Case Series - Interventional Cardiology (2021) Volume 13, Issue 1
Transcatheter coronary artery fistula occlusion in pediatric and adult patients facilitated by detachable coils
- Corresponding Author:
- Kali A. Hopkins
Division of Pediatric Cardiology,
Department of Pediatrics,
Northwestern Feinberg School of Medicine,
Ann & Robert H. Lurie Children’s Hospital of Chicago,
Chicago,
Illinois,
USA,
E-mail: kahopkins@lurichildrens.org
Received date: December 17, 2020 Accepted date: January 06, 2021 Published date: January 13, 2021
Abstract
Coronary artery fistulae are rare congenital or acquired lesions that may require surgical or transcatheter closure to prevent long-term sequelae. We present our experience using detachable coils with expandable hydrogel for successful occlusion of fistulae in patients ranging from 7 months to 82 years of age. The young children demonstrated remarkable remodeling of giant coronary aneurysms after fistula closure.
Keywords
Coronary artery vascular fistula • Coil • Coronary intervention
Background
Coronary artery fistulae (CAF) are connections between a coronary artery and another vessel or cardiac chamber. CAF account for 0.04% of congenital cardiac abnormalities. Acquired CAF are more common and occur following trauma, coronary bypass grafting, infective endocarditis, or Kawasaki disease [1,2]. Hemodynamic consequences range from insignificant to severe, with large volume lesions potentially resulting in coronary steal, volume overload, and congestive heart failure [2]. Long-term sequelae include myocardial infarction, aneurysm formation/rupture, arrhythmias, pulmonary hypertension, and infective endocarditis [1-4]. Options for closure include surgical ligation or transcatheter occlusion [3-6]. Transcatheter occlusion can be challenging, often requiring veno-arterial loops and the need for long sheaths and guide catheters [4] that create technical problems in adults due to length of equipment. The Azur® Hydrocoil Embolization System (Terumo Medical Corporation, Somerset, New Jersey) consists of a platinum frame coated with an expandable hydrogel polymer, which, when activated, increases the filling volume. Coils can be delivered by standard or microcatheters and are detachable, thus making delivery straightforward. Prior reports have documented Azur® Hydrocoil use in congenital heart disease [7]. Here we describe our experience using the Azur® Hydrocoil for CAF closure in four patients ranging from 7 months to 82 years of age (Table 1).
| Case | Age at fistula closure | Gender | Fistula | Associated signs/symptoms | Intervention | Antiplatelet/ anticoagulation | Follow-up |
|---|---|---|---|---|---|---|---|
| 1 | 7 months | Male | LCX to CS | Severe dilation LMCA, LCX, and CS. Moderate LA enlargement. Distal aneurysm | Retrograde deployment of 2 framing coils in aneurysm; AVP II deployed in fistula | Aspirin, clopidogrel, enoxaparin. Enoxaparin stopped after 9 months. | Reverse remodeling of the distal LCX on 9-month catheterization |
| 2 | 14 months | Male | LAD to RV | Dilated LAD and LMCA | Antegrade deployment of 2 coils in the fistula | Aspirin, clopidogrel | Mildly reduced size of distal LMCA, significantly reduced size of proximal LAD |
| 3 | 82 years | Female | RCA to PA; LMCA to PA | Unstable angina | Antegrade deployment of 2 coils in RCA to PA fistula and 3 coils in LMCA to PA fistula | Aspirin | Resolution of angina |
| 4 | 51 years | Female | RCA to PA | Inferior ischemia on stress test | Antegrade deployment of 2 coils in fistula | Aspirin | Resolution of exertional angina and dyspnea |
Abbreviations: CS: Coronary Sinus; LAD: Left Anterior Descending; LA: Left Atrium; LCX: Left Circumflex; LMCA: Left Main Coronary Artery; PA: Pulmonary Artery; RCA: Right Coronary Artery; RV: Right Ventricle
Table 1: Clinical summary.
