Case Report - International Journal of Clinical Rheumatology (2021) Volume 16, Issue 8
Ultrasound findings in Reactive arthritis after COVID-19: Case Report
- *Corresponding Author:
- Jaime Mendoza Torres
Department of musculoskeletal ultrasound applied to rheumatology, EMET Clinic, Veracruz, Mexico
E-mail: jaime.mendoza.torres.86@gmail.com
Abstract
Reactive arthritis is classified in the group of spondyloarthritis, it has been frequently associated with bacterial infections, however, it has also been linked with viral infections. Recently, different patterns of arthritis have been reported in convalescent COVID-19 patients, with involvement of large and small joints. We report the first case of post-covid 19 arthritis evaluated with ultrasound, highlighting the examination of tendons and entheses. We found an asymmetric polyarticular inflammatory pattern characterized by synovial hypertrophy, effusion, tenosynovitis, and ultrasound signs of enthesitis, based on OMERACT definitions. Ultrasound is a tool that has greater sensitivity than physical examination for the diagnosis as well as for the follow-up of patients with autoimmune diseases.
Introduction
Reactive Arthritis (ReA) is classified as a subtype spondyloarthritis, is characterized by sterile joint inflammation triggered by a distant infection in susceptible hosts. Conventionally, it has been associated with sexually transmitted and gastrointestinal diseases, as well as viral infections [1]. COVID-19 infection induces an excessive or uncontrolled host immune response, elicited by T-cell activation, effector cytokine production and the chemotaxis of neutrophils, mechanisms that also characterize the COVID-19 infection induces an excessive or uncontrolled immune response of the host, caused by the activation of T cells, the production of effector cytokines and the chemotaxis of neutrophils, mechanisms that also characterize synovial proliferation in inflammatory arthropathies [2]. ReA typically manifests asymmetric monoarthritis or oligoarthritis involving lower limbs, usually occurs 1 weeks to 3 weeks after a viral or bacterial infection [3].
Musculoskeletal Ultrasound (MSUS) is a tool with greater sensitivity than physical examination to detect synovitis and other soft tissue alterations, mainly in the evaluation of tendons and entheses. Gray Scale (GS) ultrasound identifies synovial hypertrophy and effusion. Additionally, Power Doppler (PD) ultrasound depicts neoangiogenesis within synovia, remarking local inflammation [4, 5].
We report the Ultrasound (US) findings in male patient with reactive arthritis after SARS-CoV- 2 infection. Is the first case of reactive arthritis after COVID-19 that demonstrates musculoskeletal alterations by USA.
Case
A 42-years-old patient presented to rheumatology outpatient clinic with acute development of asymmetric oligoarthritis predominantly in large joints, enthesitis and dactylitis that started 14 days after recovery from COVID-19 infection; SARS-CoV-2 PCR was positive from nasopharyngeal swab specimen. The affected joints were knee, ankle, radiocarpal joint, in addition to Aquilles tendon enthesis.
Laboratorial findings were as follows: Leucocyte: 3,700 K/Ul,neutrophil: 3,100 K/ Ul, total lymphocytes: 827, hemoglobin: 13.1 gr/dl, platelets: 247.000 K/Ul, creatinine: 0,7 mg/dl, CRP: 12.4 mg/L, sedimentation: 16 mm/h. Autoantibodies were measured: HLA-B27 Rheumatoid factor, anti-CCP, Anti-Nuclear Antibodies (ANAs), anti-SSA/ Ro, and SSB/La were found to be negative.
Hepatitis B virus surface antigen, anti-hepatitis C virus antibodies and anti-human immunodeficiency virus antibodies were negative. Gonococcal and Chlamydia trachomatis urine PCR were also negative.
The US assessment and scanning technique included evaluation of synovial sites: (wrist-radiocarpal joints, 2 - 3 Metacarpophalangeal (MCP) joints and 2-3 Proximal Interphalangeal Joint (PIP), dorsal side and palmar side; knee-suprapatellar recess, lateral and medial parapatellar recess. Ankle-tibiotalar joint, tibialis posterior tendon, peroneal tendons. Foot-metatarsophalangeal (MTP) joints 2-5.
