Research Article - Diabetes Management (2018) Volume 8, Issue 1
Trends of preventive healthcare utilizations in the type 2 diabetes in asian americans versus whites using behavioral risk factors surveillance system 2002-2013 data
- *Corresponding Author:
- Fengxia yan
Morehouse School of Medicine Atlanta
GA, United States
E-mail: fyan@msm.edu
Abstract
Objective: To examine the diabetes self-management and management with healthcare providers trends in Asian Americans compared to Non-Hispanic white.
Research Method: National telephone survey data BRFSS was used to analyze the trend. Total 372532 participants were used for our final analyses which included 6640 Asians and 365892 whites. SAS survey procedures were constructed to show the difference between Asian and whites.
Results: An increase trend of type 2 diabetes over 12 years was observed in both Asian and white. There was no significant difference of diabetes rate between Asian and white from the raw data while Asian was almost 50% more likely to have type2 diabetes after adjusting age, gender and BMI. There were increase trend in self-checking blood sugar and feet as well as HbA1C checking at least twice a year and checking feet with doctor at least a year. Asian was 50- 60% less likely to perform self-checking management including blood sugar and feet check. There were no significant difference of routine checkup, eye and feet checkup with doctors within past year as well as checking HbA1C at least twice a year.
Conclusion: Increase trend was observed in some diabetes management even though several management rates were very low in both Asian and white. Asian Americans were less likely to perform self-checking.
Keywords
preventive health care, type2 diabetes, Asian
Introduction
The National Diabetes Statistics Report data released on June 2014 showed that the diabetes prevalence in Asian American is 1.4 percent high than Non-Hispanic White [1,2]. Research using National Health Interview Survey (NHIS) data also showed Asian Americans have higher prevalence of type 2 diabetes [3]. Effective diabetes self- management, including self-care, keeping diabetes care appointments and getting vaccinated against influenza and pneumonia, is very important in reducing diabetes related morbidity and mortality. There is evidence that by lifestyle modification, medication and self-monitoring of blood glucose, diabetes can be better controlled [4,5]. The main goal of diabetes management is glycemic control and a reduction in diabetes related complications, morbidity and mortality. Self-management can benefit glycemic control as well as the diabetes management. Researchers have showed that diabetes self-management has great differences between racial and ethnic groups because of the socioeconomic status, disease knowledge and awareness, as well as access to healthcare which may influence the racial disparities of the diabetes outcomes [6-12]. Even though, no significant differences among whites, African Americans and Hispanic in HbA1c testing or examining feet for sores have been detected using 2000 Medical Expenditure Panel Survey (MEPS) data [13]. Recent study [14] using 2009 BRFSS data showed that compared to Whites, the Asian Americans were significantly less likely to check their blood sugar at least once a day. There are no differences between these two groups for diabetes education, having seen professionals for diabetes within past year, having cholesterol or HbA1C checked in past year, and having an eye or foot exam in past year. Several trend analyses conducted using national data showed an increase rate of diabetes prevalence over past decade [3,14]. Also there was study revealed increased rate of preventive healthcare for diabetes both in Non-Hispanic white and Africa American4. The American Diabetes Association recommends annual measurements of HbA1c, lipids, cholesterol and urine protein; dilated eye and foot examinations; and biannual measurement of blood pressure [15]. These recommendations have been associated with the decreases of diabetes complications rate [16-20]. The diabetes preventive health care are less in minority including Asian Americans [4], racial disparities in preventive health care may contribute to the higher rate of diabetes-related complications and mortality. To examine the preventive diabetes self-management changes over time as well as the racial differences can provide better intervention program to better control the diabetes. However, there is little information about the preventive health care trend over time period in Asian American population.
Research Design and Method
▪ Data source
Behavioral Risk Factor Surveillance System (BRFSS) from Center for Disease Control and Prevention’s (CDC) is a state-based system used to gather information through random digit dialing conducted by the health departments of all 50 states, the District of Columbia, Guam, Puerto Rico, and the U.S. Virgin Islands, with help from Centers for Disease Control and Prevention (CDC). This survey collected preventive health practices and chronic disease data from individuals aged 18 and older [21]. All the data are from self-reported responses.
