Research Article - Imaging in Medicine (2017) Volume 9, Issue 3
Topography of mental foramen in a selected Belarusian population according to cone beam computed tomography
Sergey Lvovich Kabak1, Natallia Victorovna Zhuravleva1, Yuliya Michailovna Melnichenko1* and Nina Alexandrovna Savrasova21Human Morphology Department, Belarusian State Medical University, Minsk, Belarus
2Radiation Examination and Radiation Therapy Department, Belarusian State Medical University, Minsk, Belarus
- *Corresponding Author:
- Yuliya
Michailovna
Melnichenko
Human Morphology
Department Belarusian State Medical University Minsk, Belarus
E-mail: mjm1980@yandex.ru
Abstract
Keywords
cone beam computed tomography ▪ mental foramen ▪ anterior loop
Introduction
The mental foramen (MF) is a topographic anatomical landmark for mental anesthesia in dentistry. It has an oval or circular shape and is located on the outer surface of the mandible on both sides off the midline at a one quarter distance between the profile projections of the mandibular symphysis and posterior edge of the ramus [1]. MF is the output point of the canal of the same name containing a neurovascular bundle.
The location of MF varies in a wide range in different ethnic and age groups as well as gender variations were observed [2]. For instance, among Mongoloids (Chinese and Malay subjects), the mental foramen is usually located apical to the lower second premolar [3,4] whereas in Caucasian subjects it is usually found between the mandibular premolars [5].
Injuries of mental nerve branches near MF may occur through a number of dental procedures, including extractions, endodontic treatment of teeth; lower lip and chin soft tissue reconstruction surgery; bone fragment immobilization and dental implant placement [6-8]. Modern radiographic methods can be helpful in clarifying individual topography of the mental foramen in vivo and so preventing possible complications during or after treatment. The crucial benefit of cone-beam computed tomography (CBCT) is overcoming the limitations of conventional radiography by producing three-dimensional (3D) images that allow comprehensive evaluation of the anatomy of the chosen region [9].
The objective of the present research was to assess the most frequent location, shape, size and individual variations in topography of the mental foramen in adults using cone-beam computed tomography. This type of research has never been performed in the Republic of Belarus previously.
Materials and Methods
This retrospective randomized study consisted of 235 CBCTs obtained from 2014 to 2016 at Minsk dental outpatient hospitals. Images were performed for different reasons such as dental implant planning, diagnosis of radiolucent lesions and temporomandibular joint disorders.
The CBCT scans were selected according to the following inclusion criteria: the presence of mandibular canines, premolars and the first molars on each side, visibility of MF, patient’s age older than 18 year and younger than 60 years. The exclusion criteria consist of CBCT images with large pathological lesions in mandible and bone fractures in region of examination, lesions observed in the apical area of premolars and MF. According to our inclusion and exclusion criteria, the final sample group included data from 117 patients (61 males and 56 females). This work was approved by the ethics committee of Belarusian State Medical University, Minsk (record of meeting 03.12.2012 №2). All patients gave written consent after the purposes of the study were explained to them.
CBCT images were obtained by Galileos GAX5 scanner using standard settings (85 kV; tube current 5-7 mA; acquisition period 14 s; effective radiation time 2-6 s; voxel size 0.3*0.3*0.3 mm). Axial, sagittal, panoramic and formatted transverse tomograms were assessed as well as 3D reconstructed images using GALILEOS Viewer (Sirona, Bensheim, Germany).
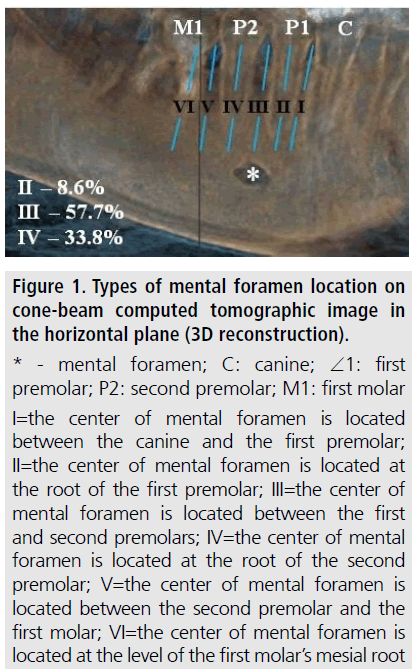
Figure 1. Types of mental foramen location on
cone-beam computed tomographic image in
the horizontal plane (3D reconstruction).
