Research Article - Clinical Practice (2018) Volume 15, Issue 5
Transcutaneous electrical nerve stimulation in acute versus chronic low back pain
Mohamed Ali Bakry1*, Mohamed Elhassaini Abdelghafar Yousef2, Hisham Mohamed Mohamed Salem21Department of Anesthesiology, Faculty of Medicine, Cairo University
2Department of Anesthesia, Research Institute of Ophthalmology, Egypt
- Corresponding Author:
- Mohamed Ali Bakry
Department of Anesthesiology
Faculty of Medicine, Cairo University
E-mail: mab628@kasralainy.edu.eg
Abstract
Objective: Low back pain (LBP) is a common disabling health problem. We aimed to compare the efficacy of using transcutaneous electric stimulation (TENS) in alleviating pain and restoring function in patients with acute versus chronic LBP. Subjects and Methods: The patients were divided into two groups acute and chronic, (n=50 in each). TENS was applied for a total of 10 sessions over a period of 2 weeks. Activity and resting visual analog scale (VAS) for low back pain, Roland Morris Disability Questionnaire (RDQ) and Oswestry Disability Index (ODI) and hand finger floor distance (HFFD) values were recorded at baseline and at one month after therapy. Results: Improvement in both groups after one month of use was observed in activity and resting VAS scores, as well as RDQ scores (p < 0.05, more in the chronic group). Improvement in ODI and HFFD was only noted in the chronic group (p < 0.05). Conclusion: TENS use is more beneficial in patients with chronic compared to acute LBP especially when it comes to physical function.
Keywords
transcutaneous electric stimulation, acute and chronic low back pain
Introduction
Low back pain (LBP) is a very common and disabling musculoskeletal disorder affecting patients of all age groups [1]. Based on duration of symptom, LBP is categorized into acute; lasting less than six weeks, subacute lasting for 6-12 weeks and chronic; longer than 12 weeks [2]. As LBP is extremely common, the disability caused by it represents a major economic burden both on the patient and society especially in chronic cases [1]. In the past the general view was that acute LBP is less of a burden as it usually has a relatively good prognosis, independent of the chosen treatment [3]. Recent studies however suggest this is not the case with frequent relapses and persistence of symptoms at one year in up to 10–30% of acute cases and recovery within 12 months in more than 30% of chronic cases [4-7].
There are many methods used for the management of acute and chronic LBP most of which are conservative such as physical therapy, medication and injections [8]. Transcutaneous electrical nerve stimulation (TENS) is a well established, safe and easy to use modality that utilizes an analgesic current to treat the pain associated with various musculoskeletal conditions [9-17]. Despite its well documented effect, there are very few studies investigating its utility in acute LBP with conflicting evidence. More supportive evidence exists for treatment of chronic LBP but again this is not supported by some studies [18].
The aim of the current study was to systematically investigate the effect of using TENS on pain and physical functions in patients presenting with acute versus chronic LBP.
Methods
This is a single centred observational study conducted in the outpatient pain clinic of a large community-based hospital in Cairo. Patients are referred to this clinic from orthopaedic doctors, neurologists and neurosurgeons from their respective clinics. Patients with low back pain were seen and when TENS use was deemed the appropriate means of management for their symptoms, they were further screened for suitability to be enrolled in the study. Those patients were approached by the recruitment officer and their measures were recorded.
Participants
The study populations were divided into two groups. “Acute Group”, defined as patients presenting with sudden symptoms of low back pain within the preceding 2-4 weeks and “Chronic Group”, defined as patients with persistent low back pain for longer than 12 weeks. The participants were consecutively recruited until a total of 50 patients who completed all the phases of the study was included in each group. This sample size was defined based on previous studies comparing the utility of TENS and other pain management modalities. The number was derived using their data, standard deviations and using a probability level of 0.05, with a power calculation of 90%.
Inclusion criteria
(a) Age>18 years and (b) pain localized between the inferior gluteal fold and the costal margin.
Exclusion criteria
(a) history of spine surgery (b) history of use of epidural or intramuscular corticosteroid injection (c) currently taking major painkillers or muscle relaxants (d) presence of skin ulceration on the back, (e) presence of any associated neurological condition, (f) pregnancy (g) presence of health problems such as malignancy, infection, fracture or an inflammatory disorder.
Patients taking mild analgesic oral drugs such as paracetamol were included, but all participants were generally discouraged from taking analgesics for the duration of the study.
Breakthrough pain was managed by nonsteroidal anti-inflammatory drugs (diclofenac sodium) to control the pain.
The study was approved by the local ethics committee and informed written consent was obtained from each patient.