▪ Study population
The subgroup of non-Hispanic whites and Asian Americans who were surveyed between 2002 and 2013 will be included in this study. Data files were downloaded from the CDC website in SAS Transport format. The variables which missing values exceeded 20% were excluded from the study measures. Because same variable may have different measurement in different year, the related variables in each were checked to make sure they are combinable. Total 372532 participants were used for our final analyses which included 6640 Asians and 365892 whites.
▪ Race and ethnicity
Race and ethnicity status were based on selfreport data. Ethnicity was coded as Hispanic or non-Hispanic. Non-Hispanic participants were assigned one of the following racial categories: White, African American/Black, Asian, Native Hawaiian/Pacific Islander, American Indian/ Native Alaskan (Native American), other, or mixed race. We included non-Hispanic white and Asian in our study. Other socioeconomic status variable including age, gender, education, income, access to health care and US born also will be adjusted. If more than 5% missing values are observed for any socioeconomic status variable, the unknown level will be added for that variable.
▪ Diabetes status and typology
Diabetes status was determined using responses to the question, “Have you ever been told by a doctor that you have diabetes”. BRFSS participants were considered to have diabetes if they reported having been told by a doctor that they had the disease. Women who reported diabetes only when pregnant and respondents told they had pre-diabetes or borderline diabetes will be treated as non-diabetic individuals. Study participants were considered to have type 2 diabetes if their age at diagnosis was 30 years or older or if their age at diagnosis was less than 30 years and they did not use insulin [22,23].
▪ Preventive healthcare
The frequency for each individual outcome will be presented first. Furthermore, the preventive health care variables will be reclassified as two groups: 1) Personally manage their diabetes: if they reported checking their blood sugar levels at least once a day and if they checked their feet for sores or irritations at least once a day, they will be treated as personally manage their diabetes well. Otherwise, they will be treated as no personally manage their diabetes. 2) Mange diabetes via healthcare provider: if they visited a healthcare professional for diabetes within past year, had their hemoglobin A1c checked at least twice a year, and had their feet checked for sores or irritations by doctor at least once a year, and checked eye by doctor within past year, they will be treated as mange diabetes well via healthcare provider. Otherwise, they will be treated as no manage diabetes via healthcare provider.
▪ Statistical analysis
The 12 years data were merged and created new design variables that consider primary sampling unit, stratum and sampling weight in order to accommodate different sampling designs between 2002-2010 and 2011-2013. In order to increase the robustness of the analysis and decrease the standard error in Asian group, the data were pooled in to four three-year period subgroups. Demographic characteristics between Asian and whites were summarized using weighted percentages and standard errors for these percentages. Rao-Scott Chi-Square Test [24-26] a design adjusted Pearson Chi-Square test which considered complex survey design was performed to compare the racial difference of demographic characteristics as well as the preventive healthcare utilization. The raw diabetes prevalence within these two races in 12 years was reported using bar graph and smoothed curve. Odds ratio plot was displayed to show the differences between Asian and white after adjusting age, gender and BMI. In order to adjust possible covariate for the difference of preventive healthcare use between Asians and white, logistics regression for complex survey design was constructed and adjusted odds ratios were reported for the pooled subgroups. Non-parametric trend test across years were used to examine the preventive health care change trends. All data management and analyses were performed using the SAS system (version 9.4; SAS institute; Cary, NC) and its complex survey-specific procedures to consider the complex survey design. P-value less than 0.05 will be considered as statistically significant. No multiple comparisons were considered in this study.