* - mental foramen; C: canine; ∠1: first
premolar; P2: second premolar; M1: first molar
I=the center of mental foramen is located
between the canine and the first premolar;
II=the center of mental foramen is located at
the root of the first premolar; III=the center of
mental foramen is located between the first
and second premolars; IV=the center of mental
foramen is located at the root of the second
premolar; V=the center of mental foramen is
located between the second premolar and the
first molar; VI=the center of mental foramen is
located at the level of the first molar’s mesial root
The center of MF in the horizontal plane (mesiodistal direction) was evaluated with respect to the lines drawn through the top of the root of the adjacent tooth parallel to the long axis or the line drawn through the middle of the distance between the roots of two adjacent teeth (FIGURE 1). According to Tebo and Telfold’s classification [10] there are six types of MF’s center location: type I- the center of MF is located between the canine and the first premolar; type II - the center of MF is located at the root of the first premolar; type III - the center of MF is located between the first and second premolars; type IV - the center of MF is located at the root of the second premolar; type V - the center of MF is located between the second premolar and the first molar; type VI - the center of MF is located at the level of the first molar’s mesial root.
The center of MF in the vertical plane was determined in relation to the apex of a corresponding tooth or horizontal line, drawn through apices of both neighbor teeth (premolars). There are three various locations of MF [11,12]: above the root apex (closer to the crown); at the level of the root apex; beyond the root apex. The projection line was measured from the upper or lower edge of the foramen in the patients with the first and second position respectively.
The vertical (a) and horizontal (b) diameters of MF were measured on sagittal and axial tomograms. There are three types of MF considering the shape and vertical/horizontal diameter relation: horizontal oval –(a/b>1.24), vertical oval –(a/b ≤ 0.76) and round –(0.76 ≤ a/b ≤ 1.24) [13].
The position of the MF in relation to anatomical landmarks of the mandible was determined by the following morphometric parameters:
• MF-MF the distance between mental foramina (the distance between edges of foramina on the mesial surface of the labial cortical plate);
• AC-MB the distance from the alveolar crest to the base of the mandible;
• AC-MF the distance from the alveolar crest to the upper edge of the mental foramen;
• MF-MB the distance from the lower edge of the mental foramen to the base of the mandible;
• MF-A the distance from the upper edge of foramen to the horizontal line, drawn through the nearest root apex.
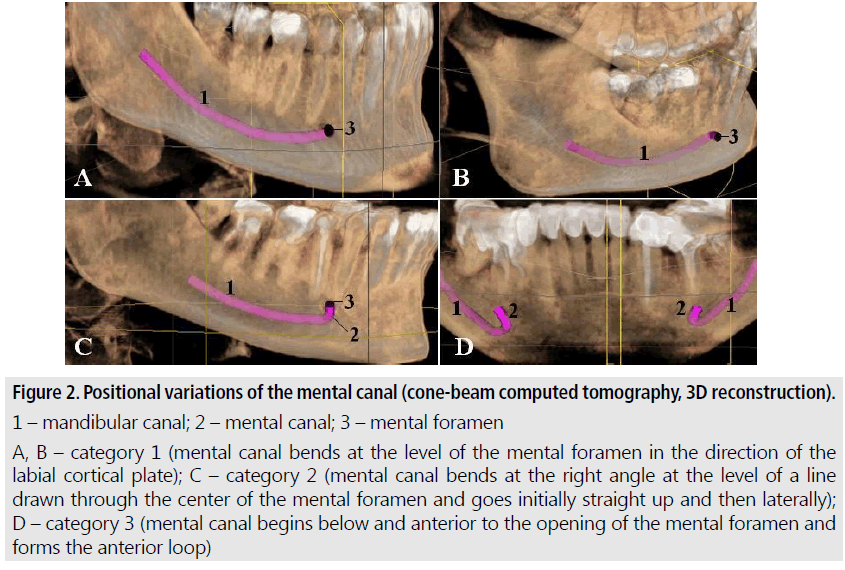
There are three categories of directional paths of mental canal [14].The first category includes canals bending in the direction of the labial cortical plate at the MF level. The second category includes canals bending at a right angle at the level of a projection line drawn through the center of MF and then going vertically and laterally. The third category includes canals going to MF anteriorly and inferiorly and forming a loop [1]. In every case the shape of the mental nerve canal was evaluated by two independent observers who were trained and calibrated in visual CT-scan analysis by the certified specialist in radiology. The overall probability of random agreement was 0.83 (p<0.05) using Cohen’s Kappa coefficient which presented a maximum possible agreement between observers.
The obtained data was analyzed using «Statistica 10.0» software package. The distribution was tested using Kolmogorov- Smirnov criterion. The difference significance between the mean values of the studied parameters was tested by Student's t-criterion. All quantitative data was subject to the normal distribution law and presented as the mean (M), standard deviation (SD), minimum and maximum values. The Chi Square test was used to evaluate comparisons between qualitative data parameters.
According to literature data it is called anterior loop of the mental nerve [15], anterior loop of the inferior alveolar nerve [16]; or anterior loop of the mandibular canal [17]. Results were considered significant when the probability of faultless prognosis was 95.5% (p<0.05) [18].
Results
Patients' average age was 32.6 years old (SD ± 11.4) and 77% of them were younger than 40 years of age.