Transcutaneous electric stimulation (TENS)
A standardized treatment protocol was implemented for each participant in each group [19]. This involved a total of 10 sessions of the therapy applied for 2 weeks (5 days/week). TENS consisted of the placement of two patches on the skin on the lumbar spine for 30 min. Using two electrodes, a premixed amplitude-modulated, conventional, frequency of 100 Hz was applied at 60 μs pulse width and intensity adjusted according to the threshold for each individual without causing pain or muscular contraction. The electrodes were placed crosswise in the paravertebral region.
The primary outcomes were evaluated for each group using activity and resting visual analog scale (VAS) for low back pain, Roland Morris Disability Questionnaire (RDQ) and Oswestry Disability Index (ODI) and hand finger floor distance (HFFD) values recorded at baseline (at the time they were recruited, prior to starting TENS use) and at one month after the therapy programs.
Statistical analysis
Descriptive statistical analysis was used and the results are presented as mean ± SD. The t-test was used for comparison of continuous variables between the two groups and the Chi-square test or the Fisher’s exact test was used for categorical variables. Pearson’s correlation was used to explore relationships between quantitative variables. Before and after treatment results were evaluated through paired sample t-tests. A twosided P < 0.05 was considered significant for all comparisons.
Results
As summarized in TABLE 1, there were no significant differences between the groups in respect of demographic data, associated symptoms such as radicular pain or pain characteristics. There was also no difference between the two groups with respect to number of patients taking mild analgesics (n= 31 in the acute group and n=26 in the chronic group) or those who experienced break through pain (n=19 in the acute group and n=14 in the chronic group) during the study time.
| Acute Group (n = 50) | Chronic Group (n = 50) | |
|---|---|---|
| Age (years) | 49.3 ± 11.7 | 52.0 ± 8.3 |
| Gender (M/F) | 24/26 | 20/30 |
| Disease duration (weeks) | 1.3 ± 0.1 | 145.6 ± 21.3 |
| BMI (kg/m2) | 27.3 ± 4.2 | 27.8 ± 4.5 |
| Associated radicular pain (%) | 65 | 52 |
| VAS activity | 7.4 ± 2.0 | 7.3 ± 1.7 |
| VAS resting | 6.8 ± 2.3 | 6.6± 2.1 |
| RDQ | 17.7 ± 6.3 | 16.9 ± 5.1 |
| ODI | 21.2 ± 13.4 | 19.1 ± 12.0 |
| HFFD (cm) | 7.1 ± 2.4 | 6.3 ± 3.7 |
Table 1. Demographic and clinical features and pain characteristics of the groups at baseline.
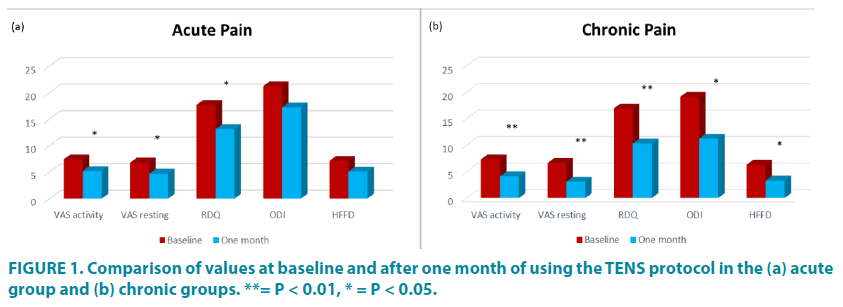
The results presented in TABLE 2 and FIGURE 1 show that there is significant improvement in both groups after one month of TENS use in activity and resting VAS scores, as well as RDQ scores (p < 0.05 in the acute group and p < 0.01 in the chronic group), however significant improvement in ODI and HFFD was only noted in the chronic group (p < 0.05).
| Acute Group (n = 50) | Chronic Group (n = 50) | |
|---|---|---|
| VAS activity | 5.2 ± 2.1 | 4.1 ± 2.0 |
| VAS resting | 4.7 ± 1.9 | 3.1 ± 1.4 |
| RDQ | 13.1 ± 14.6 | 10.4 ± 4.1 |
| ODI | 17.2 ± 11.0 | 11.2 ± 4.6 |
| HFFD (cm) | 5.1 ± 4.2 | 3.3 ± 1.2 |
Table 2. Values after one month of using the TENS protocol in each group.
When comparing the outcomes after one month of TENS between the two groups, a significant difference was found in the HFFD and ODI values (p < 0.05) but not in VAS activity and resting or in RDQ (TABLE 2).