Results
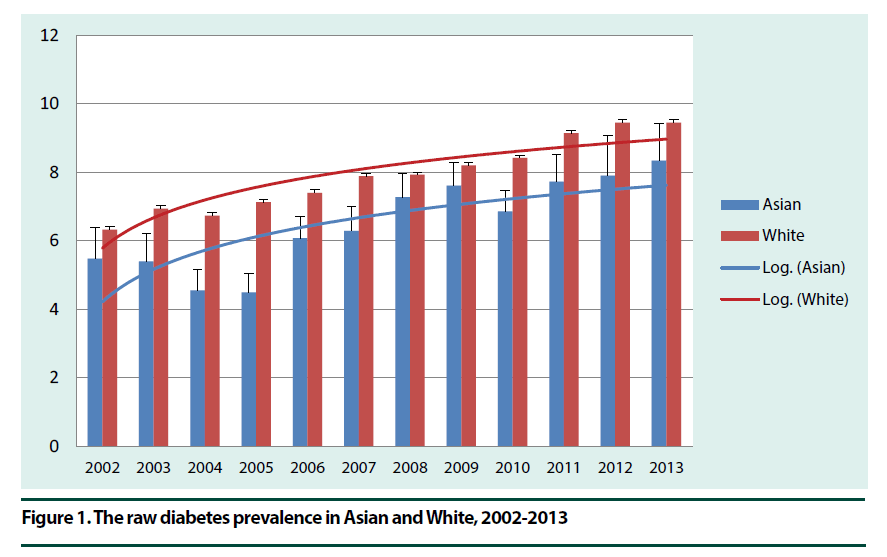
Demographic characteristics of type 2 diabetes individual of both 6640 Asians and 365892 whites were displayed in Table 1. In the BRFSS data over 12 years, Whites had higher percentage of 65 or older person while Asian Americans had more male participants, higher education level and employed rate. Asian Americans also had more participants earned $50,000 or more and good health condition. As expected, Asian’s obese rate was lower than whites while there were a significant increase obese rate in both Asian and whites (Table 1). All demographic characteristics and obese status of Asian were significantly different from those of whites (p<0.05) except the income of Asian in 2005-2007 (p=0.1068). Figure 1 showed the raw diabetes prevalence in Asian over 12 year period was from 5.5% in year 2002 to 8.3% in year 2013 which was lower than prevalence in white (6.3%-9.5%). These differences were not statistically significant.
| 2002-2004 | 2005-2007 | 2008-2010 | 2011-2013 | |||||
|---|---|---|---|---|---|---|---|---|
| Asians | Whites | Asians | Whites | Asians | Whites | Asians | Whites | |
| Column % (SE) | Column % (SE) | Column % (SE) | Column % (SE) | |||||
| N | 743 | 45135 | 1358 | 81473 | 2095 | 109086 | 2444 | 130198 |
| Age≥65 (%) | 25.42 (4.41) | 45.30 (0.40) | 36.76 (3.17) | 44.74 (0.31) | 31.07 (1.86) | 44.27 (0.26) | 36.40 (2.35) | 46.06 (0.25) |
| Male (%) | 62.24 (4.84) | 50.95 (0.40) | 64.66 (2.99) | 51.58 (0.32) | 65.03 (1.93) | 52.08 (0.27) | 57.04 (2.41) | 51.26 (0.26) |
| Education (Some college or graduate) (%) | 82.15 (4.12) | 49.67 (0.40) | 77.75 (2.58) | 52.09 (0.32) | 77.37 (1.75) | 54.27 (0.26) | 71.78 (2.41) | 49.26 (0.26) |
| Income (50,000 or more) (%) | 48.08 (4.99) | 27.84 (0.41) | 40.70 (3.28) | 34.39 (0.35) | 49.53 (2.28) | 37.01 (0.29) | 49.32 (2.55) | 34.52 (0.28) |
| Employed (%) | 58.94 (5.13) | 41.35 (0.40) | 58.89 (3.15) | 41.31 (0.32) | 55.91 (2.12) | 40.51 (0.27) | 55.87 (2.44) | 37.07 (0.26) |
| Health condition good (%) | 67.25 (4.85) | 54.53 (0.40) | 62.85 (3.19) | 56.17 (0.32) | 68.91 (1.97) | 58.49 (0.26) | 63.10 (2.40) | 57.40 (0.26) |
| Obese (%) | 10.73 (2.43) | 48.61 (0.41) | 18.65 (2.42) | 51.31 (0.33) | 20.24 (1.75) | 53.23 (0.27) | 22.16 (2.02) | 54.11 (0.27) |
Table 1. Demographic Characteristics of type 2 diabetes Asian and whites, BRFSS 2002-2013.
