Review Article - Interventional Cardiology (2011) Volume 3, Issue 3
Transradial angioplasty for STelevation myocardial infarction
- Corresponding Author:
- David Meerkin
Department of Cardiology, Shaare Zedek Medical Center
Jerusalem, Israel
Tel: +972 2655 5975
Fax: +972 2655 5437
E-mail: meerkin@szmc.org.il
Abstract
Keywords
access site complication, cardiac catheterization, major bleeding, primary PCI, ST-elevation MI, transradial
Since the widespread introduction of cardiac catheterization using the Judkins technique, the transfemoral approach has been the mainstay in cardiac catheterization. Coronary catheterization using the transradial approach has progressed significantly, technically as well as with widespread application and popularity, since it was first described by Campeau in 1989 [1]. Initially, it was used for diagnostic procedures. In 1993, Kiemeneij described its application for interventional procedures [2]. The last decade has been witness to a progressive worldwide expansion of this approach. Most operators adopting this technique have initiated their experience with stable patients undergoing elective procedures [3–5]. However, over the last decade, an increased number of patients with acute coronary syndrome, including ST-elevation myocardial infarction (STEMI), have undergone primary percutaneous coronary interventions (PCIs) with this approach [6–11]. In an era of aggressive and prolonged antiplatelet and antithrombotic regimens, bleeding has emerged as one of the most important prognostic factors in the outcome of patients suffering acute coronary syndromes and particularly STEMI [12,13]. In recent years evidence has accumulated to suggest that in experienced hands, transradial PCI offers significant advantages to patients, in particular, lowering bleeding rates and access site-related complications with a resultant morbidity benefit [6,11,14]. There are a few small randomized prospective trials comparing interventions from the radial with the traditional femoral approach in terms of success rate and morbidity, none of which are powered to demonstrate a mortality benefit [6–11]. Most of the data has been generated from registries or case series. In this article we focus upon patients admitted with STEMI with particular emphasis on data comparing the radial and femoral approaches in primary PCI.
Prevalence and geographical penetration
Owing to disparate penetration and the initial absence of randomized trials comparing the transradial to the transfemoral approach, a significant geographical diversity has developed not only between countries but also between proximate interventional centers. By assessing different reported studies this disparity becomes obvious. Approximately 20% of the PCIs during the years 1999–2005 in British Colombia were performed using the transradial approach as reported at the British Columbia Cardiac Registry. The ratios remain the same among the patients that were included in the MORTAL trial over the same years. The study includes prospectively collected data from approximately 38,872 procedures performed in four major centers. Of these, 7972 were performed using the transradial approach with 90% of them performed in only one of the four centers that participated in that study [15]. Two thirds of the patients were classified as urgent or emergency. In comparison, in the USA, only 1.3% of the total PCIs were reported to be performed using the radial approach [16]. Of these, non- STEMI acute coronary syndrome and STEMI were the indications for referral for interventions in 50 and 3% of patients, respectively. A recent observational study from a single center in the UK demonstrates the adoption trend of the radial approach as the access site of choice for interventions in acute myocardial infarctions [14]. Of the 1051 primary PCIs performed between 2004 and 2008, the selected access site was radial in 55% of cases. However, when the study was commenced, the radial approach was the site of choice in only 20% of cases, escalating to 80% by the same operators 4 years later. In China, 60% of coronary angiography and 56% of PCI procedures were perfomed via the radial approach in 2007 [17].
It is clear from the variety of reports from across the globe that the penetration of the transradial approach for coronary angiography, PCI and particularly primary PCI is heterogeneous. Despite this, the trends are of increasing numbers, with the USA being an area of slower adoption but of increasing interest as witnessed by the development of new courses such as those offered by the Society of Cardiovascular Angiography and Intervention, and the promise of interventionalists to increase the proportion of transradial cases within their practices.
Success rates
The crucial issues raised regarding the adoption of any novel technique are what are the benefits and at what expense are these achieved. The benefits of the transradial approach to PCI are generally claimed to be reduced complication rates and earlier ambulation as will be discussed later. The concern of many interventionalists is: does this come at the expense of our current standard excellent success rate?
