Clinical images - Imaging in Medicine (2020) Volume 12, Issue 3
Tracheobronchopathia Osteochondroplastica - Rare Case
- Corresponding Author:
- Farrell A & Henry MTDepartment of Respiratory Medicine, Cork University Hospital, Cork, Ireland Email: aisling.farrell2@hse.ie
Abstract
Clinical Image
Presentation: A 60yr old male was referred to a tertiary referral centre with a chronic dry cough. He was a lifelong non-smoker. Clinical examination was unremarkable.
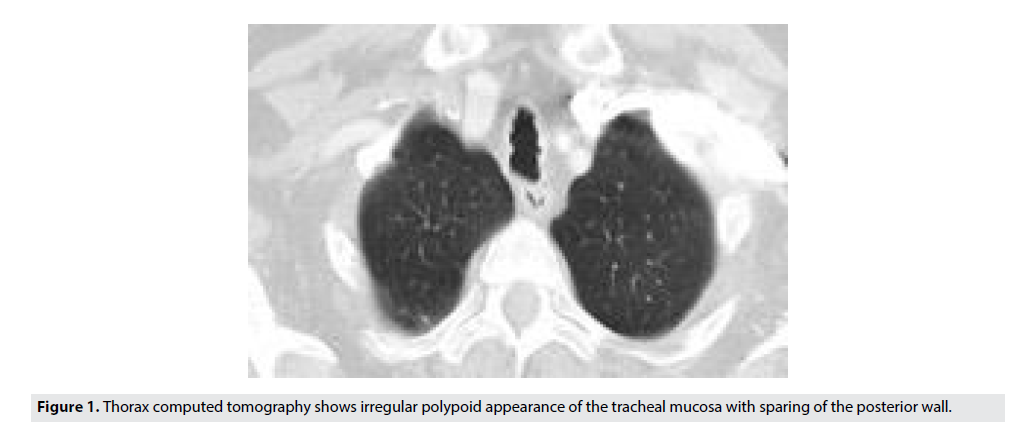
Assessment: IGE, RAST to common allergens, eosinophils and alpha one anti-trypsin were within normal limits. Barium swallow did not show any oesophageal dysmotility, gastric outlet obstruction or reflux. Normal pulmonary function testing with no reversibility noted post bronchodilator. Computed Tomography (CT) of the thorax showed an irregular polypod appearance of the tracheal mucosa on the anterior and lateral surfaces (FIGURE 1).
Figure 1. Thorax computed tomography shows irregular polypoid appearance of the tracheal mucosa with sparing of the posterior wall.
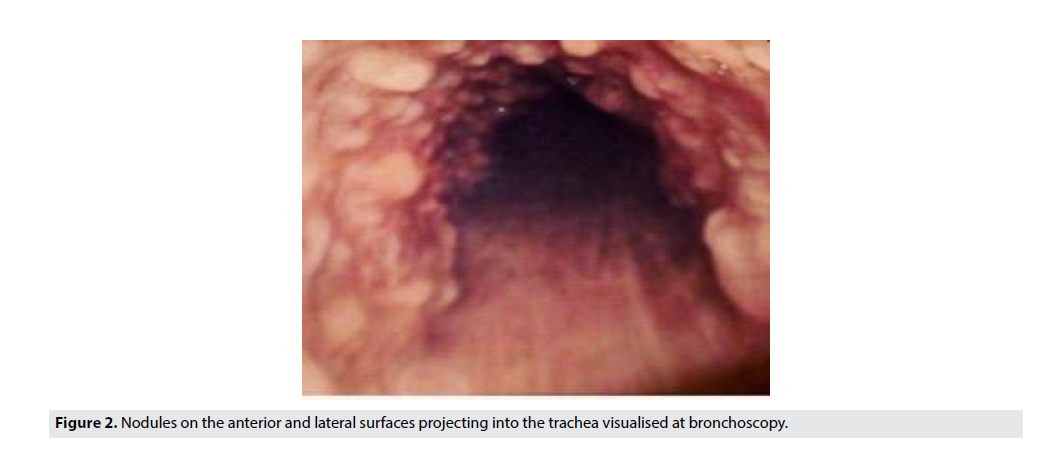
Direct visualisation of this area at bronchoscopy showed nodules projecting into the trachea (FIGURE 2). Endobronchial biopsy demonstrated benign ciliated respiratory type epithelium which included areas of ossification within the sub-epithelial tissue.
Diagnosis: Findings were consistent with a diagnosis of Tracheobronchopathia Osteochondroplastica (TO).
Management: TO is a rare disorder of the large airways, characterised by the presence of multiple bony and cartilaginous nodules in the submucosa of the tracheobronchial wall which can lead to airway obstruction [1]. It is an idiopathic condition and to date, there is no known genetic susceptibility.
Often it is asymptomatic, however some patients present with dry cough, recurrent infection wheeze or rarely stridor [2].
Treatment for TO is symptomatically driven but includes inhaled corticosteroids and bronchodilators [3]. The patient was commenced on inhaled corticosteroids and long-acting bronchodilator with some improvement in his symptoms. Prompt treatment of pulmonary infections, laser therapy, nodule removal and bronchoscopic dilation may be needed in some cases.
Awareness of this rare condition amongst physicians is critical in its correct diagnosis and management.
References
- Simmons C, Vinh D, Donovan DT et al. Tracheobronchopathia osteochondroplastica. Laryngoscope. 126, 2006-2009, (2016).
- Corcoran JP, Wrightson JM, Moore AJ et al. Sykes A. Large airways nodularity secondary to tracheobronchopathia osteochondroplastica. Thorax. 72, 288-289, (2017).
- Ulasli SS, Kupeli E. Tracheobronchopathia osteochondroplastica: A review of the literature. Clin. Respir. J. 9, 386-391, (2015).