Enthesis: Cuadriceps tendon, pattelar and Achilles tendon. Gray Scale (GS) and Power Doppler (PD) were graded according to a 0-3 semi-quantitative score depending on their severity according to the OMERACT definitions, in each joint, the presence of Synovial Effusion (SE) and Synovial Hypertrophy (SH) and intra-articular PD signal were registered. Entheses were explored in search of alterations in their echostructure, thickening, bone erosion, calcification and power Doppler signal.
Hands and wrists
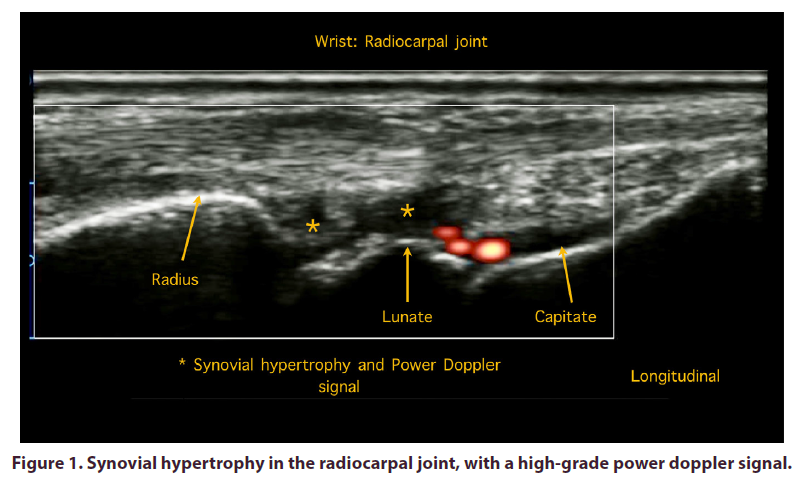
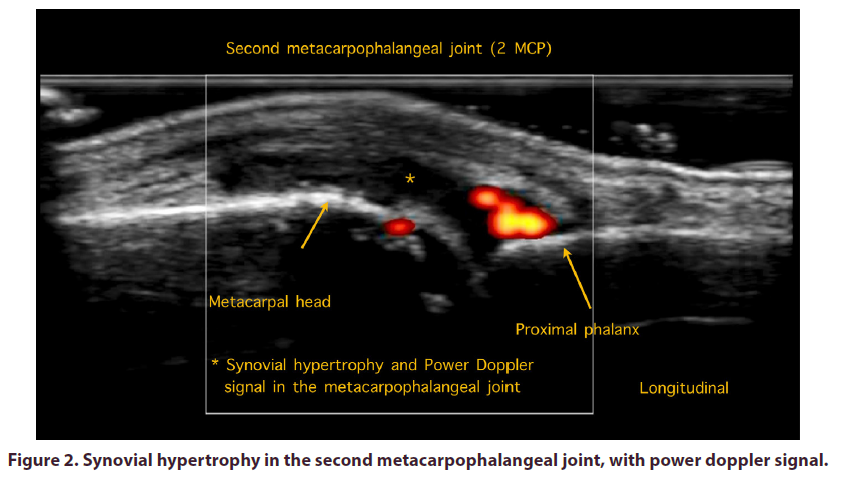
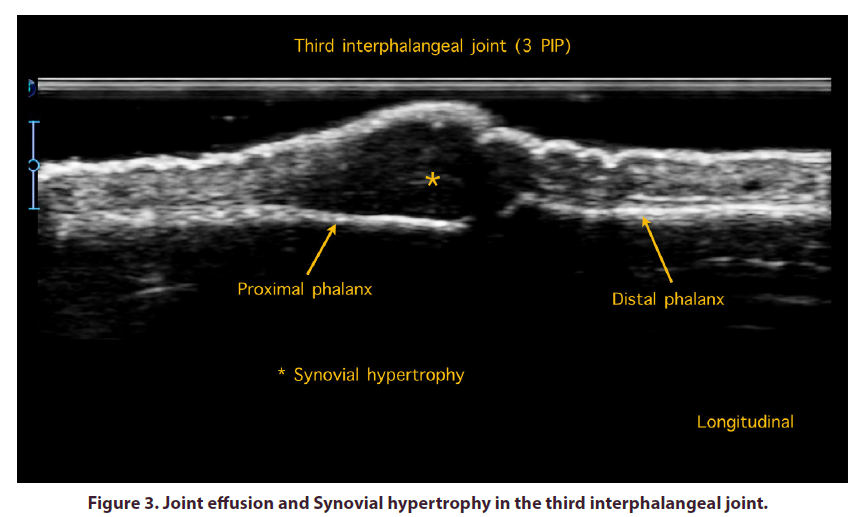
In the hands, the Grayscale Scan (GS) showed synovial hypertrophy in the radiocarpal joint, as well as in the proximal metacarpophalangeal and interphalangeal joints (Figures 1-3) with a high-grade power Doppler signal, which correlates with neovascularization associated with an active autoimmune response.