MF was most commonly located between the roots of lower premolars (57.7%) or in the projection of the second lower premolars root (33.8%). Less often, the foramen was found in the projection of the first lower premolar's root (8.6%) (FIGURE 1 and TABLE 1). Mental foramen vertical position types I, V and VI were not observed. The location of MF in a horizontal plane did not always coincide on the right and left side of the mandible in the same patient. Symmetrical localization of MF in the horizontal plane was found in 75 patients (64.1%). In the rest of the cases it was aligned at Mental foramen vertical position types I, V and VI were not observed different levels with respect to the roots of teeth (TABLE 2). It was located at the right lower second premolar level (47.6%) and between the first and second left lower premolars in 20 of 42 cases of an asymmetrical MF location.
| Horizontal position | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Location according to Tebo and Telford [10] |
Overall n (%) | Right side n (%) | Left side n (%) | *p-value | Male n (%) | Female n (%) | *p-value | ||||
| II | 20 (8.6%) | 7 (6.0%) | 13 (11.1%) | 0.23 ns | 11 (9.0 %) |
9 (8.0 %) | 0.78 ns | ||||
| III | 135 (57.7%) | 65 (55.6%) | 70 (59. 9%) | 70 (57.4%) |
65 (58.0 %) |
||||||
| IV | 79 (33.8%) | 45 (38.5%) | 34 (29.1%) | 41 (33.6%) |
38 (33.9%) |
||||||
| Total | 234 (100%) | 117 (100%) | 117 (100%) | 122 (100%) |
112 (100%) |
||||||
| Vertical position | |||||||||||
| Location according to Fishel et al. [11] and Green [12] |
Overall n (%) | Right side n (%) | Left side n (%) | *p-value | Male n (%) | Female n (%) | *p-value | ||||
| 1 | 13 (5.6%) | 6 (5.1%) | 7 (6.0%) | 0.77ns | 5 (4.1%) | 8 (7.1%) | 0.36 ns | ||||
| 2 | 69 (29.5%) | 35 (29.9%) | 34 (29.1%) | 36 (29.5%) |
33 (29.5%) |
||||||
| 3 | 152 (65.0%) |
76 (65.0%) | 76 (65.0%) | 81 (66.4%) |
71 (63.4%) |
||||||
| Total | 234(100) | 117 (100) | 117 (100) | 122(100) | 112 (100) | ||||||
n: number of mental foramina
II=the center of mental foramen is located at the root of the first premolar; III=the center of mental foramen is located between the first and second premolars; IV=the center of mental foramen is located at the root of the second premolar
1=mental foramen is projected coronal to the apex of dental root; 2=mental foramen is projected at the apex of dental root; 3=mental foramen is projected apical to the apex of dental root
* Comparison between male and female, right and left side assessed with the Chi square test, ns=not significant
Mental foramen vertical position types I, V and VI were not observed
Table 1. Horizontal and vertical position of mental foramen in relation to the apices of roots of mandibular teeth.
| Right side | Left side | n | |
|---|---|---|---|
| Location according to Tebo and Telford [10] |
II | III | 3 (7,1%) |
| II | IV | 1 (2.8%) | |
| III | II | 10 (23. 8%) | |
| III | IV | 8 (19,1%) | |
| IV | III | 20 (47.6%) | |
| Total | 42 (100%) |
II=the center of MF is located at the root of the first premolar; III=the center of MF is located between the first and second premolars; IV=the center of MF is located at the root of the second premolar
Mental foramen vertical position types I, V and VI were not observed
Table 2. Frequency of asymmetrical location of MF on the right and left sides of the mandible.
In the majority of patients the mental foramen was projected below the apices of roots (65%), (FIGURE 1 and TABLE 1) at a distance of 3.2 ± 1.3 mm between them. In 29.5% of cases, MF was detected at the level of the projection line drawn through the apex of the root. The first position of mental foramen in the vertical plane (FIGURE 2) was less frequent (5.6%). In such cases, the foramen was found at a distance of 2.2 ± 0.8 mm from the projection line (TABLE 3a).
Figure 2. Positional variations of the mental canal (cone-beam computed tomography, 3D reconstruction). 1 – mandibular canal; 2 – mental canal; 3 – mental foramen A, B – category 1 (mental canal bends at the level of the mental foramen in the direction of the labial cortical plate); C – category 2 (mental canal bends at the right angle at the level of a line drawn through the center of the mental foramen and goes initially straight up and then laterally); D – category 3 (mental canal begins below and anterior to the opening of the mental foramen and forms the anterior loop)
| Predictor | Mean ± SD (n=234) | Range |
|---|---|---|
| AC-MB | 28.9± 2.9 | 21.4-38.8 |
| AC-MF | 13.0 ± 2.2 | 6.9-19.7 |
| MF-MB | 13.0 ± 1.5 | 9.0-17.3 |
| MF-A††| 3.2± 1.3 | 0.9-6.9 |
| MF-MF | 50.5 ± 3.2 | 44.1 ± 57.6 |
Table 3a. The distance (mm) from the mental foramen to anatomical landmarks of the mandible.