Case 1
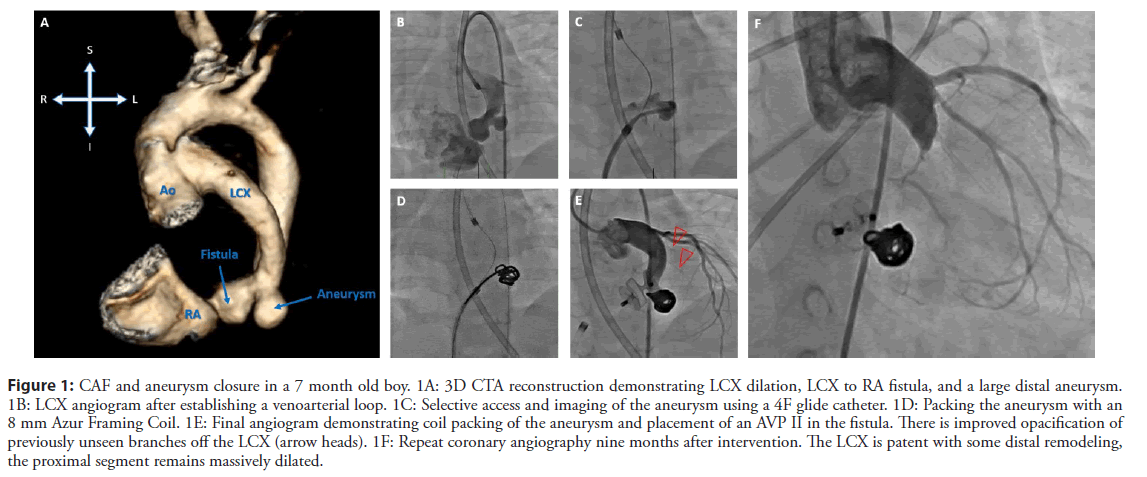
An asymptomatic 4-month-old male presented with a continuous murmur. Electrocardiogram (ECG) showed inferior and apical q waves and transthoracic echocardiogram (TTE) demonstrated dilation of the left main coronary artery (LMCA) (7.6 mm, z-score 15.4), left circumflex artery (LCX) (4.8 mm), and coronary sinus (CS), with flow acceleration at the CS os (velocity=4.8 m/s). computed tomography angiogram (CTA) confirmed a CAF from LCX to CS but with a large aneurysm in the distal LCX measuring 9.4 mm × 8.1 mm (Figure 1A). Diagnostic cardiac catheterization confirmed the lesion and revealed a Qp:Qs of 1.7:1 (Figure 1B). At multi-disciplinary conference the decision was to attempt interventional closure.
At the time of intervention, the patient was 7 months old and weighed 9.8 kg. A 4 French (F) 45 cm Performer sheath (Cook Medical, Bloomington, IN) was placed in the ascending aorta via the right femoral artery (RFA) and a coaxial system comprised of a 4F JL 1.5 (Cook), Bern microcatheter (Boston Scientific, Boston, MA), and an All Track Wire (ATW) (CardinalHealth, Dublin, OH) was used to selectively access the LCX, cross the CS os, and terminate in the right atrium (RA). From a sheath in the right femoral vein (RFV), a 10 mm gooseneck snare (Medtronic, Minneapolis, MN) was used to snare the wire to create a veno-arterial loop. The venous line was exchanged for a 5F 45 cm Performer long sheath, which was then advanced over the wire loop, across the fistula and into the distal LCX. A 4F non-taper angled glide catheter (Terumo) was advanced into the venous sheath alongside (not over) the wire and positioned in the aneurysm (Figure 1C). The aneurysm was then packed using 8 mm × 20 cm then 6 mm × 17 cm Azur® CX Detachable 0.035” Coils (Terumo) (Figure 1D).
With the aneurysm packed, the fistula was closed with a 10 mm Type II Amplatzer Vascular Plug (AVP) (Abbott, Chicago, IL) delivered via the 5F long sheath. The distal disc was extended into the aneurysm neck, thus securing the packing coils in place (Figure 1E). The central and proximal discs were deployed entirely within the saccular pouch of the fistula. Ten-minute follow-up angiogram revealed complete occlusion of the fistula and improved opacification of previously unfilled small coronary branches (Figure 1F). The patient was monitored for four days and discharged on triple anticoagulation (aspirin 40.5 mg orally daily, clopidogrel 0.2 mg/kg orally daily, enoxaparin 1 mg/kg subcutaneously twice daily).
