Review Article - Interventional Cardiology (2014) Volume 6, Issue 4
Transradial approaches in women and the elderly: deciphering the challenges and opportunities
- Corresponding Author:
- Adhir Shroff
Division of Cardiology, University of Illinois at Chicago, IL, USA
Tel: +1 312 996 6730
Fax: +1 312 413 2948
E-mail: arshroff@uic.edu
Abstract
Transradial versus transfemoral approach: complications • The transition from the classic transfemoral (TF) approach to a transradial (TR) approach is notable for a dramatic reduction of access-associated complications (AAC) including decreased medical costs, hospitalization fees and length of stay. • Despite the improvement in vascular access closure devices and the use of safer anticoagulants, the relative risk for AAC remains higher in both female patients and elderly patients regardless of method of entry. Complications in females • There is a significantly increased risk for vascular complications in females using the TF approach. • Specific complications include entry site bleeding, hematoma, and pseudoaneurysm formation. • The relative risk for access complications in females is augmented with larger sheath sizes. • Bleeding and complication rates in females for diagnostic and interventional procedures combined are significantly lower using the TR versus the TF approach. Age-related impact on complications • Elderly populations who are post cardiac intervention have increased in-hospital mortality and morbidity related to vascular complications and bleeding. • The etiology of increased vascular complications is related to alteration in vascular anatomy and calcification. • There is a significant decrease in vascular complications when utilizing the TR approach versus the TF approach. Reconciling the challenges in TR approach in women & the elderly • Despite a proven decrease in vascular complications in women and elderly undergoing TR versus TF catheterization, there is still unwillingness for many operators to adopt TR catheterization into their practices, likely due to concerns regarding excess procedural and fluoroscopy times. • Upper extremity complications associated with the TR approach including perforations, forearm hematomas, and compartment syndromes are not conditions commonly faced by the interventional cardiology community and this likely augments the disproportionate anxiety level in operators. Conclusion • The benefits of TR over TF catheterization in female and elderly patient populations continue to outweigh the AAC in either group. • With increased emphasis on improved patient-centered outcomes, a TR option should be integrated into every institution’s cardiac catheterization program.
Keywords
complications, elderly, transfemoral, transradial, women
Background
Since its introduction in 1989, the transradial (TR) approach to cardiac catheterization and coronary angioplasty has been shown to offer several advantages over the transfemoral (TF) approach [1]. For example, the TR approach is associated with a decreased risk of vascular access complications and shorter hospitalizations [2–6]. However, the utilization of the TR approach has many perceived limitations, requiring adequate training to avoid access site crossover, prolonged procedure time, and increased radiation exposure [6,7]. While the economic incentive of shorter hospitalizations and overall decreased vascular complications remain alluring, the demographics of the typical patient with coronary artery disease have changed. Currently, this patient population has a higher percentage of women and elderly individuals, both who have been linked to higher rates of complications [2,8,9].
Women account for approximately 46% of the 635,000 Americans with acute coronary syndrome [9]. The outcomes of this patient population has suggested gender as a strong independent factor of vascular complications [10,11]. Efforts to minimize these complications are paramount in the care of women with coronary artery disease, favoring a transition from TF to TR catheterization.
In addition to gender, age has been identified as a significant risk factor for bleeding complications [2,10–13]. Specifically, the subgroup of patients greater than 70 years old is at an increased risk for access site hematoma, gastrointestinal bleeding, and a higher mortality at 3-year follow-up [14]. The TR approach in patients 75 years and older has been shown to have a high success rate and lower major and minor complication rates [11]. Despite the decreased risk with the TR technique, the associated catheterizationrelated complications have led to a less invasive management overall in elderly patients. While the TR technique has fallacies of its own, these high-risk subgroups will benefit from increased utilization of this approach for cardiac catheterization.
This article aims first to detail the known complications of the TR and TF techniques in the general population, then focus on the notably susceptible groups of female and elderly patients. By characterizing the previous challenges faced in these groups, the article will postulate future innovations and techniques to decrease the mortality and morbidity for these vulnerable subgroups.
