Cineangiography was done and recorded as a baseline. Thereafter, 200 mcg of NTG was injected via the catheter. Interval cineangiography at 30, 60, 90, 120, and 150 seconds was performed. Hemodynamics was recorded throughout the procedure. Coronary artery size was measured by the Quantitative Coronary Analysis (QCA) method. Calibration was made by using a catheter as a reference. Measurement was done in optimal view for each part of the vessel and the frame to be measured was selected from the same phase of cardiac cycle in each patient.
Results: Coronary artery diameter was significantly increased with IC NTG. The mean time for a maximal change was 101.25 ± 31.95 seconds. The maximal increase in vessel size was 0.36 mm. (95% CI 0.29, 0.43 p<0.001). Mean aortic pressure significantly decreased after IC NTG. Mean time for maximal change of Mean Aortic Pressure (MAP) was 63.75 ± 41.99 seconds. The maximal decreased of MAP was -14.08 mmHg (95% CI-17.22, -10.93).
Conclusion: In PCI naïve coronary artery, A 200 mcg IC NTG reaching maximal vasodilatory effect around 2 minutes. MAP was significantly reduced but without clinical significance.
Keywords
Nitroglycerin • Coronary angiogram • Vasodilator • Cardiac catheterization • Quantitative Coronary Analysis (QCA)
Introduction
Nitroglycerin (NTG), a vasodilator, is well-known medication for treating angina pectoris for decades [1]. Both oral, sublingual, and intravenous forms are available. NTG widely used in cardiac catheterization laboratory when performing coronary angiography (CAG) [2] to relieve coronary vasospasm. NTG is mostly administered directly to the coronary artery because of very effective delivery method [3,4]. NTG also helpful to evaluate coronary vessel size, determine actual lesion length by ruling out vasospastic component so this can provide appropriate stent size, and avoid unnecessary Percutaneous Coronary Intervention (PCI) [5,6] because angiographic catheter itself also induced coronary spasm, especially left main [7] and ostial and proximal part of right coronary artery. However, the timing of the maximal vasodilatory effect of NTG while performing CAG is not well established. This study aims to determine the timing of the maximal vasodilatory effect of intracoronary NTG (IC NTG) administration to reduced radiation dose, time, and contrast usage while getting optimal coronary angiographic interpretation.
Methodology
Study population
This prospective single-center study was carried out at Surin Hospital, Thailand. Sample size calculation was made by using this formula

Where z1-α is 1.96 (for z score when using 95% CI)
z1-β is 0.84 (for 1-β=0.80)
ϵ is the margin of error
n is the sample size
μ is 3.39 (for the measure vessel size after NTG)
μ0 is 2 (for the baseline vessel size)
δ is 0 (for the margin)
σ is 3 (for standard deviation)
By using data from the previous study [8], the sample size will be 40 to achieved statistical power of 80%.
A total of 40 consecutive patients were scheduled for CAG and/or Percutaneous Coronary Intervention (PCI). Inclusion criteria were patients age 18-80 years who were diagnosed with Stable Coronary Artery Disease (SCAD), suspected ischemic cardiomyopathy, positive ischemia from non-invasive tests, and Non-ST elevation Acute Coronary Syndrome (NSTE-ACS). Exclusion criteria were hemodynamic unstable, currently, on intravenous inotropic drugs, Estimated glomerular filtration rate less than 30 ml/min/1.73 cm2 , presence of coronary stents in an observed vessel, received sildenafil within 24 hours, hypertrophic cardiomyopathy, recently received oral or intravenous nitrate within 12 hours and history of serious adverse event with receiving NTG or oral form nitrate. Inform consent was obtained before enrolling.
Cardiac catheterization and angiographic technique
After giving informed consent, coronary angiography was performed by one experienced interventional cardiologist. All patients were requested not to eat or drink at least 6 hours before starting the procedure. Standard preparation was done for all patients. The 5, 6, or 7 Fr. size arterial sheath was inserted via radial artery or femoral artery which depends on operator’s choice. Every patient received local anesthetized with 2% lidocaine without adrenaline. An additional 70-100 units per kilogram of heparin was administered via arterial sheath if radial approached was selected. Cine angiography was obtained and recorded by Philips Allura Xper® FD10 with multiple standard views at 7.5 frames per second or 15 frames per second if cannot obtain optimal image quality for both left coronary and right coronary artery.
Cine angiography was done and recorded as a baseline. Thereafter, 200 mcg of NTG was injected via a diagnostic catheter. Additional 3 ml of normal saline was flushed after NTG administration. Interval cine angiography at 30, 60, 90, 120, and 150 seconds was performed after NTG. Hemodynamics was recorded throughout the procedure to avoid ventricularization and change in blood pressure before and after IC NTG.
