Case Report - Interventional Cardiology (2021)
Two-stage endovascular treatment of a patient with hemodynamic interrupted aortic arch in segment A and bicuspid aortic valve
- Corresponding Author:
- Kostiantyn Boyko
Heart Institute,
Ministry of Health,
Kyiv,
Ukraine,
E-mail: dmitriy.loskutov96@gmail.com
Received date: January 11, 2021 Accepted date: February 03, 2021 Published date: February 10, 2021
Abstract
This clinical case represents an experience of two-stage endovascular repair of Complete Interrupted Aortic Arch (CIAA) in segment A in a 21-year-old patient.
Upon admission to clinic, the patient was diagnosed with CIAA and bicuspid aortic valve. Aortography showed CIAA distally from the origin of the left subclavian artery. At the first stage of treatment, CIAA on-site perforation was performed followed by PTFE (polytetrafluoroethylene)-coated CP STENT 45 mm system implantation using BIB (Balloon-in-Balloon) catheter.
The second intervention stage was performed 10 months after the first stage using balloon dilatation of stented segment with AndraBalloon 12.0 mm × 20.0 mm and 14.0 × 40.0 mm.
The residual maximum pressure gradient in descending aorta after our treatment was 10 mm Hg.
Three years after the treatment the patient has no symptoms of CIAA or coarctation, the patient does not take any antihypertensive drugs, and the pressure on the upper limbs is 125/85 mm Hg.
Keywords
Interrupted aortic arch • Bicuspid aortic valve • Refractory hypertension • Aortic coarctation
Introduction
Complete Interrupted Aortic Arch (CIAA) is a rare congenital abnormality defined as a complete loss of anatomical continuity between the ascending and descending parts of aorta. Up to 98% of similar cases are associated with additional cardiovascular anatomical defects [1]. Overall, this abnormality accounts for approximately 1% of critical congenital heart diseases [2]. Only few IAA cases in adults have been described in the scientific literature [3]. The authors describe a rare case of two-stage endovascular treatment in 21-year-old patient with IAA in segment A and bicuspid aortic valve with good clinical outcome.
Materials and Methods
Patient history
Patient 21 years old with a history of refractory hypertension from early childhood, underwent regular medical examination. At the time of physical examination, the patient complained of recurrent pain and leg weakness. A systolic murmur was heard during the auscultation of the heart in aortic valve projection. Blood pressure on the upper limbs was 140/90 mm Hg, lower limbs-90/60 mm Hg.
Patient was hospitalized. Laboratory studies showed no significant changes, including biomarkers of myocardial necrosis. 12-lead electrocardiogram showed early ventricular repolarization syndrome. Dopplerographic examination of renal vessels showed no findings for stenotic process in the main artery trunks and vasorenal hypertension. In addition, no pathology detected during ultrasonic examination of the abdominal cavity and thyroid gland. The patient had no signs of cardiofacial syndrome. The presence of refractory hypertension, a large difference in pressure on the upper and lower limbs, as well as the lack of data for pathology in other organs and systems suggested possible aortic coarctation.
Echocardiography showed aortic coarctation with Δp in descending aorta of 35 mm Hg, bicuspid aortic valve with aortic insufficiency of 1 degree.
Chest CT scan showed signs of abnormal thoracic aorta development: local hypoplasia site in the aortic arch with a critical lumen diameter (presumably with interruption of the lumen).
The patient underwent aortography to confirm diagnosis. Aortographic findings showed hemodynamic CIAA in segment A with Δp 50 mm Hg.
Operative technique
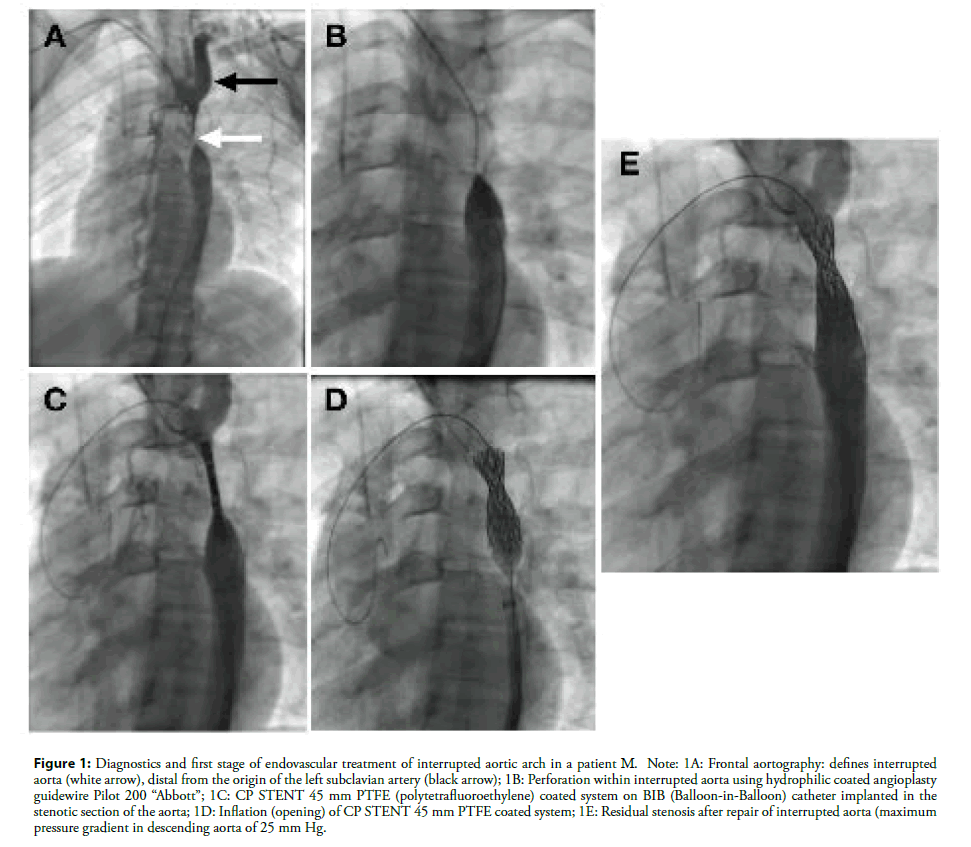
Following surgical case conference it was decided to conduct a two-stage endovascular intervention with recanalization and stenting CIAA using a CP STENT 45 mm PTFE-coated stent system (Figure 1).