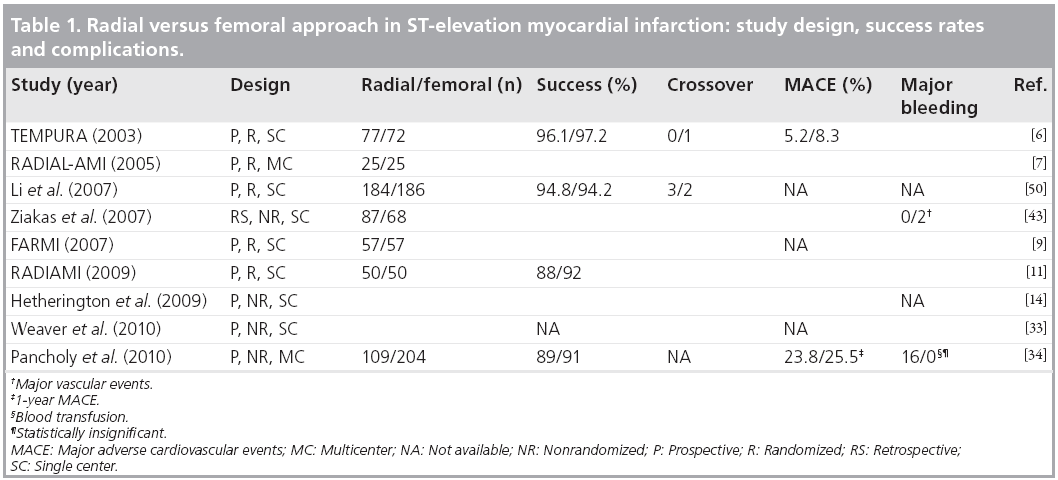
The TEMPURA trial published in 2003 was the first to prospectively compare transradial to transfemoral access in the setting of primary PCI for STEMI [6]. The study was performed at a single center where the default approach was radial. Subsequently, a number of additional small trials were performed comparing the two approaches [7,9,11]. Conversely, in these studies, the operators’ prestudy default had been the transfemoral approach. Overall, the success rates of transradial PCI in STEMI are very high in all the trials and are not inferior to that of the transfemoral approach (Table 1). Patient selection and crossover rates are important variables that need to be considered when comparing the success rate of the two methods in the different trials. The success rates in the TEMPURA trial were 96.1 and 97.1% in the radial-PCI (r-PCI) and femoral-PCI (f-PCI) groups, respectively [6]. In RADIAL-AMI [7], a small Canadian multicenter randomized pilot trial that enrolled 50 patients, and the FARMI trial [9], a single-center randomized trial with a total of 114 patients, the intention-to-treat success rates were equivalent. In a meta-analysis published in 2009, Jolly et al. included 23 studies comparing the radial to the femoral approach for catheterization [18]. The population studied was diverse and although including some patients who underwent primary or rescue catheterization, the majority were electively treated patients. They neutralized cases of access failure in order to specifically assess the number of cases in which the procedure failed because of an inability to open the target coronary artery. There was a trend toward higher failure rate with the radial approach (4.7% r-PCI vs 3.4% f-PCI; p = 0.2). However, in those studies performed by experienced transradial interventionalists, the failure rates were similar with a p-value of 0.44, reinforcing the fact that in skilled hands there were similar success rates. Another meta-analysis published recently included only studies that focused on urgent catheterization, for instance, primary or rescue PCIs [19]. This article included 12 studies and a total of 3324 patients between 2002 and 2009. No difference was found in the success rates or the length of the procedure between the two methods. In summary, the success rates of the two approaches appear similar in both elective and urgent patients, provided the procedure is performed by an experienced operator.
Table 1: Radial versus femoral approach in ST-elevation myocardial infarction: study design, success rates and complications.
Crossover
Success rates may be alternatively represented as success in achieving a patent vessel from the selected or predetermined access site, or whether successful revascularization was achieved irrespective of the final access used. The anatomical differences between the radial and femoral arteries indicate that the approach to each access site be distinct and site specific. Furthermore, the anatomical variations of the radial artery, its smaller caliber, the area it supplies and the competency of the palmer arches, necessitate more attention prior to puncture, during wiring, sheath insertion and catheter passage to the ascending aorta. Additionally, the radial artery is more prone to spasm, a feature that necessitates judicious use of spasmolytics [20], as well as minimizing vessel trauma and avoidance of catheter/sheath to vessel mismatch. Concern has been expressed about the limitation of guide catheter size to be used in the radial artery. This issue has been well addressed by the continuous miniaturization that has occurred in angioplasty equipment. The vast majority of transfemoral procedures are performed in 6F guide catheters and these are appropriate for radial use in the majority of patients. This approach has been adopted by the majority of centers commencing their transradial experience. Most cases, however, can be performed in 5F and as such many centers have adopted this size for standard angioplasty from the radial approach. Some specialized transradial centers have adopted specialized guiding catheters such as the Asahi Sheathless system (Asahi Intecc, Japan), allowing for larger bore catheters with smaller puncture sites and excellent hydrophilicity, all of which contribute to less radial arterial trauma [21]. This in turn reduces spasm and theoretically should contribute to improved long-term patency. The combination of the need for rapid reperfusion, a small vessel and the potential requirement for 6 or 7F has dissuaded many interventionalists from adopting the radial approach in STEMI where complex bifurcations may be uncovered or where significant thrombus load may require the use of aspiration thrombectomy or protection devices. This same constellation of primary PCI results in operators having less patience before abandoning the transradial approach and crossing over to the transfemoral approach in attempts to reduce door-to-balloon times.
Crossover rates in primary PCI have varied between 0 and 12% in different reports (Table 1). In the TEMPURA study there were no crossovers from the radial to the femoral approach [6]. There was, however, a single crossover from femoral to radial. A single radial to femoral crossover of 25 primary PCIs was reported in the pilot study RADIAL-AMI. This occurred owing to failure to cannulate the radial artery. However, in the FARMI trial, crossovers were far more frequent with 7 out of 57 (12%) instances, all occurring at the diagnostic stage [9]. Each of the operators in these two trials had experience of greater than 100 cases of transradial PCI prior to enrolling patients in the trial. Four out of 50 patients in the radial arm of the RADIAMI trial crossed over to femoral approach, three of them due to positive Allen tests [11]. Similar patients were excluded from randomization in most of the other trials, such that radial failure or crossover rates remain similar. Crossover rates in a recent meta-analysis were divided into two categories: inability to cannulate the access artery and procedural failure due to inability to open the coronary artery after successful cannulation. Access site cannulation failure was significantly higher with the radial approach. Following arterial cannulation, success rates were similar with a slight trend to the femoral approach [18]. In a meta-analysis that focused on urgent catheterization, crossover rates were significantly higher using the radial approach [19]. Most operators prefer right radial artery access as the access site of choice. Some use the left radial artery when they expect technical difficulties with the right radial approach, as is the case in patients with an in situ left internal mammary graft. A comparison of left and right radial approaches reached inconclusive results with respect to success rates and procedural times. While in most studies the right radial approach was the default approach for radial access [22], other studies indicate left radial access superiority [23,24]. A retrospective analysis of 135 STEMI patients, 85 from the right radial artery and 50 from the left, revealed that there was no difference between the groups in terms of procedural success, length or complications [25].