Measurement of the coronary artery
Coronary artery size was measured by the Quantitative Coronary Analysis (QCA) method that was made by an experienced interventional cardiologist. Calibration was made by using a catheter as a reference size. Measurement was done in optimal view for each part of the vessel and the frame to be measured was selected from the same phase of cardiac cycle, view, vessel segment, and length in each patient.
Statistical analysis will be made by SPSS version 17.0 (IBM). Descriptive statistics will be used to describe baseline characteristics by Mean ± SD. Statistical significant is defined with p-value <0.05
Changes in mean vessel size and mean aortic pressure between Pre and post-nitroglycerin administration will be analyzed by Paired t-test.
Results
A total of 40 consecutive patients were enrolled. All successfully followed study protocol and can be obtained optimal image quality. Baseline characteristics are described in Table 1.
| n=40 | |
|---|---|
| age(Y) | 61.78 ± 9.27 |
| Gender | |
| Female | 15 (37.5%) |
| Male | 25 (62.5%) |
| Indication for coronary angiography | |
| Suspected ischemic cardiomyopathy | 11 (27.5%) |
| Ischemia from non-invasive tests | 2 (5%) |
| NSTE-ACS | 27 (67.5%) |
| Hypertension | 20 (50%) |
| Diabetes mellitus | 7 (17.5%) |
| Hyperlipidemia | 15 (37.5%) |
| Smoking | 3 (7.5%) |
| Prior stroke | 2 (5%) |
| GFR (ml/min/1.73m2) | 81.55 ± 23.84 |
| Left ventricular ejection fraction (%) | 52.81 ± 12.53 |
| Vessel | |
| Left anterior descending | 19 (47.5%) |
| Left circumflex | 6 (15%) |
| Right coronary artery | 15 (37.5%) |
Table 1: Baseline characteristics.
Mainly patients were male gender (62.5%). The mean age was 61.78 ± 9.27 years. The most indication for coronary angiography was NSTE-ACS (67.5%). Fifty percent of patients had hypertension.
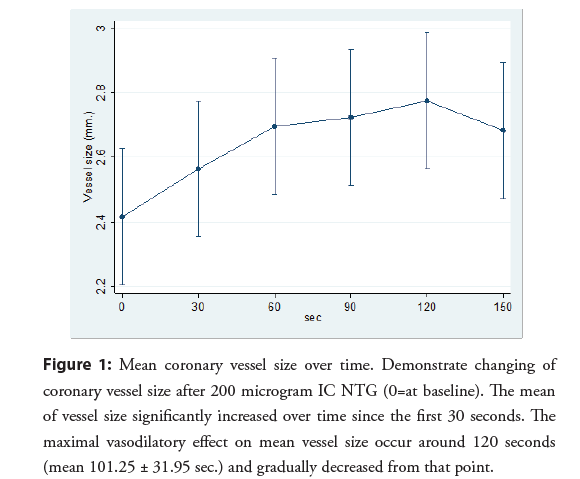
Coronary artery diameter was significantly increased after 200 mcg IC NTG administration. These significant changes were observed in every period. The mean time for a maximal change of coronary artery diameter was observed at 101.25 ± 31.95 seconds. The maximal increase in vessel size was 0.36 mm. (95% CI 0.29, 0.43 p<0.001) at 120 seconds (Table 2). Changes in vessel diameter over a period of time were demonstrated in Figure 1.
| Vessel size (mm.) ± SD | Mean change (mm. (95% CI)) | p-value | |
|---|---|---|---|
| Baseline | 2.42 ± 0.59 | Reference | 1 |
| 30 sec. | 2.56 ± 0.68 | 0.15 (0.08, 0.21) | <0.001* |
| 60 sec. | 2.7 ± 0.73 | 0.28 (0.21, 0.35) | <0.001* |
| 90 sec. | 2.72 ± 0.7 | 0.31 (0.24, 0.37) | <0.001* |
| 120 sec. | 2.77 ± 0.74 | 0.36 (0.29, 0.43) | <0.001* |
| 150 sec. | 2.68 ± 0.69 | 0.27 (0.2, 0.33) | <0.001* |
Table 2: Coronary artery vessel size and mean changes.
Figure 1: Mean coronary vessel size over time. Demonstrate changing of coronary vessel size after 200 microgram IC NTG (0=at baseline). The mean of vessel size significantly increased over time since the first 30 seconds. The maximal vasodilatory effect on mean vessel size occur around 120 seconds (mean 101.25 ± 31.95 sec.) and gradually decreased from that point.