TR versus TF approach
complications
The transition from the classic TF approach toward a TR approach for cardiac catheterization was heralded by studies noting a dramatic reduction of access-associated complications (AAC) using the latter method [12,13]. The ‘downstream’ benefits of lower AAC include decreased medical costs, hospitalization fees, and length of stay. In a large randomized clinical trial, the authors demonstrated a reduction in vascular complications, but were unable to show a reduction in 30-day morbidity (i.e., myocardial infarction, major bleeding, and stroke) and mortality between TF and TR [2]. The RIVAL trial demonstrated that isolating centers with greater experience with TR technique was associated with a decline in 30-day morbidity and mortality. Despite improvement in vascular access closure devices and use of safer anticoagulants that decreased AAC for both TF and TR approaches, the relative risk for AAC remains higher in both female patients, as well as elderly patients (defined as greater than 75 years old) despite method of entry [12,13].
Complications in females
Although many trials have documented the impact of gender on outcomes, the physiologic basis of this disparity is not clear [3,13,15]. A review of over 13,000 cases in the ACC-NCDR registry explored specific vascular and bleeding complications, as well as potential contributing biologic factors (i.e., smaller femoral artery vasculature that may benefit from smaller sheath sizes) [16]. A statistically significant increased risk for vascular complications was observed in women more so than men, specifically with entry site bleeding, hematoma, and pseudoaneurysm while retroperitoneal bleed and dissection were not statistically significant [13,16]. The authors adjusted the vascular complications for sheath size as increasing sheath size is directly proportional to increased AAC [13,16]. Interestingly, the relative risk for access complications in women versus men is also augmented with a larger sheath, suggesting that either femoral artery vasculature is smaller or more susceptible to injury among women [16].
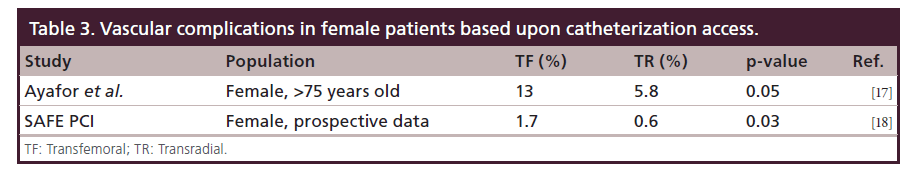
Despite the decrease in overall number of access complications with smaller sheath sizes for TF approach, the discrepancy in complications between female and male patients remains [15]. In a single-center study, the relative risk of vascular and bleeding complications between women and men in the TF group was eliminated in the TR group. This data would suggest that TR would be the preferred method for female patients, confirmed again by another single-center study that noted similar findings specifically in women over the age of 75 years [17].
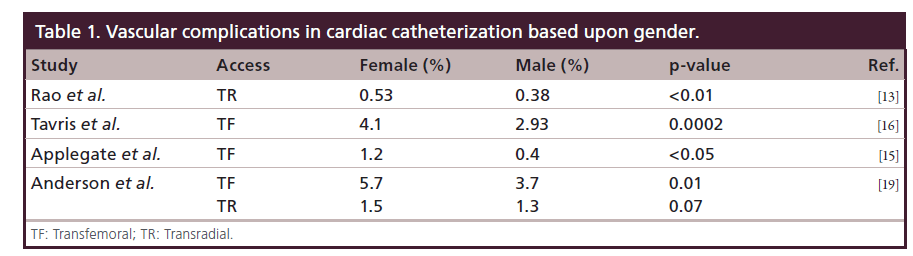
A recently presented multicenter, randomized, prospective clinical trial studying urgent or elective percutaneous coronary intervention (PCI) in women, hypothesizes that TR PCI will result in a significant reduction in bleeding and vascular complications compared with TF PCI [18]. The initial data indicates that bleeding and complication rates (for diagnostic and interventional procedures combined) were significantly lower in the TR than TF approach. However, there was no difference in the primary, composite end point [18]. The reduction in vascular complications is mirrored by the multicenter randomized study of RIFLE-STEACS [3]. The study once again noted female gender as an independent risk factor for net composite of cardiac death, stroke, myocardial infarction, and bleeding [3]. Despite this risk, TR approach led to improved 30-day cardiac morbidity and mortality across both gender and age (Table 1) [3].