At 16 months of age, a follow-up catherization was performed. Angiography revealed remodeling of the distal LCX, though the LMCA (9.1 mm, z-score 17.8) and proximal LCX remained dilated. The LCX starts to taper at its origin and after 1 cm, the diameter normalizes (1.2 mm) (Figure 1G). TTE demonstrated normal biventricular function and the ECG had normalized. Enoxaparin was stopped, and the patient remains on dual antiplatelet therapy (DAPT) of aspirin and clopidogrel.
Figure 1: CAF and aneurysm closure in a 7 month old boy. 1A: 3D CTA reconstruction demonstrating LCX dilation, LCX to RA fistula, and a large distal aneurysm. 1B: LCX angiogram after establishing a venoarterial loop. 1C: Selective access and imaging of the aneurysm using a 4F glide catheter. 1D: Packing the aneurysm with an 8 mm Azur Framing Coil. 1E: Final angiogram demonstrating coil packing of the aneurysm and placement of an AVP II in the fistula. There is improved opacification of previously unseen branches off the LCX (arrow heads). 1F: Repeat coronary angiography nine months after intervention. The LCX is patent with some distal remodeling, the proximal segment remains massively dilated.
Case 2
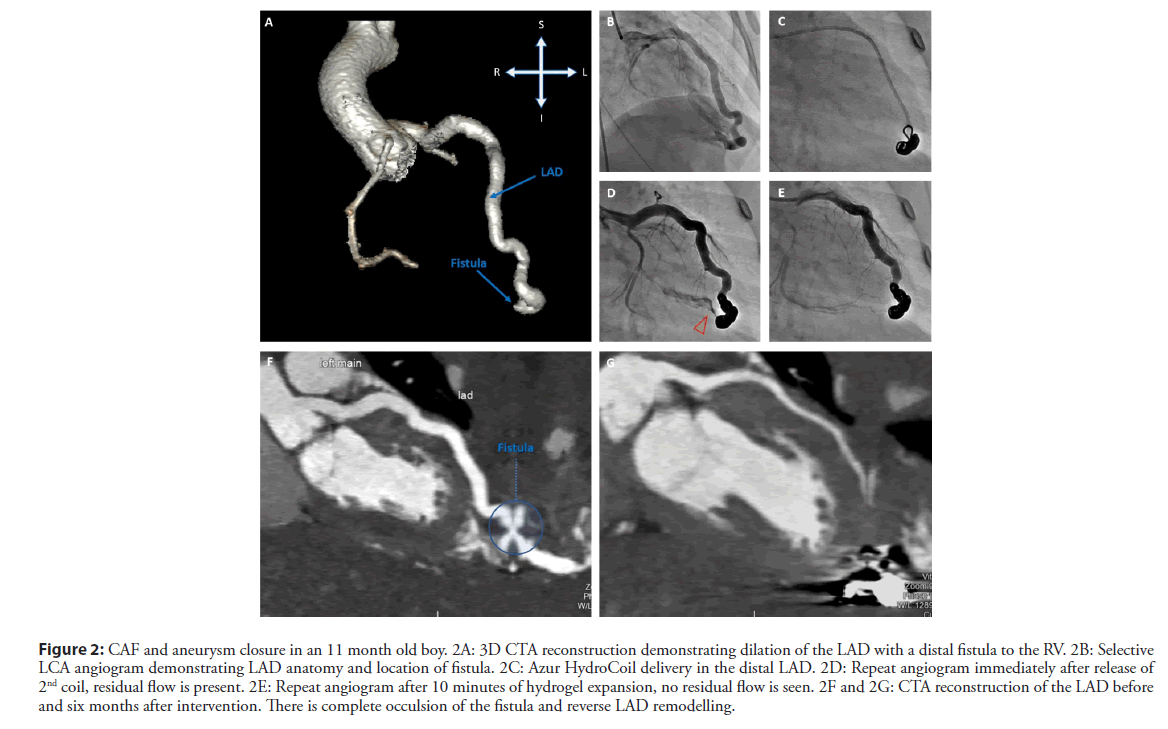
An asymptomatic 11-month-old male presented with a continuous murmur. TTE revealed severe dilation of the left anterior descending (LAD) coronary artery. The proximal LAD measured 3.8 mm (z-score 9.1) and the mid-LAD measured 4.4 mm (z-score 11.2). The normal origin LMCA was dilated at 3.7 mm (z-score 3.3). CTA confirmed the findings and further demonstrated that the LAD coursed to the cardiac apex where it directly communicated with the right ventricular cavity (Figure 2A). The LCX and Right Coronary Arteries (RCA) were normal.