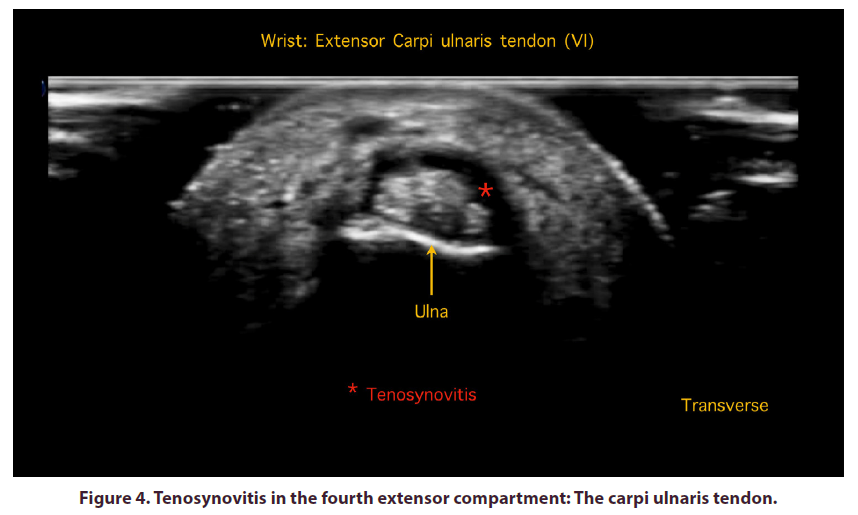
Tenosynovitis of the extensor compartments of the wrist was observed, mainly of the common extensor (IV) and the Carpi Ulnaris tendon (VI), frequent alterations in different early inflammatory arthropathies (Figure 4).
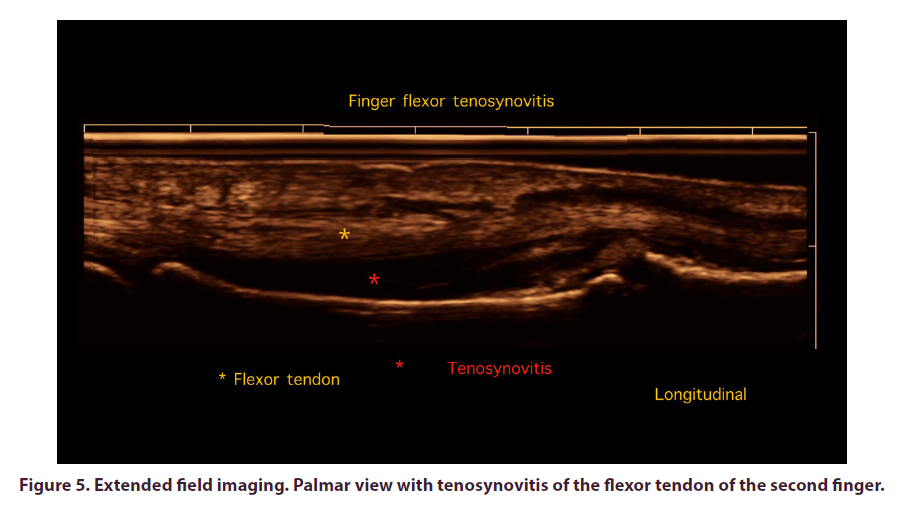
In the palmar view, tenosynovitis of the flexor tendons of the second and third fingers of both hands was observed (Figure 5), which clinically manifested as morning stiffness and decreased grip strength.