Age-related impact on complications
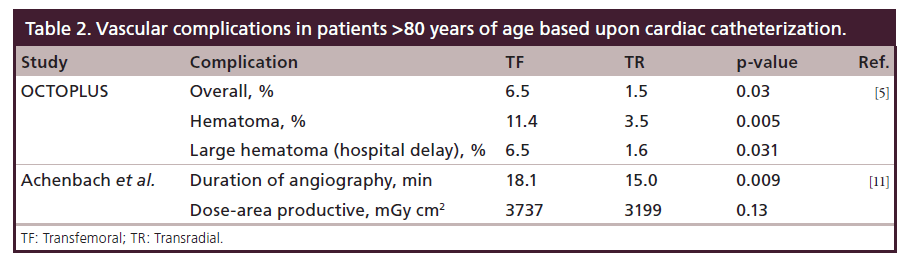
With the growing proportion of elderly population and the increased risks and complications of cardiovascular disease as one ages, access site complications for the aging population has also been evaluated [5,11]. The overall increase in-hospital mortality and morbidity in the aging population post cardiac intervention is matched with a statistically significant increase in vascular complications and bleeding risks in this population [20]. The etiology of increased vascular complications has been attributed to alteration in vascular anatomy with arterial loops and calcification of vasculature [5,11,20]. Although both of these contributing factors should affect both TF and TR approaches, the OCTOPLUS study evaluating 377 patients over the age of 80 years noted a significant decrease in vascular complications when utilizing TR approach versus TF approach [5]. Both hematoma and large hematoma (defined as a hematoma that resulted in a delay in discharge from hospital) noted a marked decline in the TR group [5].
Regardless of the origin of access, the elderly population has proven to be a consistently vulnerable group not only in the more immediate vascular complications but also in major adverse cardiac events weeks to months postprocedure. Three separate retrospective analyses confirm that the elderly populations are more vulnerable to AAC risks and long-term mortality risks along with the procedural complexity their anatomy creates. Despite advancement in vascular closure techniques, trends in PCI techniques, or access strategies, age remains an independent, negative risk factor for periprocedural complications, as well as long-term mortality (Tables 2 & 3) [21–23].
Reconciling the challenges in TR approach in women & the elderly
Although multiple previous studies have proven a decrease in vascular complications, TR catheterization has yet to become an integral part of many hospital’s cardiac catheterization programs. Experts cite multiple reasons to explain the lack of more widespread penetration of TR approach in the field. Many operators are often unwilling to adopt new techniques, have concerns for excess procedural and fluoroscopy times, as well as for upper extremity complications that are specific to TR approach [13,24].
Access site bleeding complications associated with the TR approach include perforations, forearm hematomas and rarely compartment syndromes [13]. These are not conditions commonly faced by the interventional cardiology community; thus, resulting in a disproportionate level of anxiety. Interestingly, female gender is an independent risk factor for forearm hematoma [13,25].
Forearm hematomas originating from a radial artery perforation is also more prominent when accessing more tortuous radial arteries as observed in elderly patients and shorter female patients [26]. In the EASY trial, the statistically significant increase in forearm hematoma in women must be balanced by evaluating the clinical significance of these forearm hematomas. More than half of the hematomas in female patients documented were ≤5 cm explaining no significant increase in major bleeding requiring any transfusion between gender subgroups [25]. Even with the use of larger 6 Fr catheters in a single-center study, the increase of access site bleeding risks in women is only minor [27]. Clinically significant bleeding is rare with TR approach due to mechanical closure methods, prompt intervention with pressure dressings and close monitoring of access sites.