Figure 2: CAF and aneurysm closure in an 11 month old boy. 2A: 3D CTA reconstruction demonstrating dilation of the LAD with a distal fistula to the RV. 2B: Selective LCA angiogram demonstrating LAD anatomy and location of fistula. 2C: Azur HydroCoil delivery in the distal LAD. 2D: Repeat angiogram immediately after release of 2nd coil, residual flow is present. 2E: Repeat angiogram after 10 minutes of hydrogel expansion, no residual flow is seen. 2F and 2G: CTA reconstruction of the LAD before and six months after intervention. There is complete occulsion of the fistula and reverse LAD remodelling.
Cardiac catheterization, performed at 14 months of age and 11.5 kg, confirmed dilation of the LAD and a distal connection to the right ventricle (Figure 2B). Prior to intervention the patient was loaded with clopidogrel (75 mg). Coronary artery access was obtained with a coaxial system consisting of a 4F Performer 45 cm long sheath via the RFA, a 4F non-taper angled glide catheter, Bern microcatheter, and a 0.014” ChoICE wire (Boston Scientific). The catheter was delivered to the distal LAD and the microcatheter and wire were removed. A 6 mm × 17 cm then 5 mm × 10 cm Azur® CX Detachable 0.035” Coils were deployed in the fistula (Figure 2C). Initial angiography showed trace residual flow (Figure 2D), but after 10 minutes to allow for hydrogel expansion, repeat angiography demonstrated no residual CAF flow and opacification of the previously unseen proximal branches (Figure 2E). The patient was monitored for four nights, and after an uneventful recovery he was discharged on aspirin 40.5 mg orally daily and clopidogrel 0.2 mg/kg orally daily.
Six months after CAF occlusion, follow-up CTA showed no residual shunt and reverse remodeling of the LMCA (z-score 3.9 down from 9.7) and proximal LAD (z-score 7.0 down from 9.7) (pre- and post-intervention images shown in Figures 2F and 2G, respectively). Given no adverse effects from DAPT, this was continued.