There was no statistically significant difference in the location of MF in the horizontal and vertical plane in men and women, as well as on the right and left side of the mandible in the analyzed cohort (TABLE 1).
The distance from the alveolar crest and the lower edge of the mental foramen to the base of the mandible was significantly greater in men than women, as well as the distance from the superior edge of mental foramen to the alveolar crest (TABLE 3b). The distance between contralateral mental foramina fluctuated in the range from 44.1 to 57.6 mm. The distance was significantly greater in men than in women (p<0.05).
| By side | |||||
|---|---|---|---|---|---|
| Predictor | Right side (n=117) Mean ± SD |
Range | Left side (n=117) Mean ± SD |
Range | p-value |
| AC-MB | 29.0 ± 2.8 | 23.2-36.2 | 28.8 ± 3.03 | 21.4-38.8 | 0.53 ns |
| AC-MF | 13.0 ± 2.3 | 6.9-19.7 | 12.9 ± 2.13 | 8.5-19.0 | 0.72 ns |
| MF-MB | 13.0 ± 1.6 | 9.0-17.1 | 13.0 ± 1.4 | 9.7-17.3 | 0.85 ns |
| MF-A | 3.2 ± 1.3†| 1.2-6.9 | 3.1 ± 1.4‡ | 1.1-6.1 | 0.87 ns |
| †n=76, ‡ n=101 | |||||
| By gender | |||||
| Predictor | Male (n=122) Mean ± SD |
Range | Female (n=112) Mean ± SD |
Range | p-value |
| AC-MB | 30.1 ± 2.7 | 21.4-38.8 | 27.6 ± 2.5 | 22.7-36.2 | 0.00* |
| AC-MF | 13.4 ± 2.2 | 6.9-19.0 | 12.5 ± 2.1 | 8.4-19.0 | 0.00* |
| MF-MB | 13.5 ± 1.4 | 10.1-17.3 | 12.4 ± 1.4 | 9.0-16.5 | 0.00* |
| MF-A | 3.3 ± 1.3§ | 1.2-6.8 | 3.1 ± 1.3¦ | 0.9-6.9 | 0.65 ns |
| MF-MF | 51.6 ± 3.3 | 45.3 ± 57.6 | 49.3 ± 2.8 | 44.1-57.1 | 0.00* |
| § n=81, ¦n=72 | |||||
n: number of mental foramina
AC-MB is the distance from the alveolar crest to the base of the mandible, AC-MF is the distance from the alveolar crest to the superior border of MF, MF-MB is the distance from the inferior border of MF to the base of the mandible, MF-A is the distance from the superior border of MF to the level of roots (the horizontal line drawn through the root apex of the nearest tooth ), MF-MF is the distance between two mental foramina ( the distance between the mesial borders of MF on the labial cortical plate)
Groups (male and female, right and left side) compared using Student T-test. Significance at p = 0.5, ns=not significant, *-significant Table 3b. The distance (mm) from the mental foramen to anatomical landmarks of the mandible related to the side and gender.
Table 3b. The distance (mm) from the mental foramen to anatomical landmarks of the mandible related to the side and gender.
The mental foramen usually had an oval shape elongated in the horizontal direction (84.2%) and less frequently demonstrated round shape and oval shape elongated in a vertical direction (15.4 and 0.4%, respectively, TABLE 4). Shape of the MF regarding to side and gender presented in TABLE 5. The horizontal and vertical size was significantly greater in men than in women (TABLE 6) (p<0.05).
| Shape | n | % |
|---|---|---|
| Oval horizontal shape | 197 | 84.2 |
| Round shape | 36 | 15.4 |
| Oval vertical shape | 1 | 0.4 |
| Total | 234 | 100 |
n: number of mental foramina
Table 4. Shape of the mental foramen.
Shape |
Right side | Left side | ||
|---|---|---|---|---|
| n | % | n | % | |
| Oval horizontal | 98 | 83.8 | 99 | 84.6 |
| Round | 18 | 15.4 | 18 | 15.4 |
| Oval vertical | 1 | 0.9 | 0 | 0 |
| Total | 117 | 100 | 17 | 100 |
| Shape | Male | Female | ||
| n | % | n | % | |
| Oval horizontal | 100 | 82.0 | 97 | 86.6 |
| Round | 21 | 17.2 | 15 | 13.4 |
| Oval vertical | 1 | 0.8 | 0 | 0 |
| Total | 112 | 100 | 112 | 100 |
n: number of mental foramina.