Discussion
In the current study we performed a detailed comparison of the effect of using TENS on pain and physical functions in patients with acute and chronic LBP. There are very limited reports describing outcomes with TENS in acute lumbar pain with conflicting results [19] and while there is a larger number of studies in chronic pain, most of which describe the beneficial effect of TENS [20-22], there are data suggesting otherwise [18,23]. To our knowledge our study is the first study to systematically compare the efficacy of using TENS in acute versus chronic lumbar pain. Our results show that the use of TENS is very helpful in reducing pain in both acute and chronic LBP while its value in improving functionality is more in patients with chronic pain, being less helpful in the acute setting.
The severity of LBP plays a major role in determining the degree of functional disability and loss of productivity that are associated with it [24]. This has major implications on daily living activities and causes many occupational and social difficulties. The good outcome in the current study is that significant effects on pain relief were observed in both the acute and chronic groups after one month of therapy. This indicates medium-term beneficial effects of TENS use on pain relief in patients with all types of LBP, though it is more advantageous in chronic pain. While the role of TENS in alleviating painful conditions including back pain is well documented, the mechanism by which electrical current decreases pain remains unknown. The main hypothesis postulates that it activates the large diameter afferent A-alpha nerve fibers, as TENS referentially stimulates the low-threshold A-alpha fibers [25]. The input through these nerves is presumed to either activate an intraneural network that leads to inhibition of nociceptive impulses supplied through the small C unmyelinated and alpha-D fibers pre-synaptically or post-synaptically or to directly inhibit the C fibers [26,27]. This effect on pain modulation does not seem to be directly related to endogenous opiates. Naloxone, an inhibitor of endogenous and exogenous opiates, failed to reverse the effect of high-frequency TENS in patients with acute and chronic pain [28]. Regardless of its exact mode of action, TENS therapy has been used to decrease acute postoperative pain in patients who have undergone lumbar spine operations [29] as well as patients with chronic pain from back conditions or neurogenic injuries [29,30]. On the other hand patients who have psychogenic pain usually have increased discomfort with TENS therapy [31].
No significant improvement was detected in ODI and HFFD tests in patients with acute LBP while a significant change was observed in the chronic group. Given that there was no difference in these scores at baseline between the groups, this suggests that TENS use is much more useful in restoring physical functions in patients with long standing pain. It maybe that the increased likelihood of muscle spasm and edema in the acute setting hinders or delays restoration of function. This is because the closer the electrodes are to the nerve, the lower the current required to stimulate the appropriate nerve fibers [29] and with increased tolerability and presumably better the efficacy.
Perhaps the main limitation of our study is that it was conducted in a single center and with a relatively short follow up period of one month. TENS, like other forms of pain therapy, has a significant placebo component [32]. In the early stages of therapy, it produces 60% to 80% relief of pain. The placebo effect portion of the response quickly falls off while the therapeutic efficacy of TENS decreases more slowly, so that between 20% and 30% continues to experience pain relief at one year [29]. This is why TENS is usually thought of as only a temporary therapy to be used while the patient tries to increase his or her physical status [32]. Whether this applies for our patients cannot be confirmed and would require longer periods of follow up than implemented in the current study. However, the aim of our study was to compare between efficacies of using TENS in acute versus chronic LBP pain. In that respect our findings do provide strong evidence to suggest that TENS use is much more beneficial in patients with chronic compared to acute LBP especially when it comes to physical function. This does not negate its value in controlling pain in both settings and thus can be a safe and cheap conservative therapy in patients with acute and chronic LBP.
Acknowledgements
The authors wish to thank the neurologists, orthopedic surgeons and general practitioners who referred patients and to their assistants Ms Fatima Mohamed and Ms Mariam Ibrahim for help with patient recruitment, management and testing as well as with data organization.
Disclosure
The authors do not have any conflict of interest or funding sources to disclose.
References
- Williams CM, Maher CG, Hancock MJ, et al. Low back pain and best practice care: a survey of general practice physicians. Intern. Med. 170, 271-277 (2010).
- van Tulder M, Becker A, Bekkering T. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur. Spine J. 15 (Suppl. 2):S169–S191 (2006).
- McCarberg BH. Acute back pain: benefits and risks of current treatments. Curr. Med. Res. Opin. 26(1), 179-190 (2010).
- Costa Lda C, Maher CG, McAuley JH, et al. Prognosis for patients with chronic low back pain: inception cohort study. BMJ. 339, b3829 (2009).
- Freburger JK, Holmes GM, Agans RP. The rising prevalence of chronic low back pain. Arch. Intern. Med. 169(3), 251-258 (2009).
- Henschke N, Maher CG, Refshauge KM, et al. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 337, a171 (2008).
- Stanton TR, Henschke N, Maher CG, et al. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine. 33(26), 2923-2928 (2008).
- Petering RC, Webb C. Treatment options for low back pain in athletes. Sports Health. 3(6), 550-555 (2011).