Figure 1. The raw diabetes prevalence in Asian and White, 2002-2013.
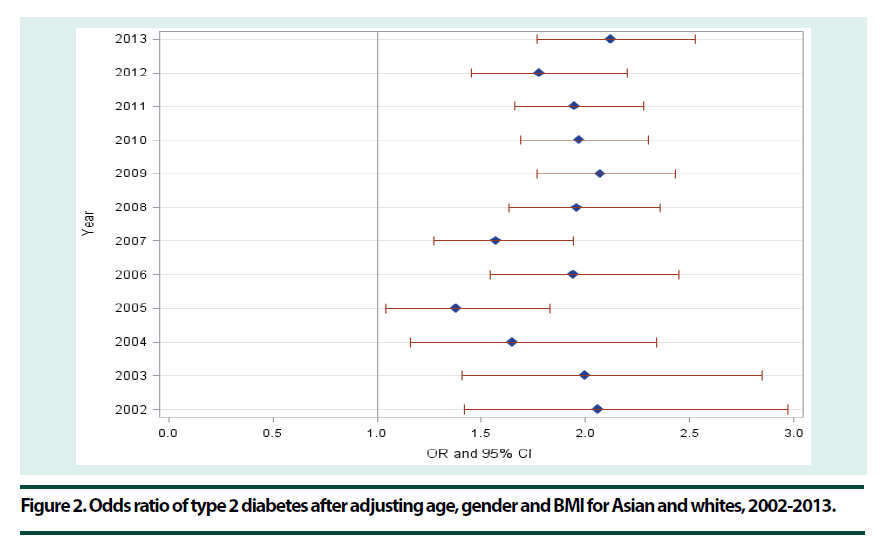
Figure 2 showed the age, sex and BMI adjusted type 2 diabetes prevalence odds ratio between Asian and whites. The prevalence in Asian was 50-60% higher than whites in year 2002-2004, 2008-2013 and this prevalence was 30% higher in year 2005-2007. Our results also showed that the type 2 diabetes rates had increase trend in both Asian and whites.
Figure 2. Odds ratio of type 2 diabetes after adjusting age, gender and BMI for Asian and whites, 2002-2013.
Personal diabetes management in Asian and whites over 12 years was listed in Table 2. Half of Asians and almost 40% of whites didn’t self-check their blood sugar or feet at least once a day. Even though the rate for both self-checking blood sugar and feet was only lower than 30% in Asian and lower than 50% in whites, there was an increase trend observed in sugar selfchecking and feet self-checking (P<0.001) while there were no trend changes after combining two self-checking (p=0.0711). Over 12 years period, compare to their white counterparts, Asians were almost half less likely to self-check blood sugar at least once day and were almost 60% less likely to self-check their feet for sore or irritations and these differences were statistically significant. Even after adjusting demographic characteristics and BMI, there were still significant differences of self-checking blood sugar and feet at least once a day between Asian and white.
| Year | Asian | White | Raw Odds ratio (95% CI) | Adjusted Odds ratio (95% CI) | |
|---|---|---|---|---|---|
| Self-checking blood sugar at least once a day | |||||
| 2002-2004 | 35.79 (4.96) | 58.12 (0.45) | 0.40 (0.26-0.61) | 0.50 (0.32-0.79) | |
| 2005-2007 | 51.05 (3.92) | 62.91 (0.37) | 0.61 (0.45-0.84) | 0.67 (0.47-0.93) | |
| 2008-2010 | 47.55 (3.44) | 61.78 (0.33) | 0.56 (0.43-0.74) | 0.72 (0.53-0.97) | |
| 2011-2013 | 46.80 (2.78) | 61.25 (0.36) | 0.56 (0.45-0.69) | 0.64 (0.50-0.82) | |
| Self-checking feet for sores or irritations at least once a day | |||||
| 2002-2004 | 45.29 (5.58) | 67.93 (0.44) | 0.39 (0.25-0.61) | 0.40 (0.26-0.61) | |
| 2005-2007 | 48.03 (3.99) | 68.14 (0.37) | 0.43 (0.32-0.59) | 0.46 (0.32-0.64) | |
| 2008-2010 | 46.88 (3.50) | 65.23 (0.33) | 0.47 (0.36-0.62) | 0.60 (0.45-0.82) | |
| 2011-2013 | 40.79 (2.77) | 63.57 (0.35) | 0.39 (0.31-0.50) | 0.42 (0.33-0.54) | |
| Personally management | |||||
| 2002-2004 | 17.47 (3.29) | 41.75 (0.44) | 0.30 (0.19-0.46) | 0.35 (0.21-0.58) | |
| 2005-2007 | 25.20 (3.60) | 44.85 (0.38) | 0.41 (0.28-0.60) | 0.45 (0.30-0.68) | |
| 2008-2010 | 28.89 (3.16) | 42.58 (0.32) | 0.55 (0.40-0.74) | 0.84 (0.60-1.17) | |
| 2011-2013 | 20.71 (2.11) | 41.02 (0.35) | 0.38 (0.29-0.48) | 0.44 (0.33-0.58) |
Personal management was defined as check sugar at least once a day and check feet at least once a day.