There is no doubt that the additional technical challenges that the interventionalist faces from the transradial approach have significant impact at the early stages of the learning curve. As the interventionalist generates greater experience, the necessity to crossover to the femoral approach becomes a rare event. Additionally, the transradialist has little concern in crossing over to the femoral technique when this is necessary, however, the majority of operators not skilled in the transradial technique have limited options when faced with insurmountable obstacles during the a priori decision to adopt the femoral approach, particularly during primary PCI where time is of the essence.
Access site complications
Current increasing use of antiplatelet and antithrombotic agents has dramatically reduced post- PCI ischemic events [26,27]. Their widespread use on the one hand, and the miniaturization of the equipment on the other, have resulted in a reduction of access site complication frequency, but with an associated potential increase in the bleeding severity of individual cases. In fact, when taking into account traditional major adverse cardiovascular events (MACE) and bleeding, the effect of bleeding is almost as important as postprocedural ischemia, particularly periand post-procedural access site bleeding [12]. A greater than twofold reduction in major access site bleeding rates in the femoral PCI approach was demonstrated in a single center retrospective study spanning 1994 to 2005 [28]. Brendan et al. reported a significant reduction, from 8.4% between 1994 and 1995 to 3.5% between 2000 and 2005, respectively. These changes were attributed to the use of smaller sheath sizes, a reduction in the postprocedural anticoagulation treatment and procedural duration. A total of 60–70% of the patients in that study were reported as having undergone urgent or emergency PCI. Interestingly, there was no significant difference in the major bleeding rates between these acute patients and the elective patients, contrary to what may have been expected.
Although the bleeding rate from the femoral approach has reduced significantly over recent years, it remains a troublesome issue. In a singlecenter prospective study that included 1703 PCIs performed for a variety of indications, including 15% of STEMI, a significantly lower rate of major bleeding events was reported in men when compared with women treated using the femoral approach [29]. This difference was not apparent in patients treated using the radial approach, owing to an extremely low bleeding rate (0.06%). Of all patients treated using the transradial approach in this study, only a single case of major bleeding was noted. Gender, peripheral arterial disease, older age, IIB/IIIA usage and the urgency of the procedure were all found to be related to bleeding tendency and access site complication, each of which were significantly reduced by the use of transradial access. STEMI patients treated with abciximab had significantly lower access site complications with the radial compared with the femoral approach as evident from the recently published EUROTRANSFER registry [30]. There were significantly lower access site complications among patients suffering from peripheral arterial disease who underwent primary PCI using the radial approach [31]. In the previously described registry from the USA, only 3% were STEMI patients. The procedural success rates were equal, however, a significant reduction in access site bleeding and complications were noted [16]. In the PREVAIL study, in which approximately 10% of the procedures performed were primary PCI, the major bleeding rate was exceptionally low at 0.4%. Intention-totreat total bleeding rate was not statistically different between both arms, but was statistically lower in the radial group in per treatment analysis [32]. In studies that included only primary PCIs, there was a trend toward lower bleeding rate in patients treated with the radial approach. In view of the small patient numbers included in these studies and a resultant lack of power to detect such differences, reduction of bleeding rates with the radial approach did not achieve statistical significance in most of the trials. In the FARMI trial, in which 114 STEMI patients were randomized, there were three major bleeding events in each group in the intention-to-treat analysis [9]. However, all of the cases of major bleeding in the radial approach group occurred following crossover to the femoral approach, such that in a per-protocol assessment, there were no transradial vascular complications. Weaver reported a trial specifically designed to assess the time taken to flow restitution with primary PCI in the radial approach when compared with the femoral approach [33]. There were seven out of 124 (5.7%) cases of access site major bleeds in the radial group as compared with 16 out of 116 (13.8%) in the femoral group (p = 0.05). In another study on a primary or rescue PCI population, patients older than 70 years of age demonstrated lower radial access site major bleeding (none of 87) when compared with the femoral approach (two out of 68). Pancholy et al. reported significantly higher access site complications in patients treated with femoral primary PCIs (20 events in 204 patients) as compared with transradially treated patients (one event in 109 patients) with 16 requiring blood transfusions as opposed to none in the radial group [34]. A retrospective analysis of 582 STEMI patients demonstrated significant lower major and minor access site complications among patients treated by the radial approach compared with the femoral approach. In fact, there were no major access site complications in the radial primary PCI group compared with 5% at the femoral primary PCI group (p < 0.05). MACE rates were also significantly reduced in the radial group (4 vs 11%, respectively; p < 0.05) [35].