Table 5. Shape of the mental foramen related to the side and gender.
| Gender/side/total | Mean ± SD | Range | P value |
|---|---|---|---|
| Male (n=122) | |||
| Horizontal diameter (mm) | 2.14 ± 0.47 | 1.38-4.76 | p=0,00* |
| Vertical diameter (mm) | 2.52 ± 0.53 | 1.45-4.27 | |
| Female (n=112) | |||
| Horizontal diameter (mm) | 3.34 ± 0.77 | 1.5-6.54 | p=0,00* |
| Vertical diameter (mm) | 2.14 ± 0.47 | 1.38-4.76 | |
| Right side (n=117) | |||
| Horizontal diameter (mm) | 3.61 ± 0.75 | 1.5-5.35 | p=0,31ns |
| Vertical diameter(mm) | 2.38 ± 0.54 | 1.45-4.76 | |
| Left side(n=117) | |||
| Horizontal diameter (mm) | 3.54 ± 0.91 | 1.92-7.1 | p=0,46ns |
| Vertical diameter (mm) | 2.31 ± 0.53 | 1.38-3.53 | |
| Total (n=234) | |||
| Horizontal diameter (mm) | 3.57 ± 0.83 | 1.5-7.1 | |
| Vertical diameter (mm) | 2.34 ± 0.53 | 1.38-4.76 | |
Groups (male and female, right and left side) compared using Student T-test, ns=not significant, *- significant
Table 6. Morphometric measurements of the mental foramen related to side and gender.
| Options (By Demir et al. [14]) | Right side n (%) | Left side n (%) | p-value | Male n (%) | Female n (%) | p-value | Total |
|---|---|---|---|---|---|---|---|
| 1st variation | 61 (52.1%) | 67 (57.3%) | 0,37ns | 70 (57.4%) | 58 (51.8%) | 0,39ns | 128 (54.7%) |
| 2nd variation | 19 (16.2%) | 19 (16.2%) | 19 (15.6%) | 19 (17.0%) | 38 (16.2%) | ||
| 3rd variation | 37 (31.6%) | 31 (26.5%) | 33 (27.1%) | 35 (31.3%) | 68 (29.1%) |
1st variation– the canal starts at the level of the foramen and goes in lateral direction
2nd variation – the canal starts at the level of the foramen and goes vertically upwards, then in lateral direction
3rd variation – the canal starts mesially (anteriorly) to the foramen and goes backwards and upwards, forming a loop
Groups (male and female, right and left side) compared using Chi square test, ns=not significant.
Table 7. Variations of the mental nerve canal pathways regarding the mental foramen.
TABLE 7 presents variations found in the mental foramen and mental nerve canal position. In most cases the canal started at the level of the mental foramen. The second most frequent configuration of the mental canal included a starting point located mesially to the mental foramen and a loop formed by the canal running backwards and upwards. In 16.2% of cases the mental nerve canal started below the MF, then went up and bent again in the lateral direction. There was no statistically significant difference in the frequency of different mental canal position presence in men and women, as well as on the right and left sides. Symmetrical location of the mental nerve anterior loop was found in 38.8% of cases (TABLE 8).
| Anterior loop | n (%) |
|---|---|
| Bilateral | 19 (38.8) |
| Unilateral: left | 12 (24.5) |
| Unilateral: right | 18 (36.7) |
| All | 49 (100) |
n: number of patients.
Table 8. Unilateral vs bilateral presence of the anterior mental loop.
Discussion
For a long time, the anatomical dissection was considered as the main method of facial bone detailed structural analysis, allowing acquisition of more accurate information compared to radiographic images. In particular, MF cannot be always detected on dental images [19].
In recent years the cone-beam computed tomography which was implemented in practical public health services in the late XX has been found to be in great demand among dentists. Adequate spatial resolution, an ability to perform accurate measurements, a relatively small dose of radiation, as well as an absence of many shortcomings of traditional radiography allow to use this method to objectively assess the state of the maxillofacial skeleton and the whole dental system [20,21].
In the present study, MF was detected on both sides of the mandible in all examined cases using CBCT, the size was measured and the exact location of foramina was detected. Jacobs et al. [22] and Parnia et al. [23] also noticed good visualization and 100% detectability of MF on CBCT scans. Three-dimensional radiographic evaluation of MF in relation to the roots of the teeth is more detailed compared to the anatomical method, because the latter does not assess the degree of distal deviation of roots [20].
Our data shows that MF is generally located between the roots of lower premolars or in the projection of the root of the second premolar. The 3rd type of foramen location is also prevalent in a number of European populations (British, Polish, Swiss, Kosovo Albanians) [24-27]. Moreover, Gawlikowska-Sroka et al. [25] have reported that its position remained unchanged in the skulls of people who lived during the period from the 11th to early 20th century. The second frequent in occurrence is the 4th type of the foramen localization in the horizontal plane. Von Arx et al. [26] performed the study using CBCT in Bern, 3rd and 4th types were detected in 56% and 35.7%, respectively. In people of Bosnia and Herzegovina the 3rd type of MF location (between the roots of the lower premolars) occurred in 20.3% of cases, while in 60.3% of cases it was detected at the level of the root of the second premolar [28]. In Spanish population MF was localized at the apex of the second lower premolar (4th class) in 57.9% of cases and between the second lower premolar and the first lower molar (5th type) in 25.3% of cases [29].