Table 2. Personal diabetes management in Asian American and whites, 2002-2013.
Table 3 showed the diabetes management using healthcare providers. The routine checkup with doctors in 2002-2004 periods had higher standard error than other period in both Asian and white because there were no measurements of routine checkup in year 2003 and 2004. For year period 2005-2013, there was no significant trend changes of routine checkup (p=0.4176). There was an increase trend of checking feet for sore with doctors (p<0.001) and HbA1C checking at least twice a year (p<0.001) while there was no increase trend of eye checking (p=0.0871). Compared to white, there was no significant difference of routine checkup, feet and eye check with doctors. The percentage of checking HbA1C at least twice a year was from 81%-90% over 12 years in Asian and this percentage in whites was around 90%. There was no significant difference of checking A1C at least twice a year over 12 years period. The rate of performing four diabetes management with healthcare provider was only around 20% in Asian and 30% in whites. There was significantly difference between Asian and white for year 2002-2004 (odds ratio=0.61(0.41-0.92)), 2008- 2010 (odds ratio=0.46(0.37-0.57)) and 2011- 2013 (odds ratio=0.48(0.40-0.59)). Even after adjusting demographic factors and BMI levels, there was still significant difference for year 2008-2010 (odds ratio=0.47(0.37-0.60)) and 2011-2013 (odds ratio=0.52(0.41-0.64)).
| Year | Asian | White | Raw Odds ratio (95% CI) | Adjusted Odds ratio (95% CI) | |
|---|---|---|---|---|---|
| Routine checkup within past year | |||||
| 2002-2004 | 93.30 (6.07) | 90.13 (1.36) | 1.53 (0.22-10.48) | 2.02 (0.23-18.13) | |
| 2005-2007 | 88.15 (2.00) | 87.03 (0.23) | 1.11 (0.76-1.62) | 1.21 (0.81-1.80) | |
| 2008-2010 | 86.05 (1.48) | 87.01 (0.19) | 0.92 (0.72-1.18) | 1.03 (0.78-1.35) | |
| 2011-2013 | 84.36 (1.67) | 87.04 (0.19) | 0.80 (0.62-1.03) | 0.87 (0.65-1.15) | |
| Checking feet for sores or irritations with doctor within past year | |||||
| 2002-2004 | 55.33 (5.58) | 68.07 (0.43) | 0.58 (0.37-0.91) | 0.56 (0.35-0.90) | |
| 2005-2007 | 62.38 (3.98) | 70.12 (0.35) | 0.71 (0.51-0.99) | 0.75 (0.52-1.08) | |
| 2008-2010 | 69.37 (3.43) | 71.76 (0.31) | 0.89 (0.65-1.22) | 0.94 (0.66-1.34) | |
| 2011-2013 | 68.95 (2.63) | 72.86 (0.33) | 0.83 (0.65-1.06) | 0.85 (0.65-1.12) | |
| Checking eye with doctor within past year | |||||
| 2002-2004 | 60.88 (5.92) | 69.83 (0.43) | 0.67 (0.41-1.10) | 0.72 (0.42-1.21) | |
| 2005-2007 | 74.93 (3.40) | 70.72 (0.35) | 1.24 (0.87-1.77) | 1.26 (0.83-1.90) | |
| 2008-2010 | 69.21 (3.38) | 69.66 (0.32) | 0.98 (0.72-1.34) | 0.91 (0.64-1.30) | |
| 2011-2013 | 73.97 (2.49) | 68.67 (0.34) | 1.30 (1.00-1.67) | 1.25 (0.95-1.64) | |
| Checking HbA1C at least twice a year | |||||
| 2002-2004 | 81.37 (6.43) | 89.32 (0.35) | 0.52 (0.23-1.20) | 0.83 (0.37-1.87) | |
| 2005-2007 | 90.26 (2.63) | 89.75 (0.25) | 1.06 (0.59-1.91) | 1.25 (0.70-2.25) | |
| 2008-2010 | 88.56 (2.51) | 91.14 (0.21) | 0.75 (0.46-1.23) | 1.04 (0.57-1.90) | |
| 2011-2013 | 90.42 (1.65) | 91.87 (0.23) | 0.84 (0.57-1.22) | 0.82 (0.53-1.26) | |
| Health care management | |||||
| 2002-2004 | 21.82 (3.49) | 31.23 (0.41) | 0.61 (0.41-0.92) | 0.65 (0.42-1.01) | |
| 2005-2007 | 31.89 (3.05) | 31.01 (0.30) | 1.04 (0.79-1.37) | 1.02 (0.76-1.39) | |
| 2008-2010 | 14.98 (1.40) | 27.73 (0.23) | 0.46 (0.37-0.57) | 0.47 (0.37-0.60) | |
| 2011-2013 | 9.43 (0.87) | 17.67 (0.17) | 0.48 (0.40-0.59) | 0.52 (0.41-0.64) |
Healthcare management included routine checkup, check feet or eye within past a year and checked HbA1C at least twice a year.
Table 3. Health management of diabetes using health care in Asian American and whites, 2002-2013.