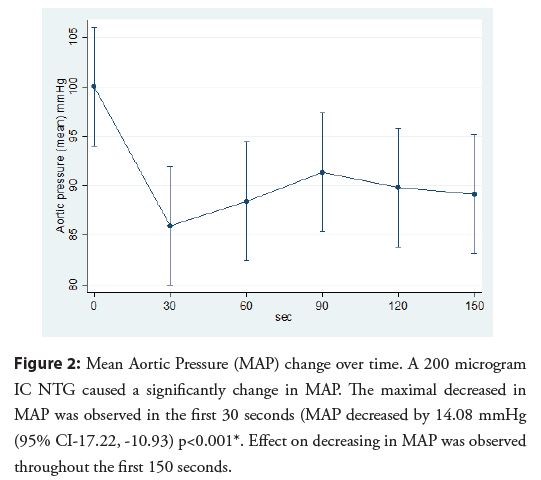
Mean aortic pressure significantly decreased after administered 200 microgram IC NTG. The mean time for a maximal change of mean aortic pressure was 63.75 ± 41.99 seconds. The maximal decreased of mean aortic pressure was -14.08 mmHg (95% CI- 17.22, -10.93) (Table 3). No patient developed a serious adverse event from changing in aortic pressure (Figure 2).
| Mean aortic pressure (mmHg) ± SD | Mean change (mmHg (95% CI)) | p-value | |
| baseline | 100.03 ± 21.88 | Reference | 1 |
| 30 sec | 85.95 ± 17.39 | -14.08 (-17.22, -10.93) | <0.001* |
| 60 sec | 88.42 ± 18.9 | -11.6 (-14.75, -8.45) | <0.001* |
| 90 sec | 91.35 ± 19.53 | -8.68 (-11.82, -5.53) | <0.001* |
| 120 sec | 89.83 ± 20.34 | -10.2 (-13.35, -7.05) | <0.001* |
| 150 sec | 89.15 ± 19.62 | -10.88 (-14.02, -7.73) | <0.001* |
Table 3: Mean aortic pressure and mean change.
Figure 2: Mean Aortic Pressure (MAP) change over time. A 200 microgram IC NTG caused a significantly change in MAP. The maximal decreased in MAP was observed in the first 30 seconds (MAP decreased by 14.08 mmHg (95% CI-17.22, -10.93) p<0.001*. Effect on decreasing in MAP was observed throughout the first 150 seconds.
Discussion
NTG was widely used for relieving angina pectoris. Mechanism of action is prolonged vasodilatation of epicardial coronary artery and reducing left ventricular filling pressure by affecting systemic venous return [9,10]. NTG also be used for evaluation coronary artery diameter, either invasive or non-invasive methods such as invasive coronary angiography and computed tomography coronary angiography [11]. Many forms of NTG such as oral short-acting, long-acting, sublingual, and intravenous forms are widely available. However, intravenous form via intracoronary administration is the most frequently used in the cath lab because of its rapid onset, more reliable and convenient administrative route [12,13].
There are many reports about the effectiveness and dosage of IC NTG Robert et al. studied optimal IC NTG dosage on the degree of coronary artery dilation [2]. They concluded that a maximal increase in coronary diameter occurred after 150 micrograms, and no additional effect after 250 micrograms. This study performed in 1982, use an old type (35 mm. film) coronary angiogram and obtained only one angiographic picture at 2 minutes after IC NTG administration.
Ahmed et al. determined time to maximal vasodilator effect of intracoronary NTG while performing intravascular ultrasound (IVUS). They concluded that with 200 mcg of NTG can get maximal vasodilation at around 2 minutes [8]. However, IVUS can cause coronary spasms and may not be used in the context of coronary angiography.
Feldman et al. studied different sublingually NTG doses and changes in hemodynamics in 13 patients [14]. A 75 to 150 μg sublingual NTG made a significant change of left anterior descending coronary artery by 20 percent and left circumflex artery around 22 percent from baseline but without significant change in heart rate or mean aortic pressure. Investigators also increasing the dose of sublingual NTG up to 450 μg and found an additional increasing in vessel size of left anterior descending artery up about 9 percent and left circumflex about 7 percent. However, Heart rate significantly increased 5 beats per minute and blood pressure decreased 11 mmHg when compared with baseline.
Nowadays, data for time to maximal the vasodilator effect of IC NTG is very limited. This study might answer this question and lead to an optimized technique and reduced time-wasting. This study demonstrates the effect of IC NTG by measuring vessel size that was obtained by cineangiogram every 30 seconds for a total of 150 minutes. Results of this study show a significant response to NTG occur within the first 30 seconds, and reaching maximal vasodilatory effect at 101.25 seconds. Mean vessel size tends to decrease after 120 seconds. This information can guide us for an optimal time to interpret vessel size in case of using IC NTG, especially for coronary spasms.