The negative prognostic implications of peri- and postprocedural bleeding are well established in the literature, particularly their association with an increased mortality rate [12,28,36–38]. There are many theories that try to explain the high mortality rates among patients that had major bleeding, particularly among those requiring blood transfusion. Early cessation of antiplatelet therapy and hemodynamic changes may only be part of the explanation. Additionally, there is evidence that stored blood has proinflammatory and prothrombotic effects [39], increased red blood cell viscosity, a tendency to aggregate [40] and impaired vasodilatory effects due to reduced NO [41]. All these factors may contribute to the poorer outcome amongst bleeding patients.
Based upon this, it seems likely that the radial approach to primary PCI would result in lower mortality rates due to lower access site major bleeding. It is important to note, however, that to date no study has demonstrated a decrease in mortality among radial approach primary PCI patients when compared with the femoral approach. Although not specific to primary PCI, the MORTAL study demonstrated mortality benefit in the radial group compared with the femoral group for the first time [15]. In this study, data was gathered prospectively from four highvolume centers. Extremely elevated mortality rates were noted in the patients that required blood transfusion. Transfused patients had mortality rates of 12.6 and 22.9% at 30 days and at 1 year, whereas in the patients not requiring transfusions, the 30-day and 1-year mortality rates were 1.3 and 3.2%, respectively, findings that are consistent with previous studies. 30-day mortality rates were 1 and 1.7%, with 1-year mortality rates of 2.8 and 3.9% for the radial versus femoral approaches, respectively (p < 0.01). It was calculated that the prevention of 15 blood transfusions would result in the saving of one patient life.
In order to further elucidate this issue, a number of meta-analyses were performed assessing access site outcomes. In the first, published in 2004, Agostoni et al. included 12 studies that compared the radial to the femoral approach in 3224 patients [42]. Predominantly ambulatory patients were studied, with only a single study including STEMI patients. The access site complications with the radial approach were much lower when compared with the femoral approach, however, at the expense of a slightly lower success rate but with an equivalent MACE rate. In a more recent meta-analysis that included 23 randomized trials with 7020 patients of which a significantly higher percentage of patients suffered acute coronary syndromes including STEMI, a 73% reduction in major bleeding was noted in the transradial group (odds ratio: 0.27; 95% CI: 0.16–0.45; p < 0.001) [18]. It also demonstrated a trend toward a lower MACE rate and mortality in the radial group.
Most recently, a meta-analysis specifically comparing the use of the transradial to the transfemoral approach in primary and rescue PCI for STEMI was published [19]. It included 3324 patients from five randomized trials and seven observational studies. The radial approach reduced the risk of major bleeding by 70%, with an associated reduction of the composite end point of death, MI and stroke (3.65 vs 6.55%; odds ratio: 0.56; 95% CI: 0.39–0.79; p = 0.01). A definitive randomized study powered to assess a mortality benefit resulting from access site is necessary.
Time, radiation and contrast
The importance of rapidly restituting flow through the culprit lesion in STEMI has been demonstrated many times in the past. In most cases, the length of the procedure correlates directly with contrast medium volume used and the amount of radiation to which the patient and operator are exposed. Particularly with less experienced operators, access to the smaller caliber radial artery and coronary engagement may be more challenging. As such, the concern has been voiced that radial access procedures may be prolonged, with such differences more pronounced and more critical in STEMI patients than stable patients undergoing elective PCI. It is also reasonable to consider that an operator’s median procedure length will have direct correlation with crossover rates, MACE and access site complication, while an inverse correlation will be found with success rates. All of these outcomes should be dependent upon the operator’s experience with the radial approach.
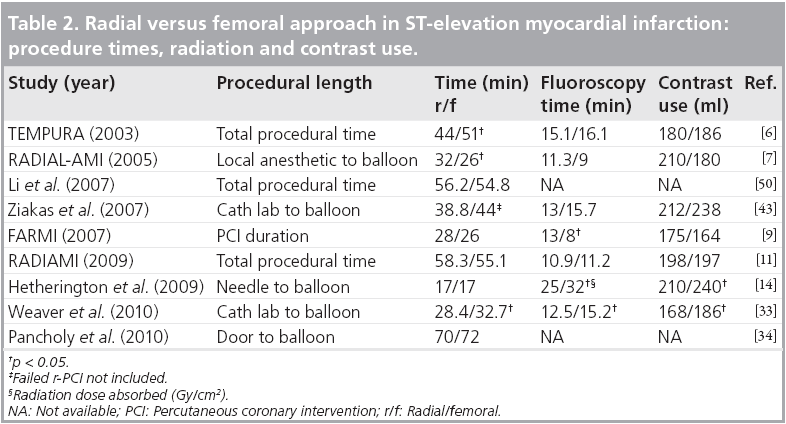
In a recent meta-analysis that included urgent patients as well as ambulatory patients [18], the mean procedure time was 3.1 min longer in the radial patients than those treated via the femoral route. The authors conjecture that the diversity in procedural length between the different trials was predominantly dependent upon the operator’s experience. The mean time for r-PCI was 1.7 min longer than f-PCI in the hands of operators that have great experience in PCIs using the radial approach compared with 4.7 min in nonradial experts. Radiation exposure was also greater with the transradial approach, as estimated by fluoroscopy time. In the TEMPURA trial, the procedural lengths, the amount of contrast and fluoroscopy time were all lower in the r-PCI compared with the femoral PCIs (Table 2) [6]. Procedure time was 44 ± 18 versus 51 ± 21 min (p = 0.033) in the radial versus the femoral approach, respectively. The contrast volume used and the fluoroscopy time were lower in the radial group, but this difference did not attain statistical significance.