The average distance between the right and left mental foramina, according to our data, equals 50.5 mm. As shown in the literature, this distance ranges from 49.5 to 55.2 mm on the sectional material [30,31] and from 46,5 ± 5 mm [32] to 53,1 ± 3.6 mm [33] on CBCT31 tomograms. The distance between the mental foramen and the incisive canal length determine the width of the mandible bone graft, which can be taken in this field without damaging nerves and blood vessels [31].
The "Safe Zone" narrows in the presence of the anterior loop of the mental nerve. It is formed in cases where the nerve begins mesially to the mental foramen and then runs backward and upward. This type of the mental nerve pathway was found in 29.1% of cases. It was observed more often in women than in men (32% vs. 26%) and on the right than on the left (32% vs. 27%).
Similarly to data shown by Demir et al. [14], Prados-Frutos et al. [15], Couto-Filho et al. [34], de Brito et al. [35], the anterior loop was radiographically detected with a frequency of 7.7% to 59.5%.
According to the listed above findings the usual size of a bone block, which is harvested from the mandibular symphysis, has the height of 1-1.5 mm and width of about 4 cm [36].
Analyzing the MF position in the vertical plane, we found that more than in a half of the cases it is localized below the apices of the premolar roots. In most people of India (72.2%), Iraq (60.1%), Korea (62.5%) and Israel (61.6%) MF is also localized downward from the apices of roots of lower premolars/first molars [11,37,38]. The MF location upwards from the apex of molars roots is a predisposing factor to the complications in immediate implant placement [7]. Moreover, the proximity of premolars root apices to the MF may result in serious neurological complications of the apical periodontitis [39,40].
We have found that the mean distance between the edges of MF and the base of the mandible and alveolar crest is almost the same. Absolute values of those parameters falling within the range of variation presented in the literature. Summarizing information from twelve publications, von Arx [26] indicated that the distance from the MF to the base of the mandible and to the upper edge of the mandible was 12.0-15.6 mm and 15.5 to 16.6 mm, respectively.
Changes in MF position are genetically determined and primarily occur due to an increase in a mandible size. However, phenotypic differentiation of bones and their growth rate in postnatal ontogenesis are known to be influenced by several factors, including epigenetic effects, altering the expression of genes, and plastic effects of environmental factors [41]. Eating habits (food consistence) and the condition of structures surrounding the mandible were referred to the environmental factors, changing the rate of bone remodeling [42,43]. Renaud et al. [41] presented that muscular dystrophy caused reshaping of entire mandible, the rate of bone tissue remodeling changed in the area of molars and points of masticatory muscle attachment in response to changes in food consistency.
In the studied cohort we did not find any statistically significant difference in the topography of mental foramen in men and women comparatively to the roots of mandibular teeth. Those findings are consistent with the results reported in earlier studies which also found gender differences in the level of the foramen location in the horizontal and vertical planes [38,44-46]. However, Fujita and Suzuki [47] found that in Japanese men MF was located more often at the apex of the second premolar, whereas in women it was found mainly close to the second root of the second premolar or between apices of the second premolar and first molar.
We observed the gender difference in MF the linear dimensions, distance between two foramina, and distance from lower edges of foramina to the base of the mandible. It felt in agreement with the data published by Muinelo- Lorenzo et al. [29] indicating that the diameter of foramina, square, and distance to the base of the mandible and alveolar crest are significantly bigger in men, than in women. But Verma et al. [48] stated that mean distance between two MF was also larger in men than in women. Listed above gender peculiarities in mental foramen topography are associated with the gender difference in the size of the mandible.
Conclusion
As stated by the literature, the mean size of the mental foramen can vary in a wide range due to different measurement methods [26]. The data on the mean vertical and horizontal dimensions of the mental foramen that we have obtained falls into this range. In 15.4% of cases the mental foramen had a round shape, and in 84.6% it had an oval shape. As claimed by the literature, the incidence of oval foramina ranged from 56.6% to 83.4% [15,27,28,47,49,50]. However, in the analyzed cohort the oval horizontal shape foramina prevailed, supporting Verna et al. [48].
In the analyzed cohort, MF was projected onto a vertical line, drawn between premolars or through the root of the second premolar. Most often it was located symmetrically on both sides of the mandible. In typical cases MF was located downwards from the horizontal line connecting apices of roots of mandibular teeth and had an oval shape (the horizontal dimension prevailed over the vertical).
Some individual variants of mental foramen and nerve topography are unfavorable because of high risk of iatrogenic injuries. Such are the cases of localization of mental foramen above the apices of the roots of the mandibular teeth as well as the presence of the anterior mental loop.
Acknowledgement
We are grateful to OA Ermakova for help in statistical analysis of research results.
References
- Smajilagić A, Dilberović F. Clinical and anatomy study of the human mental foramen. Bosn. J. Basic Med. Sci. 4, 15-23 (2004).