Case 3
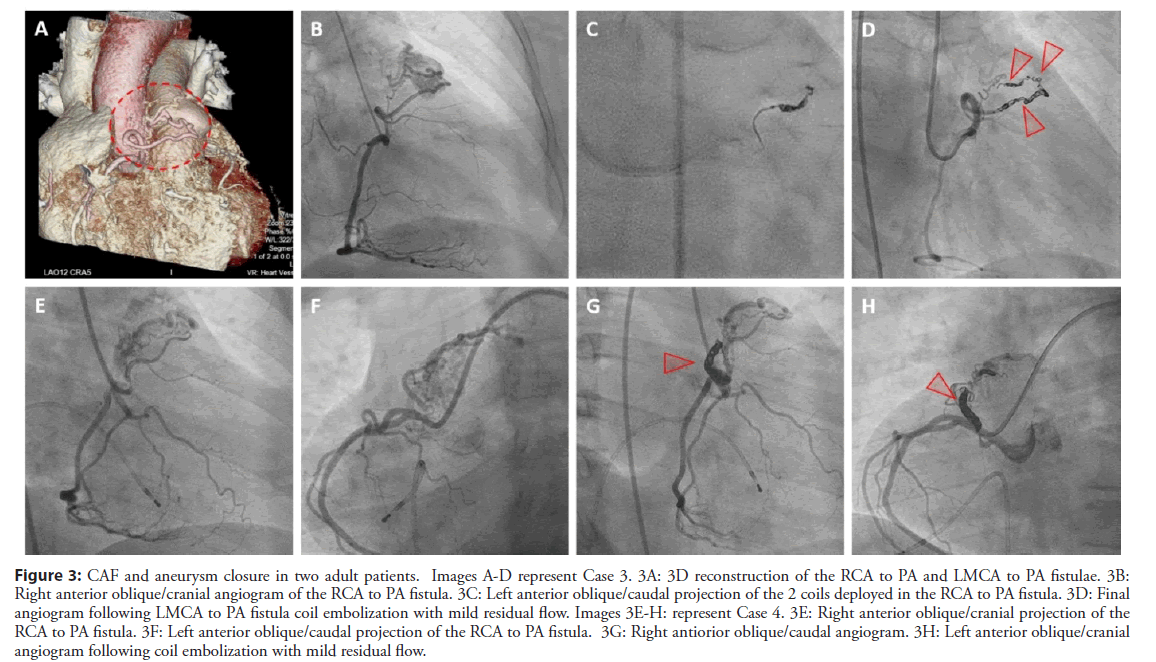
An 82-year-old woman with history of breast cancer treated with external beam radiation therapy presented with unstable angina. Coronary angiogram revealed an RCA artery to pulmonary artery (PA) fistula (Figures 3A and 3B) as well as a LMCA to PA fistula (Figure 3A). The fistulae were characterized on coronary CT. Following six weeks of medication titration, she remained symptomatic with minimal exertion and the decision was made to proceed with coil embolization of the fistulae.
During cardiac catheterization a Bern-shaped microcatheter and a Sion Blue coronary wire (Asahi Intecc USA, Irvine, CA) were used to access the fistulous connection from the LMCA to the PA. Two 2 mm × 4 cm Azur® Hydrocoils were deployed in the fistula. Repeat angiogram approximately 1 hour later revealed no residual flow in the connection (Figure 3D). Again, using the Bern-shaped microcatheter and Sion Blue coronary wire, the fistula from the RCA to the PA was engaged. Three 3 mm × 8 cm Azur Hydrocoils were deployed in the lesion (Figure 3C). There was mild residual flow that was anticipated to cease following coil activation.
Figure 3: CAF and aneurysm closure in two adult patients. Images A-D represent Case 3. 3A: 3D reconstruction of the RCA to PA and LMCA to PA fistulae. 3B: Right anterior oblique/cranial angiogram of the RCA to PA fistula. 3C: Left anterior oblique/caudal projection of the 2 coils deployed in the RCA to PA fistula. 3D: Final angiogram following LMCA to PA fistula coil embolization with mild residual flow. Images 3E-H: represent Case 4. 3E: Right anterior oblique/cranial projection of the RCA to PA fistula. 3F: Left anterior oblique/caudal projection of the RCA to PA fistula. 3G: Right antiorior oblique/caudal angiogram. 3H: Left anterior oblique/cranial angiogram following coil embolization with mild residual flow.
Case 4
A 51-year-old woman with history of hypertension, diabetes mellitus, and a myocardial infarction managed conservatively during pregnancy 25 years prior, presented to her primary care physician with chest discomfort. She was referred to cardiology who recommended coronary angiography. Coronary angiogram revealed an RCA to PA fistula (Figures 3E and 3F). An exercise stress test identified inferior ischemia believed to signify coronary steal phenomenon. Coronary CT confirmed the fistula and the decision was made to proceed with coil embolization.
During cardiac catheterization, using a Runthrough (Terumo) and subsequent Fielder XT (Asahi) coronary wire, the fistulous connection was engaged distally followed by placement of a Progreat microcatheter (Terumo). Two Azur Cx 18 detachable coils were deployed successfully (Figure 3G). There was mild residual flow in the fistulous connection anticipated to cease following coil activation (Figure 3H).