Table 2: Radial versus femoral approach in ST-elevation myocardial infarction: procedure times, radiation and contrast use.
Conversely, in the RADIAL-AMI trial, the contrast use and fluoroscopy time were greater in the radial primary PCIs [7]. In this study, in an attempt to more closely determine the effects of different components of procedural length with particular emphasis on minimizing door-toballoon time in STEMI patients, the procedure time was divided into several segments. The time from local anesthetic injection to first balloon inflation was longer in the radial primary PCIs (32 min) when compared with the transfemoral PCIs (26 min; p = 0.04). These findings support the suppositions that for most operators the radial artery is more time consuming to puncture, and the passage to the coronary artery and catheter manipulations are more challenging compared with the femoral approach.
Several other trials have also demonstrated that the procedure time, fluoroscopy time and contrast medium volumes were greater when the radial approach was used, however, in most cases the differences were small and not statistically significant. In one study the procedural time was shorter in the radial approach but in that study seven patients in whom the radial approach failed, were excluded [43]. In the FARMI trial, the radial approach procedure took, on average, 6 min longer when compared with the femoral approach [9]. This prolongation is markedly longer than that found in most other trials and is probably associated with the high rates of failed procedures and crossover rates from the radial approach in this study.
Conversely, in a single-center US study, that compared door-to-balloon time between both access routes, the radial approach was on average 10 min shorter for the entire procedure [33]. This study examined the entire procedure and divided portions of the procedure into timed segments. When looking at the procedural segments that were specifically related to the access site such as case commencement to balloon inflation, the radial approach was slightly faster, 30.8 min in the radial group versus 34.6 min in the femoral group. Another recent single-center study from the USA compared door-to-balloon time in primary PCI, in which 313 patients were divided into two groups, 204 in the femoral group and 109 in the radial group. Five operators participated in this study, with two radial experts and three femoral experts. The door-to-balloon time was not significantly different, with trend to shorter time with the radial access approach [34].
In summary, in current day practice some prolongation of procedural time may be noted in some centers, particularly those centers with limited transradial experience. However, in most studies the difference is minimal without any significant difference in contrast material volume or fluoroscopy time used. The nursing aspects requiring preparation and draping of both the radial and femoral sites as well as the puncturing of the smaller vessel, make it likely that a small time delay will remain with the radial approach. This has led some operators to suggest not draping the groin at all, but this remains controversial. It seems inevitable that as more operators and laboratory staff develop greater experience in the transradial approach, these differences will minimize such that its differential impact on MACE will be negligible.
MACE
The effects of access site on MACE rates are multifactorial, based upon a combination of success rates, complications and procedural delays. There was no difference in either in-hospital or 6-month MACE rates between the two arms (transradial and transfemoral) in the randomized TEMPURA trial [6]. More than half of the patients underwent repeat angiography within 6 months after first admission, which demonstrated no difference between target vessel diameters between the two groups. The majority of primary PCI trials demonstrated no significant difference in MACE rates in the radial group compared with the femoral group, but none of these trials was large enough or adequately powered to distinguish such a difference (Table 1).
In a meta-analysis by Vorobcsuk et al., 12 studies were included in the MACE rate calculation [19]. Most of these individual studies demonstrated trends to reduce MACE rates with radial access without demonstrating statistical significance. In the meta-analysis, however, a significant MACE benefit in favor of radial access was clearly demonstrated.
Early ambulation and discharge
Competent management of arterial access sheaths and their removal represent major steps towards the reduction of bleeding complications. Traditionally, removal of the femoral sheath is delayed post-PCI for a number of hours to allow normalization of coagulation following intra-procedural medication. It is then removed either empirically or following an assessment of coagulation by using some laboratory measures such as activated clotting time. In some centers, femoral sheaths are removed immediately on the table at the conclusion of the procedure by using a closure device. A number of these devices are available and have been shown on the whole to be effective at reducing time to ambulation but without reducing bleeding rates [44] and in some reports have even resulted in increased bleeding rates [45]. Conversely, when using the transradial approach, the sheath is removed immediately at the completion of the procedure and a compression device placed. This allows for immediate ambulation without the risk of increased bleeding rates.
Early ambulation allows for the early discharge of patients that have undergone PCI using the transradial approach with the additional advantage of lower costs due to shorter hospitalization. This is true particularly for ambulatory patients [46].
Patients admitted with acute myocardial infarction undergoing primary PCI, however, routinely remain hospitalized for a number of days; therefore the length of hospital stay is not directly influenced by the access site. It may, however be influenced by an associated hematoma and vascular complications. Early discharge was successful among 62% (62 out of 100) of patients admitted with acute myocardial infarction [27]. The patients were catheterized by the radial approach, underwent stent implantation and treated with tirofiban per protocol. In the TEMPURA trial, the investigators adopted an early discharge protocol, with planned discharge being on the third hospitalization day [6]. There are several scoring methods to assess the risk for adverse events after myocardial infarction, for instance, the CADILLAC score is a simple and popular choice [47]. Mean hospital stays were 5.7 and 7.4 days for the transradial and transfemoral approaches, respectively. Furthermore, discharge on day 3 was successful in 58.9% of the patients treated transradially with only 48.5% in the femoral approach group. Owing to the small study size these findings did not attain statistical significance (p < 0.204) nor did the reduction of hospitalization cost (p < 0.591).
In an additional single-center observational study with prospectively collected data, hospital stay was 2.46 days in the transradial group and 3.51 days in the transfemoral group (p < 0.001) [14]. In other studies, hospital stay was not different in other primary PCI trials [9,43].