- Lipski M, Tomaszewska IM, Lipska W et al. The mandible and its foramen: anatomy, anthropology, embryology and resulting clinical implications. Folia. Morphol. (Wartsz). 72, 285-292 (2013).
- Hasan T. Characteristics of the mental foramen in different populations. The. Internet. Journal. of. Biological. Anthropology. 4, 1-7 (2010).
- Ngeow WC, Yuzawati Y. The location of the mental foramen in a selected Malay population. J. Oral. Sci. 45, 171-175 (2003).
- Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 75, 1061-1067 (2004).
- Gianni AB, D’Orto O, Biglioli F et al. Neurosensory alterations of the inferior alveolar and mental nerve after genioplasty alone or associated with sagittal osteotomy of the mandibular ramus. J. Craniomaxillofac. 30, 295-303 (2002).
- Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part ii: mandibular incisive canal, mental foramen and associated neurovascular bundles in relation with dental implantology. J. Oral Maxillofac. Res. 1(1), e3 (2010).
- Song Q, Li S, Patil PM. Inferior alveolar and mental nerve injuries associated with open reduction and internal fixation of mandibular fractures: A Seven Year retrospective study. J. Craniomaxillofac. Surg. 42(7), 1378-1381 (2014).
- Zmysłowska-Polakowska E, Radwański M, Łęski M, et al. The assessment of accessory mental foramen in a selected polish population: A CBCT study. BMC. Med. Imaging. 17, 17 (2017).
- Tebo HG, Telford IR. An analysis of the variations in position of the mental foramen. Anat. Rec. (Hoboken) 107, 61-66 (1950).
- Fishel D, Buchner A, Hershkowith A et al. Roentgenologic study of the mental foramen. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 41, 682-686 (1976).
- Green RM. The position of the mental foramen: a comparison between the southern (Hong Kong) Chinese and other ethnic and racial groups. Oral. Surg. Oral. Med. Oral. Pathol. 63, 287-290 (1987).
- Zhang L, Zheng Q, Zhou X, et al. Anatomic relationship between mental foramen and peripheral structures observed by cone-beam computed tomography. Anat. Physiol. 5, 182 (2015).
- Demir A, Izgi E, NamdarPekiner F. Anterior loop of the mental foramen in a turkish subpopulation with dentate patients: A cone beam computed tomography study. Journal. of. Marmara. University. Institute. of. Health. Sciences. 5 (2015).
- Prados-Frutos JC, Salinas-Goodier C, Manchón Á, et al. Anterior loop of the mental nerve, mental foramen and incisive nerve emergency: Tridimensional assessment and surgical applications. Surg. Radiol. Anat. (2016).
- Juan del VL, Grageda E, Gómez CrespoSJ. Anterior loop of the inferior alveolar nerve: Averages and prevalence based on CT scans. Prosthet. Dent. 115, 156-160 (2016).
- Do Nascimento EH, Dos AnjosPontual ML, Dos AnjosPontual A et al. Assessment of the anterior loop of the mandibular canal: A study using cone-beam computed tomography. Imaging. Sci. Dent. 46, 69-75 (2016).
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 33, 159-174 (1977).
- Kqiku L, Sivic E, Weiglein AH, Glockner K. Position and symmetry of the mental foramen. EC. Dental. Science. 1, 193-195 (2015).
- Saito K, de Araújo NS, Saito MT, et al. Analysis of the mental foramen using cone beam computerized tomography. Rev. Odontol. UNESP. 44, 226-231 (2015).
- Kiarudi AH, Eghbal MJ, Safi Y, et al. The applications of cone-beam computed tomography in endodontics: a review of literature. Iran. Endod. J. 10, 16-25 (2015).
- Jacobs R, Mraiwa N, vanSteenberghe D, et al. Appearance, location, course, and morphology of the mandibular incisive canal: an assessment on spiral CT scan. Dentomaxillofac. Radiol. 31, 322-327 (2002).
- Parnia F, Moslehifard E, Hafezeqoran A, et al. Characteristics of anatomical landmarks in the mandibular interforaminal region: a cone-beam computed tomography study. Med. Oral. Patol. Oral. Cir. Bucal. 17, e420-425 (2012).
- Santini A, Land M. A comparison of the position of the mental foramen in Chinese and British mandibles. Acta. Anat. (Basel). 137, 208-212 (1990).
- Gawlikowska-Sroka A, Stocki Ł, Dąbrowski P, Kwiatkowska B, Szczurowski J, Czerwiński F. Topography of the mental foramen in human skulls originating from different time periods. Homo. 64, 286-295. (2013).
- von Arx T, Friedli M, Sendi P, et al. Location and dimensions of the mental foramen: a radiographic analysis by using cone-beam computed tomography. J. Endod. 39, 1522-1528. (2013).