In addition to bleeding, other important complications related to TR approach include asymptomatic occlusion, dissection, and spasm. Radial arterial occlusion is thought to be a thrombotic process triggered by endothelial injury during sheath insertion. Key risk factors for arterial occlusion are larger sheath size, prolonged postprocedure compression, and lack of anticoagulation. While neither asymptomatic occlusion nor radial arterial occlusion with ischemia have a predilection toward either female or elderly subgroups [28], the higher rate of past PCI attempts seen in the elderly population correlates with increased nonocclusive radial artery injury [5,22]. Ensuring the sheath to artery ratio <1 may result in decreased arterial occlusion in these subgroups with smaller arterial diameters. Unlike occlusion, radial arterial spasm can be seen with more tortuous and smaller diameter vessels, both of which are seen more commonly in women and the elderly. Fortunately, the increased constriction from the injured vessels may normalize at 12 months after access [24].
These issues partially account for procedural failure, access site crossover to TF, and increased radiation exposure with prolonged procedure times [14]. Radial arterial spasm can be seen with more tortuous and smaller diameter vessels, both of which are seen more commonly in women and the elderly. Fortunately, the increased constriction from the injured vessels may normalize at 12 months after access. These issues partially account for procedural failure, access site crossover to TF, and increased radiation exposure with prolonged procedure times.
The overall discrepancy in length of procedure time and of fluoroscopy exposure time between radial and femoral access in the elderly remains unclear. While Caputo et al. did not observe a notable discrepancy between total procedure time or fluoroscopy time, one must understand that individual physicians were able to choose access site for patients >70 years old. The decision could be for a variety of reasons including physician competency in TR approach or poor experience with known tortuous or calcified radial vessels in elderly patients [11]. A contributing factor to prolonged procedure time is radial access failure, requiring access site crossover [29]. Through a large analysis from a single-center study, prime reasons for access site failure include failure to advance catheter to ascending aorta, failure of radial arterial access, and lack of guide support [29]. Female sex and advanced age yet again remain an independent risk factor for access site failure [29,30]. Specifically in elderly patients, the tortuosity of subclavian tortuosity can be counteracted by the use of left radial approach, decreasing procedure time [30]. The difficulty in traversing a tortuous pathway through subclavian innominate and aorta can be counteracted by the more direct curvilinear route through the left subclavian (similar to a TF approach) [30]. However, the study that touted this benefit could not eliminate the confounding factor of using a preshaped TF catheter from the success of the left radial approach by itself [30]. Both puncture time and duration of angiography were significantly increased in TR approach in elderly patients. However, the total fluoroscopy time and measurement of exposure via dose-area product remain not significant [11].
Conclusion
Despite a decline in overall vascular complications with the transition from TF to TR cardiac catheterizations, both female and elderly patients still pose increased rate of adverse outcomes. The combination of an aging patient population and the heightened awareness of atypical cardiac symptoms in females results in a group of elderly women who are assumed to be more susceptible to vascular damage than either subgroup alone. However, the benefits of TR over TF catheterization continue to outweigh the AAC in either group. By focusing efforts on the vulnerable yet expanding population of elderly and female patients, the encompassing field of cardiology will again adapt to the evolving face of coronary artery disease. In this era of increased emphasis on improved patient-centered outcomes, a TR option should become an integral part of every institution’s cardiac catheterization program.
Future perspective
Given the known benefits of TR over TF catheterization, which continue to outweigh the AAC in elderly and female patients, it can be speculated that more institutions will integrate a TR option into their catheterization programs. The transition from the classic TF toward TR catheterization will decrease the observed morbidity and mortality related to vascular complications in vulnerable subgroups.
Executive summary
Transradial versus transfemoral approach: complications
• The transition from the classic transfemoral (TF) approach to a transradial (TR) approach is notable for a dramatic reduction of access-associated complications (AAC) including decreased medical costs, hospitalization fees and length of stay.
• Despite the improvement in vascular access closure devices and the use of safer anticoagulants, the relative risk for AAC remains higher in both female patients and elderly patients regardless of method of entry.
Complications in females
• There is a significantly increased risk for vascular complications in females using the TF approach.
• Specific complications include entry site bleeding, hematoma, and pseudoaneurysm formation.
• The relative risk for access complications in females is augmented with larger sheath sizes.
• Bleeding and complication rates in females for diagnostic and interventional procedures combined are significantly lower using the TR versus the TF approach.
Age-related impact on complications
• Elderly populations who are post cardiac intervention have increased in-hospital mortality and morbidity related to vascular complications and bleeding.