Discussion
The type II diabetes disproportionally distributed among different race/ethnicities and minorities possessed higher rate of diabetes compared to white [27]. In this current study, the 12 years BRFSS data were utilized to compare the diabetes complications and diabetes preventive health care use. The results showed that the prevalence of diabetes in Asian was lower than prevalence in white before adjusting age, gender and BMI which is not consistent with the report from American Diabetes Association, where they reported that the Asian population had higher type II diabetes prevalence compare to their white counterparts [28]. This may because of the telephone survey sampling of Asian population. After adjusting age, gender and BMI level, the diabetes prevalence in Asian within 12 years was 50% - 110% higher than the diabetes prevalence in white and all odds ratios were statistically significant. So our data can well coincide with the previous study. Several studies explained the possible reasons of this difference [29-35] which built the foundation for our study. The reason included environmental risk as well as the race factors. Using same criterion of obesity for Asian population, the obesity rate in Asian is significantly lower than white while this difference became not statistically significant if different criterion were applied as mention by WHO expert consultation [36]. Adjusting for BMI means at the same BMI level, the diabetes prevalence in Asian was much higher than the prevalence in white. Proper preventive diabetes management can reduce the diabetes mortality and morbidity. Study using 2008-2012 BRFSS data showed us that there were racial disparity of health care services between Black and white among adults 65 years or older with diabetes [37]. Our results proved that Asian Americans were significantly less likely to check their blood sugar. These differences remained unchanged even after adjusting possible demographic risk factors. Blood sugar is the major factor to affect the process of diabetes. The reduced blood sugar check may lead to worse diabetes outcome, such as diabetes retinopathy. The good parts found from this study was both Asian and white had an increase trend of performing self-preventive health care over 12 year period. Our studies also showed that Asian population was more likely to check their eyes compare to their white counterparts. One possibility is that the people who suffered from diabetes retinopathy badly were more likely to check their eyes with doctors. Those who have more cardiovascular disease complications were more likely to get severe situation which makes them more to check blood sugar once a day, check HbA1C at least twice a year and more likely to perform routine checkup. Results from this study showed that both Asian and white had higher checkup rate with health care provider while the selfmanagement rates were lower. Half of the participants didn’t report self-management for blood sugar check as well as the eyes and feet check. Some researchers found out that Asian were the least race to get recommended diabetes screening which may contribute to the lower rate of blood sugar self-checking [38]. Our study suggested that preventive health care utilization to manage the type 2 diabetes is an important medical issue for both Asian and white. Further studies need to examine the effect of preventive health care on diabetes complications for both Asian and white. The strength of this study is that 12 years of national large survey data was used. Nevertheless, several limitations in this study need to be improved: first, all the variables included in this study such as the type 2 diabetes