- Ratajczak B, Hawrylak A, Demidaś A, Kuciel-Lewandowska J, Boerner E. Effectiveness of diadynamic currents and transcutaneous electrical nerve stimulation in disc disease lumbar part of spine. J. Back Musculoskelet. Rehabil. 24(3), 155-159 (2011).
- Cole AJ, Farrel JP, Stratton SA. Cervical spine athletic injuries. Phys. Med. Rehabil. 5, 37-68 (1994).
- Johnson M, Martinson M. Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: a meta-analysis of randomized controlled trials. Pain. (1-2), 157-165 (2007).
- Vance CG, Dailey DL, Rakel BA, Sluka KA. Using TENS for pain control: the state of the evidence. Pain Manag. 4(3), 197-209 (2014).
- Johnson MI, Bjordal JM. Transcutaneous electrical nerve stimulation for the management of painful conditions: focus on neuropathic pain. Expert Rev. Neurother. 11(5), 735-775 (2011).
- Khadilkar A, Odebiyi DO, Brosseau L, Wells GA. Transcutaneous electrical nerve stimulation (TENS) versus placebo for chronic low-back pain. Cochrane Database Syst. Rev. 8(4), CD003008 (2008).
- Jensen I, Harms-Ringdahl K. Strategies for prevention and management of musculoskeletal conditions. Neck pain. Best. Pract. Res. Clin. Rheumatol. 21(1), 93-108 (2007).
- Sluka KA, Lisi TL, Westlund KN. Increased release of serotonin in the spinal cord during low, but not high, frequency transcutaneous electric nerve stimulation in rats with joint inflammation. Arch. Phys. Med. Rehabil. 87(8), 1137-1140 (2006).
- Topuz O, Özfidan E, Ozgen M, Ardic F. Efficacy of transcutaneous electrical nerve stimulation and percutaneous neuromodulation therapy in chronic low back pain. J. Back Musculoskelet. Rehabilitation. 1(17), 127-133 (2004).
- van Tulder MW, Waddell G. Conservative treatment of acute and subacute low back pain, in Nachemson AL, Jonsson E (eds): Neck and Back Pain: The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia, PA: Lippincott Williams & Wilkins, 241-269 (2000).
- Selcuk Sayilir S, Yildizgoren MT. The medium-term effects of diadynamic currents in chronic low back pain; TENS versus diadynamic currents: A randomised, follow-up study. Complement Ther. Clin. Pract. 29, 16-19 (2017).
- Koldas Dogan SK, Tur BS, Kurtais Y, Atay MB. Comparison of three different approaches in the treatment of chronic low back pain. Clin. Rheumatol. 27, 873-881 (2008).
- Grabiańska E, Leśniewicz J, Pieszyński I, Kostka J. Comparison of the analgesic effect of interferential current (IFC) and TENS in patients with low back pain. Wiad. Lek. 68(1), 13-19 (2015).
- Jarzem PF, Harvey EJ, Arcaro N, Kaczorowski J. Transcutaneous electrical nerve stimulation (TENS) for chronic low back pain. J. Musculoskelet. Pain.13, 3-8 (2005).
- Van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions forchronic non-specific low back pain. Eur. Spine J. 20, 19-39 (2011).
- Waddell G, Waddell H. A review of social influences on neck and back pain and disability. In Nachemson AL, and Jonsson E. (eds): Neck and Back Pain. Philadelphia: Lippincott Williams & Wilkins, (2000).
- Bloedel J, McCreery D. Organization of peripheral and central pain pathways. Surg. Neurol. 4(1), 65-81 (1975).
- Campbell JN, Taub A. Local analgesia from percutaneous electrical stimulation. Arch. Neurol. 28(5), 347-350 (1973).
- Woolf CJ. Transcutaneous and implanted nerve stimulation. In Wall PD, Melzack R (eds): Textbook of Pain. Edinburgh, Churchill Livingstone, 679-690 (1986).
- Abrams SE, Reynolds AC, Cusick JF. Failure of naloxone to reverse analgesia from transcutaneous electrical stimulation in patients with chronic pain. Anaesth. Analg. 60(2), 81-84 (1981).
- Bates JAV, Nathan PW. Transcutaneous electrical nerve stimulation for chronic pain. Anaesthesia. 35(8), 817-822 (1980).
- Cauthen JC, Renner EJ. Transcutaneous and peripheral nerve stimulation for chronic pain states. Surg. Neurol. 4(1), 102-104 (1975).
- Nielzen S, Sjolund BH, Eriksson MB. Psychiatric factors influencing the treatment of pain with peripheral conditioning stimulation. Pain. 13(4), 365-371 (1982).
- Thorsteinsson G, Stonnington HH, Stillwell GK. The placebo effect of transcutaneous electrical stimulation. Pain. 5(1), 31-41 (1978).