In conclusion, following uncomplicated primary PCI for STEMI, hospital stay is mainly influenced by the underlying disease and not by access site. However, there are some data demonstrating a reduction of hospital stay in PCI centers with transfer back to referring centers within a few hours [48]. Nonetheless, the increasing popularity of early discharge protocols in association with the reduced incidence of access site complications when using the radial approach are likely to result in a difference in hospitalization length and cost when the two approaches are compared.
Conclusion
Recent years have seen a dramatic change in the access site of choice in some centers and countries. In most centers where the radial approach was adopted, it has become the default approach for primary PCIs as well. Excellent success rates have been demonstrated with the radial approach. Publications to date give the impression that once an operator has become familiar and expert with the radial approach in elective cases it soon progresses to become the access site of choice for urgent catheterizations. Success rates, equivalent radiation exposure and contrast doses compared with the femoral approach probably all contribute to this trend. In addition, the radial approach permits early ambulation with greater patient convenience. However, the most important benefit is the reduction of access site complications. While there is a trend toward lower MACE rates, small trial sizes with inadequate statistical power have probably resulted in an inability to demonstrate this conclusively. To date, the radial approach offers many real benefits, however, we are in need of larger studies, with the power to demonstrate significant benefits in morbidity and probably mortality with this technique.
Future perspective
The indications that we are getting from studies and meta-analyses are that the transradial approach for STEMI patients along with improved patient comfort affords outcome benefits, particularly those related to access site complications. These benefits may be potentially shown to result in MACE and mortality benefits in larger more statistically powerful studies. The RIVAL trial and a substudy from the CURRENT trial are both prospective, randomized trials that compare the radial approach to the femoral approach in acute coronary syndrome patients. The RIVAL study results were recently published and demonstrated no mortality benefit for the transradial approach in the total population [49]. A specific subanalysis of primary PCI in STEMI patients is ongoing and with the results of these and more studies over the next 5–10 years, we are confident that such benefits will be well established. This in turn will generate further momentum for the trend of broader adoption of the transradial technique across the globe. As we train a younger generation of interventionalists that are more ‘radial aware’ and we leave the issues related to learning curves and development of dedicated transradial equipment, we may well see the transradial approach become the predominant access site for primary PCI with well proven benefits, with reduced MACE and probably mortality.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
Primary transradial percutaneous coronary interventions (PCIs) compared with primary transfemoral PCIs: success rate
▪ Equal and very high success rate in both approaches.
▪ Patients presenting with cardiogenic shock or after coronary artery bypass were excluded from most trials.
▪ Right radial approach is equal to the left radial approach in terms of success.
Primary transradial PCIs compared with primary transfemoral PCIs: crossover rates
▪ Higher in the radial approach compared with the femoral approach.
▪ Do not have significant impact on success rate in the intention-to-treat calculation.
▪ In inverse relation to the operator experience and are practically negligible in high volume, radial-oriented centers.
Primary transradial PCIs compared with primary transfemoral PCIs: access site complication
▪ Much higher in the femoral approach.
▪ Major access site bleeding almost eradicated with the radial approach.
▪ Although trends toward reduction in access site major bleeding exist, large randomized, prospective, multicenter studies are needed in order to demonstrate a significant difference and mortality benefit.
Primary transradial PCIs compared with primary transfemoral PCIs: patient safety & satisfaction
▪ Same amount of contrast use.
▪ Equal radiation exposure.
▪ Equal procedural length.
Primary transradial PCIs compared with primary transfemoral PCIs: major adverse cardiovascular event (MACE) rates
▪ Small trials demonstrate equal MACE rates in both approaches.
▪ Lack of large randomized trials that compare the two approaches in ST-elevation myocardial infarction.
▪ Single meta-analysis demonstrates significantly lower MACE in the radial approach.
Primary transradial PCIs compared with primary transfemoral PCIs: mobility
▪ Early ambulation due to immediate sheath extraction and excellent control on access site.
▪ No difference in hospitalization length in small trials.
References
Papers of special note have been highlighted as:
▪ of interest
- Campeau L: Percutaneous radial artery approach for coronary angiography. Cathet. Cardiovasc. Diagn. 16, 3–7 (1989).
- Kimeneij F, Laarman GJ: Percutaneous transradial artery approach for coronary stent implantation. Catheter Cardiovasc. Diagn. 30, 173–178 (1993).
- Grinfeld L, Berrocal D, Rojas Mata C et al.: What is the most effective vascular approach for a diagnostic cardiac catheterization? A randomized trial using the femoral, brachial or radial approach. J. Am. Coll. Cardiol. 27(Suppl. A), 901 (1996).
- Benit E, Missault L, Eeman T et al.: Brachial, radial, or femoral approach for elective Palmaz-Schatz stent implantation: a randomized comparison. Catheter Cardiovasc. Diagn. 41, 124–130 (1997).
- Kiemeneij F, Laarman GJ, Odekerken D et al.: A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the ACCESS study. J. Am. Coll. Cardiol. 29, 1269–1275 (1997).
- Saito S, Tanaka S, Hiroe Y et al.: Comparative study on transradial approach vs. transfemoral approach in primary stent implantation for patients with acute myocardial infarction: results of the test for myocardial infarction by prospective unicenter randomization for access sites (TEMPURA) trial. Catheter Cardiovasc. Interv. 59, 26–33 (2003).