• The etiology of increased vascular complications is related to alteration in vascular anatomy and calcification.
• There is a significant decrease in vascular complications when utilizing the TR approach versus the TF approach.
Reconciling the challenges in TR approach in women & the elderly
• Despite a proven decrease in vascular complications in women and elderly undergoing TR versus TF catheterization, there is still unwillingness for many operators to adopt TR catheterization into their practices, likely due to concerns regarding excess procedural and fluoroscopy times.
• Upper extremity complications associated with the TR approach including perforations, forearm hematomas, and compartment syndromes are not conditions commonly faced by the interventional cardiology community and this likely augments the disproportionate anxiety level in operators.
Conclusion
• The benefits of TR over TF catheterization in female and elderly patient populations continue to outweigh the AAC in either group.
• With increased emphasis on improved patient-centered outcomes, a TR option should be integrated into every institution’s cardiac catheterization program.
Financial & competing interests disclosure
A Shroff serves as a consultant to Terumo Corporation who is a maker of radial products. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
Papers of special note have been highlighted as:
• of interest; •• of considerable interest
- Kiemeneij F, Laarman, GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet. Cardiovasc. Diagn. 30, 173–178 (1993).
- Jolly SS, Yusuf S, Cairns J et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet 377(9775), 1409–1420 (2011).
- Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al. Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in STElevation Acute Coronary Syndrome) study. J. Am. Coll. Cardiol. 60(24), 2481–2489 (2012).
- Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am. Heart J. 157(1), 132–140 (2009).
- Louvard Y, Benamer H, Garot P et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am. J. Cardiol. 94(9), 1177–1180 (2004).
- Sciahbasi A, Burzotta F, Rigattieri S et al. Impact of vascular approach (transradial vs transfemoral) on the efficacy of thrombus aspiration in acute myocardial infarction patients. Cardiovasc. Revasc. Med. 13(2), 79–83 (2012).
- Jolly SS, Cairns J, Niemela K et al. Effect of radial versus femoral access on radiation dose and the importance of procedural volume: a substudy of the multicenter randomized RIVAL trial. JACC Cardiovasc. Interv. 6(3), 258–266 (2013).
- Safley DM, Amin AP, House JA et al. Comparison of costs between transradial and transfemoral percutaneous coronary intervention: a cohort analysis from the Premier research database. Am. Heart J. 165(3), 303–309.e302 (2013).
- Go AS, Mozaffarian D, Roger VL et al. Heart disease and stroke statistics – 2013 update: a report from the American Heart Association. Circulation 127(1), e6–e245 (2013).
- Akhter N, Milford-Beland S, Roe MT, Piana RN, Kao J, Shroff A. Gender differences among patients with acute coronary syndromes undergoing percutaneous coronary intervention in the American College of Cardiology- National Cardiovascular Data Registry (ACC-NCDR). Am. Heart J. 157(1), 141–148 (2009).
- Achenbach S, Ropers D, Kallert L et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter. Cardiovasc. Interv. 72(5), 629–635 (2008).
- Brueck M, Bandorski D, Kramer W, Wieczorek M, Holtgen R, Tillmanns, . A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc. Interv.2(11), 1047–1054 (2009).
- Rao SV, Ou FS, Wang TY et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. JACC Cardiovasc. Interv.1(4), 379–386 (2008).
- Bagur R, Bertrand OF, Rodes-Cabau J et al. Comparison of outcomes in patients > or =70 years versus <70 years after transradial coronary stenting with maximal antiplatelet therapy for acute coronary syndrome. Am. J. Cardiol. 104(5), 624–629 (2009).
- Applegate RJ, Sacrinty MT, Kutcher MA et al. Vascular complications in women after catheterization and percutaneous coronary intervention 1998–2005. J. Invasive Cardiol. 19(9), 369–374 (2007).
- Tavris Dr WY, Jacobs S et al. Bleeding and vascular complications at the femoral access site following percutaneous coronary intervention (PCI): an evaluation of hemostasis strategies. J. Inv. Cardiol. 24(7), 328–334 (2012).