status are based on self-reported results and there is no way to verify by medical record review. Secondly, those individuals with severe physical disease, such as heart attack, stroke might not have been able to complete the survey. Although a previous research showed relatively high agreement of determining the diabetes status based on self-reports and those based on clinical diagnoses (kappa=0.76; sensitivity=75%), bias may occur due to the misclassification of diabetes and other variables status [39]. Another limitation came from the BRFSS data collection where exclude people without telephone and those with cell phone only before year 2011. The excluded people may be minority in majority and they may have higher cardiovascular disease which may lower the coverage of cardiovascular disease in Asian. The last limitation to this study may because of the questionnaire design where the language only has English version and Spanish version. Majority of Asian population especially older population can’t understand both languages which may reduce the Asian population with Diabetes. In the Kaiser study, Asian American who had difficulty to communicate in English had a lower frequency of home glucose monitoring [40] which related to poorer glucose control [41] then led to the occurrence of diabetes and its complications.
References
- Jessica S, Claudette E. "The Asian Population: 2000". Census 2000. United States Census Bureau. Retrieved October 20, 2014.
- Karen R, Nicholas A, Roberto R. "Overview of Race and Hispanic Origin: 2010". United States Census Bureau. United States Department of Commerce. Retrieved October 20, 2014.
- Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997-2008. Diabetes. Care. 34(2), 353–357 (2011).
- Hardman K, Hunt KJ, Cater RE et al. Diabetes management and vaccination rates in the southeast United States, 2000 through 2007. Ethn. Dis. 21(1),13–19 (2011).
- Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast Asian and African regions: need for effective strategies for prevention and control in primary health care settings. Int. J. Hypertens. Article ID 409083, P: 14 (2013).
- Oladele CRW, Barnett E. Racial/Ethnic and social class differences in preventive care practices among persons with diabetes. BMC. Public. Health. 6, 259–267 (2006).
- Harris M. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes. Care. 24 (3), 454–459 (2001).
- Chou AF, Brown AF, Jensen RE et al. Gender and racial disparities in the management of diabetes mellitus among Medicare patients. Womens. Health. Issues. 17 (3),150–161(2007).
- Nwasuraba C, Khan M, Egede LE. Racial/Ethnic differences in multiple self-care behaviors in adults with diabetes. J. Gen. Intern. Med. 22(1), 115–120 (2007).
- Egede L, Zheng D. Racial/Ethnic differences in adult vaccination among individuals with diabetes. Am. J. Public. Health. 93 (2), 324–329 (2003).
- Egede L, Zheng M. Racial/Ethnic differences in influenza vaccination coverage in high-risk adults. Am. J. Public Health. 2003; 93 (12):2074–2079.
- CDC Preventive-care practices among persons with diabetes--United States, 1995 and 2001. MMWR - Morbidity & Mortality Weekly Report. CDC. 51(43), 965–969 (2002).
- Lee JA, Liu CF, Sales AE. Racial and Ethnic Differences in Diabetes Care and Health Care Use and Costs. Prev. Chronic. Dis. 3(3), A85 (2006).
- Yan F, Guo JF, Cui X. Racial disparity of the preventive health care and behavior risk factors among Type 2 Diabetes. Ethn. Dis. 25(2), 220–225 (2015).
- Lin C, Li C, Hsiao C et al. Time trend analysis of the prevalence and incidence of diagnosed type 2 diabetes among adults in Taiwan from 2000 to 2007: a population-based study. BMC. Public. Health. 13,318–327 (2013).