- Cantor WJ, Puley G, Natarajan MK et al.: Radial versus femoral access for emergent percutaneous coronary intervention with adjunct glycoprotein IIb/IIIa inhibition in acute myocardial infarction – the RADIAL-AMI pilot randomized trial. Am. Heart J. 150, 543–539 (2005).
- Mann T, Cubeddu G, Bowen J et al.: Stenting in acute coronary syndromes: a comparison of radial versus femoral access sites. J. Am. Coll. Cardiol. 32, 572–576 (1998).
- Brasselet C, Tassan S, Nazeyrollas P et al.: Randomised comparison of femoral versus radial approach for percutaneous coronary intervention using abciximab in acute myocardial infarction: results of the FARMI trial. Heart 93, 1556–1561 (2007).
- Vazquez-Rodriguez JM, Calvino-Santos RA, Baz-Alonso JA et al.: Radial vs. femoral arterial access in emergent coronary interventions for acute myocardial infarction with ST segment elevation. J. Am. Coll. Cardiol. 49(Suppl. 2), 12B (2009).
- Chodor P, Kurek T, Sokal A et al.: Radial vs. femoral approaches for PCI for patients with acute myocardial infarction. The RADIAMI prospective, randomized, single center trial. Cardiol. J. 16, 332–340 (2009).
- Ndrepepa G, Berger PB, Mehilli J et al.: Peri-procedural bleeding and 1-year outcome after percutaneous coronary interventions: appropriateness of including bleeding as a component of a quadruple end point. J. Am. Coll. Cardiol. 51(7), 690–697 (2008).
- Feit F, Voeltz MD, Attubato MJ et al.: Predictors and impact of major hemorrhage on mortality following percutaneous coronary intervention from the REPLACE-2 trial. Am. J. Cardiol. 100, 1364–1369 (2007).
- Hetherington SL, Adam Z, Morley R et al.: Primary percutaneous coronary intervention for acute ST-segment elevation myocardial infarction: changing patterns of vascular access, radial versus femoral artery. Heart 95, 1612–1618 (2009).
- Chase AJ, Fretz EB, Warburton WP et al.: Association of the arterial access site at angioplasty with transfusion and mortality: the MORTAL study (Mortality benefit Of Reduced Transfusion after percutaneous coronary intervention via the Arm or Leg). Heart 94, 1019–1025 (2008).
- Rao SV, Ou FS, Wang TY et al.: Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the national cardiovascular data registry. J. Am. Coll. Cardiol. Intervent. 1, 379–386 (2008).
- Wang L, Yang Y, Zhou Y et al.: Prevalence of transradial coronary angiography and intervention in China: report from the transradial coronary intervention registration investigation in China (TRI-China). Int. J. Cardiol. 145(2), 246–247 (2009).
- Jolly S, Amlani S, Hamon M et al.: Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157, 132–140 (2009).
- Vorobcsuk A, Kónyi A, Aradi D et al.: Transradial versus transfemoral percutaneous coronary intervention in acute myocardial infarction systematic overview and metaanalysis. Am. Heart J. 158 814–821 (2009).
- Kiemeneij F, Vajifdar BU, Eccleshall SC et al.: Evaluation of a spasmolytic cocktail to prevent radial artery spasm during coronary procedures. Catheter Cardiovasc. Interv. 58, 281–284 (2003).
- Kiemeneij F, Fraser D, Slagboom T et al.: Hydrophilic coating aids radial sheath withdrawal and reduces patient discomfort following transradial coronary intervention: a randomized double-blind comparison of coated and uncoated sheaths. Catheter Cardiovasc. Interv. 59, 161–164 (2003).
- Bertrand OF, Rao SV, Pancholy P et al.: Transradial approach for coronary angiography and interventions: results of the first international transradial practice survey. JACC Cardiovasc. Interv. 3, 1022–1031 (2010).
- Kawashima O, Endoh N, Terashima M et al.: Effectiveness of right or left radial approach for coronary angiography. Catheter Cardiovasc. Interv. 61(3), 333–337 (2004).
- Sciahbasi A, Romagnoli E, Burzotta F et al.: Transradial approach (left vs right) and procedural times during percutaneous coronary procedures: TALENT study. Am. Heart J. 161(1), 172–179 (2011).
- Pyne CT: Comparison of procedural times, success rate and safety between left versus right radial arterial access in primary percutaneous coronary intervention for acute ST- segment elevation myocardial infarction. Catheter Cardiovasc. Interv. DOI: 10.1002/ ccd.22843 (2010) (Epub ahead of print).
- Montalescot G, Barragan P, Wittenberg O et al.: Abciximab before direct angioplasty and stenting in myocardial infarction regarding acute and long-term follow-up. Platelet glycoprotein IIb/IIIa inhibition with coronary stenting for acute myocardial infarction. N. Engl. J. Med. 344, 1895–1903 (2001).
- Dirksen MT, Ronner E, Laarman GJ et al.: Early discharge is feasible following primary percutaneous coronary intervention with transradial stent implantation under platelet glycoprotein IIb/IIIa receptor blockade. Results of the AGGRASTENT Trial. J. Invasive Cardiol. 17(10), 512–517 (2005).
- Doyle BJ, Ting HH, Bell MR et al.: Major femoral bleeding complications after percutaneous coronary intervention. Incidence, predictors, and impact on long-term survival among 17,901 patients treated at the Mayo Clinic from 1994 to 2005. J. Am. Coll. Cardiol. Intervent. 1, 202–209 (2008).