- Ayafor G A-RM, Gulati M, Capers Q. PCI in elderly women: superior outcomes with transradial versus transfemoral approach. J. Am. Coll. Cardiol. 61(Suppl. 10), doi:10.1016/ S0735-1097(13)61595-8 (2013).
- Rao Sv HC, Barham B et al. A registry-based randomized trial comparing radial and femoral approaches in women undergoing percutaneous coronary intervention: the study of access site for enhancement of PCI for women (SAFEPCI for Women) trial. JACC Cardiovasc. Interv. 7(8), 857–867 2014).
- Anderson J, Sacrinty M, Turner S et al. Gender differences in vascular complications associated with transfemoral and transradial cardiac catheterization and PCI: a single-center experience. J. Am. Coll. Cardiol. 61(Suppl. 10), doi:10.1016/ S0735-1097(13)60078-9 (2013).
- Singh M, Peterson ED, Roe MT et al. Trends in the association between age and in-hospital mortality after percutaneous coronary intervention: National Cardiovascular Data Registry experience. Circulation Cardiovasc. Int. 2(1), 20–26 (2009).
- Dodson JA, Wang Y, Chaudhry SI, Curtis JP. Bleedingavoidance strategies and outcomes in patients >/=80 years of age with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention (from the NCDR CathPCI Registry). Am. J. Cardiol. 110(1), 1–6 (2012).
- Rao SV, Hess CN, Dai D, Green CL, Peterson ED, Douglas PS. Temporal trends in percutaneous coronary intervention outcomes among older patients in the United States. Am. Heart J. 166(2), 273–281.e274 (2013).
- Rodriguez-Leor O, Fernandez-Nofrerias E, Carrillo X et al. Results of primary percutaneous coronary intervention in patients >/=75 years treated by the transradial approach. Am. J. Cardiol. 113(3), 452–456 (2013).
- Kanei Y, Kwan T, Nakra NC et al. Transradial cardiac catheterization: a review of access site complications. Catheter. Cardiovasc. Interv. 78(6), 840–846 (2011).
- Tizon-Marcos H, Bertrand OF, Rodes-Cabau J et al. Impact of female gender and transradial coronary stenting with maximal antiplatelet therapy on bleeding and ischemic outcomes. Am. Heart J. 157(4), 740–745 (2009).
- Calvino-Santos RA, Vazquez-Rodriguez JM, Salgado- Fernandez J et al. Management of iatrogenic radial artery perforation. Catheter. Cardiovasc. Interv. 61(1), 74–78 (2004).
- Pristipino C, Pelliccia F, Granatelli A et al. Comparison of access-related bleeding complications in women versus men undergoing percutaneous coronary catheterization using the radial versus femoral artery. Am. J. Cardiol. 99(9), 1216–1221 (2007).
- Kotowycz MA, Dzavik V. Radial artery patency after transradial catheterization. Circulation Cardiovasc. Int. 5(1), 127–133 (2012).
- Dehghani P, Mohammad A, Bajaj R et al. Mechanism and predictors of failed transradial approach for percutaneous coronary interventions. JACC Cardiovasc. Int. 2(11), 1057–1064 (2009).
- Sciahbasi A, Romagnoli E, Burzotta F et al. Transradial approach (left vs right) and procedural times during percutaneous coronary procedures: TALENT study. Am. Heart J. 161(1), 172–179 (2011).
•• The RIVAL trial was a landmark large multicentered, randomized trial that clearly explain multiple benefits and even the limitations of the transradial (TR) over the transfemoral (TF) approach.
• The OCTOPLUS study was a large multicentered prospective evaluation of the benefits of TR over TF specifically in the aging population >80 years of age.
•• Large retrospective multicentered analysis of the National Cardiovascular Data Registry detailing the independent risk factors of female gender and age >75 years of increased bleeding and vascular complications despite TR approach.
•• The SAFE-PCI trial was one of the first randomized trials determining the benefits and limitations of TR versus TF approach in women.
• Kanei’s evaluation of specific difficulties with TR technique help to delineate possible solutions to further enhance the benefits of TR approach.
• TALENT study noted potential benefits from left-sided radial approach, thus assisting in decreasing complications in a key subgroup of elderly patients.