- American Diabetes Association. Standards of medical care in diabetes. Diabete. Care. 27(1), S15–S35 (2004).
- Harris MI. Health care and health status and outcomes for patients with type 2 diabetes. Diabetes. Care. 23(6), 754–758 (2000).
- Huang ES, Gleason S, Gaudette R et al. Health care resource utilization associated with a diabetes center and a general medicine clinic. J. Gen. Intern. Med. 19(1), 28–35 (2004).
- Meigs JB, Stafford RS. Cardiovascular disease prevention practices by U.S. physicians for patients with diabetes. J. Gen. Intern. Med. 15(4),220–228 (2000).
- Saaddine JB, Engelgau MM, Beckles GL et al. A diabetes report card for the United States: quality of care in the 1990s. Ann. Intern. Med. 136(8), 565–574 (2002).
- Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, Georgia: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention.
- CDC. Behavioral Risk Factor Surveillance System. Available from: http://www.cdc.gov/brfss/index.htm Accessed 3/6/2017
- World Health Organization Study Group. Prevention of diabetes mellitus, report of a who study group. World. Health. Organ. Tech. Rep. Ser. 844, 1-100 (1994).
- Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness-of-fit and independence in two-way tables. J. Am. Stat. Assoc. 76(374), 221–230 (1981).
- Rao JNK, Scott AJ. On chi-squared tests for multi-way tables with cell proportions estimated from survey data. Ann. Stat.12(1), 46–60 (1984).
- Rao JNK, Scott AJ. On simple adjustments to chi-squared tests with survey data. Ann. Stat. 15(1), 385–397 (1987).
- Beckles G, Engelgau MM, Narayan KM. Population-based assessment of the level of care among adults with diabetes in the U.S. Diabetes. Care. 21(9), 1432–1438 (1998).
- Chan JC, Malik V, Jia W, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 301(20), 2129–2140 (2009).
- Malik V, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat. Rev. Endocrinol. 9(1), 13–27 (2013).
- Yajnik CS, Lubree HG, Rege SS et al. Adiposity and hyperinsulinemia in Indians are present at birth. J. Clin. Endocrinol. Metab. 87(12), 5575–5580 (2002).
- Huxley R, James WP, Barzi F et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. Obes. Rev. 9 (1), 53–61(2008).
- BMI Calculator. Asian American Diabetes Initiative Web site. http://aadi.joslin.org/content/bmi-calculator
- Hu Fb. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes. Care. 34(6), 1249–1257 (2011).
- Li Y, He Y, Qi L et al. Exposure to the Chinese famine in early life and the risk of hyperglycemia and type 2 diabetes in adulthood. Diabetes. 59(10), 2400–2406 (2010).
- Pearson JF, Bachireddy C, Shyamprasad S et al. Association between fine particulate matter and diabetes prevalence in the U.S. Diabetes. Care. 33(10), 2196–2201(2010).
- WHO expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 363(9403), 157-63 (2004).
- Chandler RF, Monnat SM. Racial/Ethnic Differences in Use of Health Care Services for Diabetes Management. Health. Educ. Behav. 42(6), 783–792 (2015).
- Tung EL, Baig AA, Huang ES et al. Racial and Ethnic Disparities in Diabetes Screening Between Asian Americans and Other Adults: BRFSS 2012-2014. J. Gen. Intern. Med. 32(4), 423–429 (2017).
- Bowlin SJ, Morrill BD, Nafziger AN et al. Validity of Cardiovascular Disease Risk Factors Assessed by Telephone Survey: The Behavioral Risk Factor Survey. J. Clin. Epidemiol. 46(6), 561–571 (1993).
- Karter AJ, Ferrara A, Darbinian JA et al. Self-Monitoring of Blood Glucose: Language and Financial Barriers in a Managed Care Population with Diabetes. Diabetes. Care. 23(4), 477–483 (2000).
- Karter AJ, Ackerson LM, Darbinian JA et al. Self-Monitoring of Blood Glucose Levels and Glycemic Control: The Northern California Kaiser Permanente Diabetes Registry. Am. J. Med. 111(1), 1–9 (2001).