Figure 1: Diagnostics and first stage of endovascular treatment of interrupted aortic arch in a patient М. Note: 1A: Frontal aortography: defines interrupted aorta (white arrow), distal from the origin of the left subclavian artery (black arrow); 1B: Perforation within interrupted aorta using hydrophilic coated angioplasty guidewire Pilot 200 “Abbott”; 1C: CP STENT 45 mm PTFE (polytetrafluoroethylene) coated system on BIB (Balloon-in-Balloon) catheter implanted in the stenotic section of the aorta; 1D: Inflation (opening) of CP STENT 45 mm PTFE coated system; 1E: Residual stenosis after repair of interrupted aorta (maximum pressure gradient in descending aorta of 25 mm Hg.
Endovascular treatment was performed in the presence of a surgical team for emergency thoracotomy using prepared heartlung apparatus.
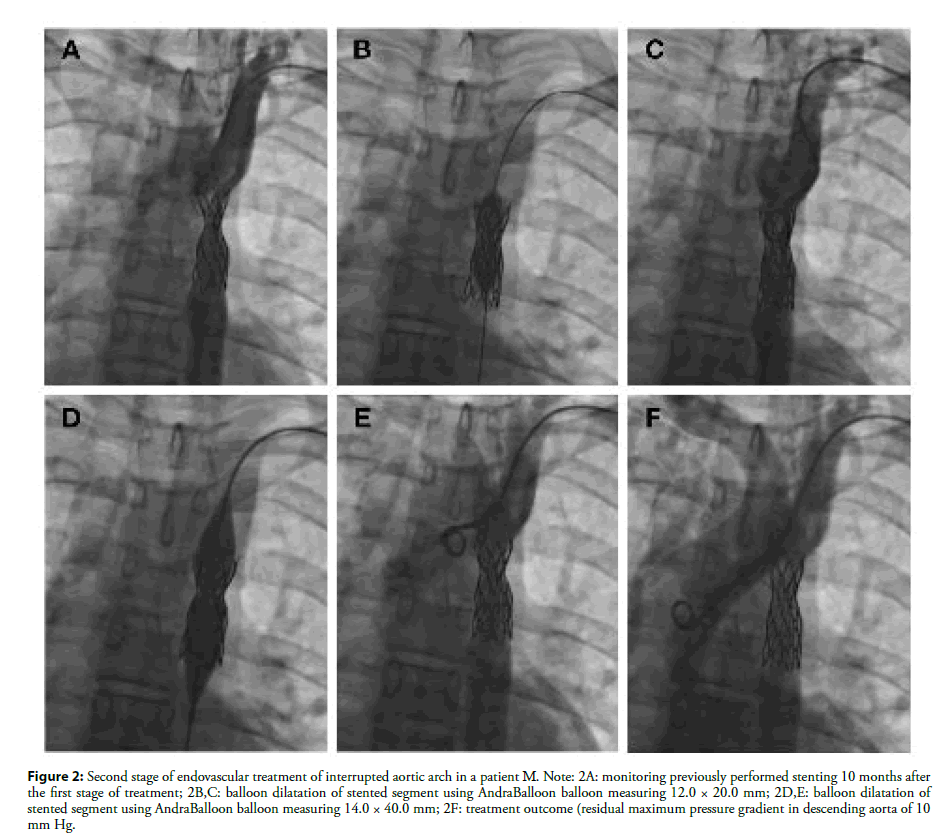
The second intervention stage was performed 10 months after the first stage using balloon dilatation of stented segment with AndraBalloon 12.0 mm × 20.0 mm and 14.0 × 40.0 mm (Figure 2).