Results and Discussion
Here we present our pediatric and adult experience of CAF occlusion using detachable coils, rendering the procedure far more straightforward than prior techniques. Key factors contributing to the ease of intervention were 1) a coaxial system with microcatheter delivery through standard 4F catheters, 2) the ability to deliver coils via 4F catheter or microcatheter, obviating the need for long sheaths or guide catheters, and 3) detachable release allowing for repositioning or retrieval. Furthermore, the hydrogel expansion post-delivery contributed to complete resolution of residual flow, arguably allowing for CAF closure with a lower coil packing density. All procedures were successful and there were no complications.
We have demonstrated large CAF in infants can be closed with a catheter alone reaching the target site, and smaller coronary artery fistulae in adults can be closed with a microcatheter alone. To our knowledge this series is the first to report use of Azur® Hydrocoils for closure of complex coronary artery fistulae. Only one patient required a veno-arterial loop and he underwent a “traditional” closure with a Type II AVP. The coils in this patient were placed via a catheter alone to successfully occlude a large aneurysm. This was the first time Azur® Hydrocoils were used in this institution, and with the learning curve behind us, it would likely have been possible to close the large fistula with detachable coils via a catheter alone.
Although a case series, there are two aspects of CAF closure that warrant comment. We note in the pediatric patients with coronary artery dilation significant reverse remodeling on follow up imaging. The second issue is anticoagulation post-CAF closure. There is limited literature on the duration and type of therapy despite the risk of thrombosis due to stasis of blood flow [5]. Lacking guidelines on anticoagulation for patients with these types of lesions, for the infants we extrapolated the American Heart Association’s guidelines for Kawasaki disease (KD) patients with residual aneurysms [8]. These guidelines provide a Class IIa recommendation for DAPT in giant aneurysms regressed to medium-size and a Class IIb recommendation for DAPT in addition to anticoagulation for giant persistent aneurysms in the setting of extensive or distal coronary artery aneurysm [8]. For Case 1, triple anticoagulation was prescribed given the massive dilation of the LMCA and LCX. At follow-up after significant remodeling, we continued DAPT. For Case 2, we chose DAPT that we continued after follow-up CTA demonstrated regression to medium-sized aneurysms. For the adult patients without aneurysms, aspirin alone was prescribed and continued indefinitely.
Conclusion
We demonstrate successful use of Azur® Hydrocoils to close coronary artery fistulae in patients spanning a wide age range. The method of coil delivery with catheters and microcatheters obviated the need for guide catheters or long sheaths entering the fistula. The detachable nature of the coil allowed for repositioning. We review our anticoagulation strategy as no guidelines exist.
References
- Burch GH, Sahn DJ. Congenital coronary artery anomalies: The pediatric perspective. Coronary Artery Disease. 12(8): 605-616 (2001).
- Vaidya YP, Green GR. Coronary artery fistula. J Card Surg. 34(12): 1-9 (2019).
- Qureshi SA. Coronary arterial fistulas. Orphanet J Rare Dis. 1(51) (2006).
- Armsby LR, Keane JF, Sherwood MC, et al. Management of Coronary Artery Fistulae: Patient Selection and Results of Transcatheter Closure. JAMA. 39(6): 1026-1032 (2002).
- Kung GC, Moore P, McElhinney DB, et al. Retrograde transcatheter coil embolization of congenital coronary artery fistulas in infanfs and young children. Pediatr Cardiol. 24: 448-53 (2003).
- Aggarwal V, Mulukutla V, Qureshi AM, et al. Congenital coronary artery fistula: Presentation in the neonatal period and transcatheter closure. Congenit Heart Dis. 13(5): 782-787 (2018).
- Goldstein BH, Aiyagari R, Bocks ML, et al. Hydrogel Expandable Coils for Vascular Occlusion in Congenital Cardiovascular Disease: A Single Center Experience. Congenit Heart Dis. 7: 212-218 (2012).
- McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A scientific Statement for Health Professionals from the American Heart Association. Circulation. 135: e927-e999 (2017).