- Kqiku L, Weiglein A, Kamberi B, et al. Position of the mental foramen in Kosovarian population. Coll. Antropol. 37, 545-549 (2013).
- Voljevica A, Talović E, Hasanović A. Morphological and morphometric analysis of the shape, position, number and size of mental foramen on human mandibles. Acta Med. Acad. 44, 31-38. (2015).
- Muinelo-Lorenzo J, Suárez-Quintanilla JA, Fernández-Alonso A, et al. Anatomical characteristics and visibility of mental foramen and accessory mental foramen: Panoramic radiography vs. cone beam CT. Med. Oral Patol. Oral Cir. Bucal. 20, e707-714 (2015).
- Denissen HW, Kalk W, Veldhuis HA, et al. Anatomic consideration for preventive implantation. Int. J. Oral. Maxillofac. Implants. 8, 191-196 (1993).
- Al-Ani O, Nambiar P, Ha KO, et al. Safe zone for bone harvesting from the interforaminal region of the mandible. Clin. Oral. Implants. Res. 24, 115-121 (2013).
- Madrigal С, Ortega R, Meniz C, et al. Study of available bone for interforaminal implant treatment using cone-beam computed tomography. Med. Oral. Patol. Oral. Cir. Bucal. 13, E307-312 (2008).
- Lee JE, Lee YJ, Jin SH, et al. Topographic analysis of the mandibular symphysis in a normal occlusion population using cone-beam computed tomography. Exp. Ther. Med. 10, 2150-2156 (2015).
- Do Couto-Filho CEG, de Moraes PH, Alonso MBC, et al. Accuracy in the diagnosis of the mental nerve loop. a comparative study between panoramic radiography and cone beam computed tomography. Int. J. Morphol. 33, 327-332 (2015).
- de Brito AC, Nejaim Y, de Freitas DQ, et al. Panoramic radiographs underestimate extensions of the anterior loop and mandibular incisive canal. Imaging. Sci. Dent. 46, 159-165 (2016).
- Park HD, Min CK, Kwak HH, et al. Topography of the outer mandibular symphyseal region with reference to the autogenous bone graft. Int. J. Oral. Maxillofac. Surg. 33, 781-785 (2004).
- Muhsen SJ. Horizontal and vertical position of the mental foramen on panoramic views of a selected Iraqi population. Journal. of. Baghdad. college. of. dentistry. 23, 69-72 (2011).
- Parnami P, Gupta D, Arora V, et al. Assessment of the horizontal and vertical position of mental foramen in indian population in terms of age and sex in dentate subjects by panoramic radiographs: a retrospective study with review of literature. Open. Dent. J. 9, 297-302. (2015).
- Stavrianos C, Eliades A, Stavrianou I. Paresthesia of the mental nerve due to chronic apical periodontitis of a non-vital tooth: a case report. Research Journal of Medical Sciences. 4, 94-97 (2010).
- GencSen O, Kaplan V. Temporary mental nerve paresthesia originating from periapical infection. Case. reports. in. dentistry. (2015).
- Renaud S, Auffray JC, de la Porte S. Epigenetic effects on the mouse mandible: common features and discrepancies in remodeling due to muscular dystrophy and response to food consistency. BMC. Evol. Biol. 10, 28. (2010).
- Yesilyurt H, Aydinilioglu A, Kavakli A, et al. Local differences in the position of the mental foramen. Folia. Morphol. 67, 32-35 (2008).
- Siddiqui AU, Daimi SR, Mishra PP, et al. Morphological and morphometric analysis of mental foramen utilizing various assessment parameters in dry human mandibles. Int. J. Stud. Res. 1, 19-22 (2011).
- Chkoura A, El Wady W. Position of the mental foramen in a Moroccan population: A radiographic study. Imaging. Sci. Dent. 43, 71-75. (2013).
- Babshet M, Sandeep R, Burde K, et al. Evaluation of the position of mental foramen and its correlation with age in selected indian population, using digital panoramic radiograph. Int. J. Dent. Sci. Res. 3, 87-91 (2015).
- Gupta V, Pitti P, Sholapurkar A. Panoramic radiographic study of mental foramen in selected dravidians of south Indian population: A hospital based study. J. Clin. Exp. Dent. 7, e451-456. (2015).
- Fujita A, Suzuki T. Computed tomographic analysis of the mental foramen and nerve in Japanese patients. Implant. dent. 23, 471-476. (2014).
- Verma P, Bansal N, Khosa R, et al. Correlation of radiographic mental foramen position and occulusion in three different indian populations. West. Indian. Med. J. 64, 269-274 (2015).
- Udhaya K, Saraladevi KV, Sridhar J. The morphometric analysis of the mental foramen in adult dry human mandibles: a study on the South Indian population. J. Clin. Diagn. Res. 7, 1547-1551 (2013).
- Eboh DE, Oliseh EI. Analysis of mental foramen in dry human mandibles of adult Nigerians. Afr. J. Med. Med. Sci. 43, 107-113 (2014).