Figure 2: Second stage of endovascular treatment of interrupted aortic arch in a patient М. Note: 2A: monitoring previously performed stenting 10 months after the first stage of treatment; 2B,C: balloon dilatation of stented segment using AndraBalloon balloon measuring 12.0 × 20.0 mm; 2D,E: balloon dilatation of stented segment using AndraBalloon balloon measuring 14.0 × 40.0 mm; 2F: treatment outcome (residual maximum pressure gradient in descending aorta of 10 mm Hg.
The residual maximum pressure gradient in descending aorta after our treatment was 10 mm Hg.
Three years after the treatment the patient has no symptoms of CIAA or coarctation, the patient does not take any antihypertensive drugs, and the pressure on the upper limbs is 125/85 mm Hg.
Discussion
We presented a rare case of a 21-year-old patient with CIAA in segment A in combination with a bicuspid aortic valve, who underwent elective endovascular treatment of this disease.
This abnormality was first classified by Celoria and Patton in 1959 [4]. Based on this classification, CIAA is divided into three different types depending on the location of interrupted aorta: type A is distal to the origin of the Left Subclavian Artery (LSA), type B is located between the Left Common Carotid Artery (LCCA) and LSA, and type C–between innominate artery and LCCA [5]. According to Patel et al. studies, type B CIAA is most common in newborns (53%) and associates with cardiofacial syndrome and deletion of chromosome 22q11.2 [5]. According to Gordon et al., type A is more common in adults (79%) [3].
As shown by Silva et al, the survival rate of such patients and degree of disability depend on the development of collaterals. Moreover, the presence of arterial duct, which gradually closes in childhood, is crucial for the development of this collateral network [6].
There are various surgical options for correction depending on the anatomy and interruption site. The main purpose of CIAA surgery is to recover aorta patency and correct concomitant cardiovascular abnormalities, preferably in a one-stage procedure [9]. One-stage CIAA recovery was described for the first time by Barratt-Boyes [7]. The procedure described by author in 1972 provided for arc continuity repair using a synthetic prosthesis. Trusler described one-stage repair involving straight arch anastomosis for the first time in 1975 [8].
According to Krishna et al. studies, extra-anatomical shunting is the preferred method due to complexity of surgical correction associated with the risk of massive blood loss due to developed collateral vessels network [10]. According to Hudsmith et al., only 8% of patients undergo percutaneous perforation with a guidewire through stenotic region of CIAA followed by placement of a drug-eluting stent. This procedure can be performed where the data available on aorta integrity on both sides of CIAA [11]. In addition, prior this type of intervention, it is necessary to notify the surgical team of possible complications.
Conclusion
We presented a clinical case of endovascular treatment of an adult patient with a combined CIAA and bicuspid aortic valve. Although CIAA may be fatal in early childhood, patients without shunting lesions can live up to adulthood with adequate development of collateral blood supply. The location of occlusion, thoracic aorta morphology, concomitant cardiovascular abnormalities, and patient’s condition play a key role in deciding on treatment tactics in such patients.
Declaration of Conflicting Interests
The authors declare no conflicts of interest and do not have any financial disclosures.
Funding
The author(s) received no financial support for the research, author- ship, and/or publication of this article.
References
- Erden I, Osman K, Erden EC, et al. Silent interrupted aortic arch in an elderly patient. Cardiol J. 18(6): 695–697 (2011).
- Friedman K. Preoperative physiology, imaging, and management of interrupted aortic arch. Semin Cardiothorac Vasc Anesth. 22(3): 265-269 (2018).
- Gordon EA, Person T, Kavarana M, et al. Interrupted aortic arch in the adult. J Card Surg. 26: 405-409 (2011).
- Celoria GC, Patton RB. Congenital absence of the aortic arch. Am Heart J. 58(3): 407-13 (1959).
- Patel DM, Maldjian PD, Lovoulos C. Interrupted aortic arch with post-interruption aneurysm and bicuspid aortic valve in an adult: A case report and literature review. Radiol Case Rep. 10(3): 5-8 (2015).
- Silva J, Guiomar N, Silva MP. Interrupted aortic arch in an adult. EJCRIM. 4 (2017).
- Barratt-Boyes BG, Nicholls N, Brandt PW, et al. Aortic arch interruption associated with patent ductus arteriosus, ventricular septal defect, and total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg. 63(3): 367-373 (1972).
- Trusler GA, Izukawa T. Interrupted aortic arch and ventricular septal defect. Direct repair through a median sternotomy incision in a 13-day-old infant. J Thorac Cardiovasc Surg. 69(1): 126-131 (1975).
- Sakellaridis T, Argiriou M, Panagiotakopoulos V, et al. Latent congenital defect: Interrupted aortic arch in an adulte case report and literature review. Vasc Endovascular Surg. 44(5): 402 (2010).
- Krishna SC, Bhan A, Sharma S, et al. Interruption of aortic arch in adults: Surgical experience with extra-anatomic bypass. Tex Heart Inst J. 32(2): 147-50 (2005).
- Hudsmith LE, Thorne SA, Clift PF, et al. Acquired thoracic aortic interruption: Percutaneous repair using graft stents. Congenit Heart Dis. 4(1): 42-5 (2009).