- Pristipino C, Pelliccia F, Granatelli A et al.: Comparison of access-related bleeding complications in women versus men undergoing percutaneous coronary catheterization using the radial versus femoral artery. Am. J. Cardiol. 99, 1216–1221 (2007).
- Siudak Z, Zawislak B, Dziewierz A et al.: Transradial approach in patients with ST-elevation myocardial infarction treated with abciximab results in fewer bleeding complications: data from EUROTRANSFER registry. Coron. Artery Dis. 21(5), 292–297 (2010).
- Jeremias A, Gruberg L, Patel J et al.: Effect of peripheral arterial disease on in-hospital outcomes after primary percutaneous coronary intervention for acute myocardial infarction. Am. J. Cardiol. 105(9), 1268–1271 (2010).
- Pristipino C, Trani C, Nazzaro MS et al.: Major improvement of percutaneous cardiovascular procedure outcomes with radial artery catheterization: results from the PREVAIL study. Heart 95, 476–482 (2009).
- Weaver AN, Henderson RA, Gilchrist IC et al.: Arterial access and door-to-balloon times for primary percutaneous coronary intervention in patients presenting with acute ST-elevation myocardial infarction. Catheter Cardiovasc. Interv. 75(5), 695–699 (2010).
- Pancholy S, Patel T, Sanghvi K, Thomas M et al.: Comparison of door-to-balloon times for primary PCI using transradial versus transfemoral approach. Catheter Cardiovasc. Interv. 75(7), 991–995 (2010).
- Ruzsa Z, Ungi I, Horváth T et al.: Five-year experience with transradial coronary angioplasty in ST-segment-elevation myocardial infarction. Cardiovasc. Revasc. Med. 10(2), 73–79 (2009).
- Eikelboom JW, Mehta SR, Anand SS et al.: Adverse impact of bleeding on prognosis in patients with acute coronary syndromes. Circulation 114, 774–782 (2006).
- Manoukian SV, Feit F, Mehran R et al.: Impact of major bleeding on 30-day mortality and clinical outcomes in patients with acute coronary syndromes: An analysis from the ACUITY Trial. J. Am. Coll. Cardiol. 49, 1362–1368 (2007).
- Stone GW, Witzenbichler B, Guagliumi G et al.: Bivalirudin during primary PCI in acute myocardial infarction. N. Engl. J. Med. 358, 2218–2230 (2008).
- Twomley KM, Rao SV, Becker RC: Proinflammatory, immunomodulating, and prothrombotic properties of anemia and red blood cell transfusions. J. Thromb. Thrombolysis 21, 167–174 (2006).
- Almac E, Ince C: The impact of storage on red cell function in blood transfusion. Best Pract. Res. Clin. Anaesthesiol. 21, 195–208 (2007).
- Reynolds JD, Ahearn GS, Angelo M et al.: S-nitrosohemoglobin deficiency: a mechanism for loss of physiological activity in banked blood. Proc. Natl Acad. Sci. USA 104, 17058–17062 (2007).
- Agostoni P, Biondi-Zoccai G, de Benedictis M et al.: Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures; systematic overview and meta-analysis of randomized trials. J. Am. Coll. Cardiol. 44, 349–356 (2004).
- Ziakas A, Gomma A, McDonald J et al.: A comparison of the radial and the femoral approaches in primary or rescue percutaneous coronary intervention for acute myocardial infarction in the elderly. Acute Card. Care. 9(2), 93–96 (2007).
- Deuling JH, Vermeulen RP, Anthonio RA et al.: Closure of the femoral artery after cardiac catheterization: a comparison of Angio-Seal, StarClose, and manual compression. Catheter Cardiovasc. Interv. 71(4), 518–523 (2008).
- Koreny M, Riedmüller E, Nikfardjam M et al.: Arterial puncture closing devices compared with standard manual compression after cardiac catheterization: systematic review and meta-analysis. JAMA 291(3), 350–357 (2004).
- Eichhofer J, Horlick E, Ivanov J et al.: Decreased complication rates using the transradial compared to the transfemoral approach in percutaneous coronary intervention in the era of routine stenting and glycoprotein platelet IIb/IIIa inhibitor use: a large single-center experience. Am. Heart J. 156, 864–870 (2008).
- Halkin A, Singh M, Nikolsky E et al.: Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. J. Am. Coll. Cardiol. 45(9), 1397–1405 (2005).
- Matteau A, Rinfret S, Dorais M et al.: The safety and feasibility of immediately returning patients transferred for primary percutaneous coronary intervention with ST-elevation myocardial infarction. EuroIntervention. 5(5), 599–603 (2009).
- Jolly S, Yusuf S, Cairns J et al.: Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377, 1409–1420 (2011).
- Li WM, Li Y, Zhao JY et al.: Safety and feasibility of emergent percutaneous coronary intervention with the transradial access in patients with acute myocardial infarction. Chin. Med. J. 120, 598–600 (2007).
▪ First randomized study that compared the transradial approach to the transfemoral approach in primary percutaneous coronary intervention and demonstrating equal success.
▪ Discusses the development and penetration of the the radial approach as demonstrated by the changing patterns of preferred access site over time.
▪ The only study that demonstrated mortality benefit of the radial approach compared with the femoral approach (not in primary percutaneous coronary intervention).
▪ The first meta-anlysis comparing radial with femoral access.