Despite benefits, NTG also causes adverse effects such as changes in hemodynamics such as blood pressure and heart rate which are dose-related. These adverse effects can be observed in every administrative route. Hypotension usually mild and manageable but can be occasionally severe symptoms [15].
A significant decrease in aortic pressure also occurred in this study. Hypotension beginning for the first 30 seconds and persisted throughout 150 seconds. Every patient gradually resolved from hypotension thereafter. There was no patient in this study got serious event from this effect. According to existing evidence, hemodynamic side effects might be avoided by reducing the dose of NTG.
This study has some limitations. First, the information from this study may not be used in the case of post-Percutaneous Coronary Intervention (PCI), either immediately or previously PCI. Second, a significant change of aortic pressure, even there was no serious event, may cause operator concern. A lower dose of IC NTG should be tested to compare both efficacy and safety. Further study with more number of patients and dose comparing between different dose (lower or standard dose) IC NTG effects on coronary spasm might be giving more information.
Conclusion
In PCI naïve coronary artery, IC NTG make significant increase of coronary artery diameter occur for the first 30 seconds and reaching maximal effect around 2 minutes then vasodilatory effect gradually declined, Aortic pressure was statistical significantly reduced but without clinical significance.
Conflict of Interest
The author has no conflicts of interest to declare.
References
- Parker JD, Parker JO. Nitrate therapy for stable angina pectoris. N Engl J Med. 338(8): 520-31 (1998).
- Feldman RL, Marx JD, Pepine CJ, et al. Analysis of coronary responses to various doses of intracoronary nitroglycerin. Circulation. 66(2): 321-7 (1982).
- Yasue H, Nakagawa H, Itoh T, et al. Coronary artery spasm-clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 51(1): 2-17 (2008).
- Balaban Y, Kaya A, Satilmisoglu MH, et al. Intracoronary focal nitroglycerin injection through drilled balloon is very effective in the resolution of coronary spasm versus into proximal coronary artery: A prospective randomized comparison study. J Interv Cardiol. 31(6): 765-74 (2018).
- Her AY, Singh GB, Chung JH, et al. Vasoconstrictor component of atherothrombotic culprit lesions in ST-segment elevation myocardial infarction. J Saudi Heart Assoc. 31(3): 114-20 (2019).
- Vishnevsky A, Fischman DL, Savage MP. Intracoronary nitroglycerin: Recognizing coronary spasm first and foremost to avoid unnecessary coronary stents. Expert Rev Cardiovasc Ther. 15(10): 727-8 (2017).
- Ilia R, Shimony A, Cafri C, et al. Angiographic characteristics of catheter-induced spasm of the left main coronary artery. Am J Cardiol. 117(4): 571-3 (2016).
- Ahmed B, Martinez JD, Schevchuck A, et al. Appropriate timing of nitroglycerin prior to intravascular ultrasound. J Invasive Cardiol. 24(9): 422-6 (2012).
- Winbury MM, Howe BB, Hefner MA. Effect of nitrates and other coronary dilators on large and small coronary vessels: An hypothesis for the mechanism of action of nitrates. J Pharmacol Exp Ther. 168(1): 70-95 (1969).
- Holtermann W, Lochner W. Effects of nitroglycerin, dipyridamole, carbocromen, xanthinol nicotinate, and butallylonal on venous return. Arzneimittelforschung. 22(8): 1376-81 (1972).
- Takx RA, Sucha D, Park J, et al. Sublingual nitroglycerin administration in coronary computed tomography angiography: A systematic review. Eur Radiol. 25(12): 3536-42 (2015).
- Esente P, Giambartolomei A, Gensini GG. The use of injectable nitroglycerin in the cardiac catheterization laboratory: Nitroglycerin in cardiac catheterization. Angiology. 33(5): 319-24 (1982).
- Bentivoglio LG, Gruntzig A. Relief by intracoronary glyceryl trinitrate of coronary artery spasm resistant to sublingual route of administration. Br Heart J. 46(5): 581-3 (1981).
- Feldman RL, Pepine CJ, Curry RC, et al. Coronary arterial responses to graded doses of nitroglycerin. Am J Cardiol. 43(1): 91-7 (1979).
- Brandes W, Santiago T, Limacher M. Nitroglycerin-induced hypotension, bradycardia, and asystole: Report of a case and review of the literature. Clin Cardiol. 13(10): 741-4 (1990).