Knees
Asymmetric synovitis of the bilateral suprapatellar recess and parapatellar recess was observed in the knees (Figure 6).
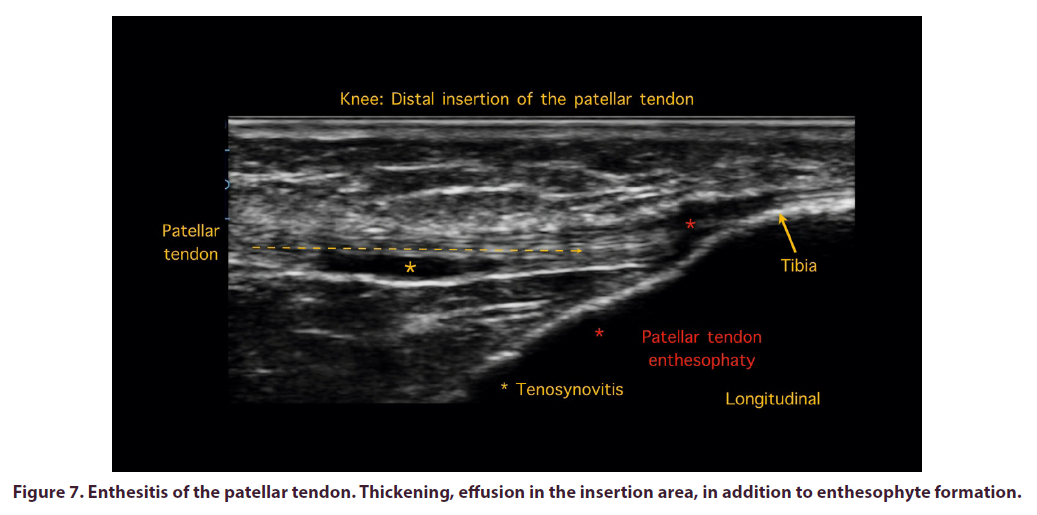
Also found enthesitis of the quadriceps tendon and the distal portion of the patellar tendon. Among the observed changes, tendon thickening, effusion in the insertion area, in addition to enthesophyte formation was found (Figure 7).
Ankles
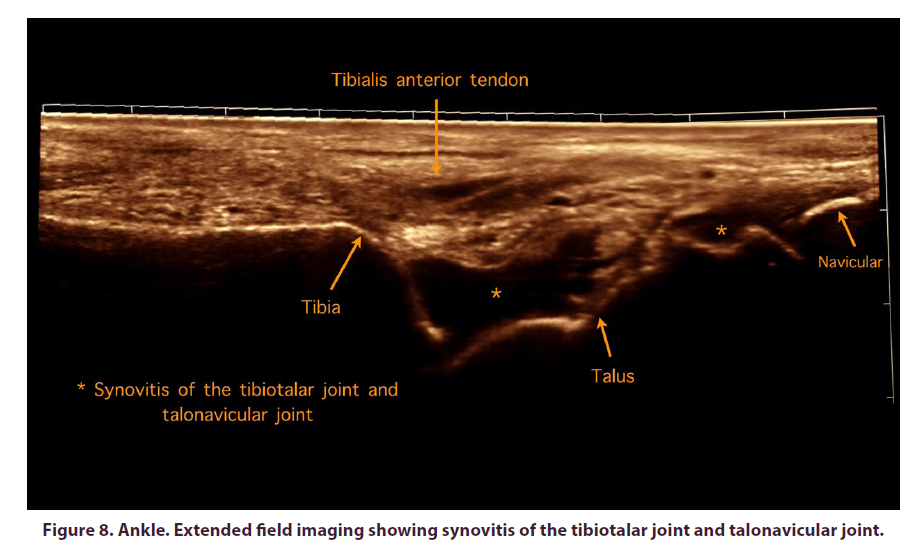
In the scan of the tibiotalar joint, synovial effusion was observed (Figure 8), in addition to tenosynovitis of the posterior tibial bone in the medial view and of the peroneal tendons (long and short) in the lateral view.
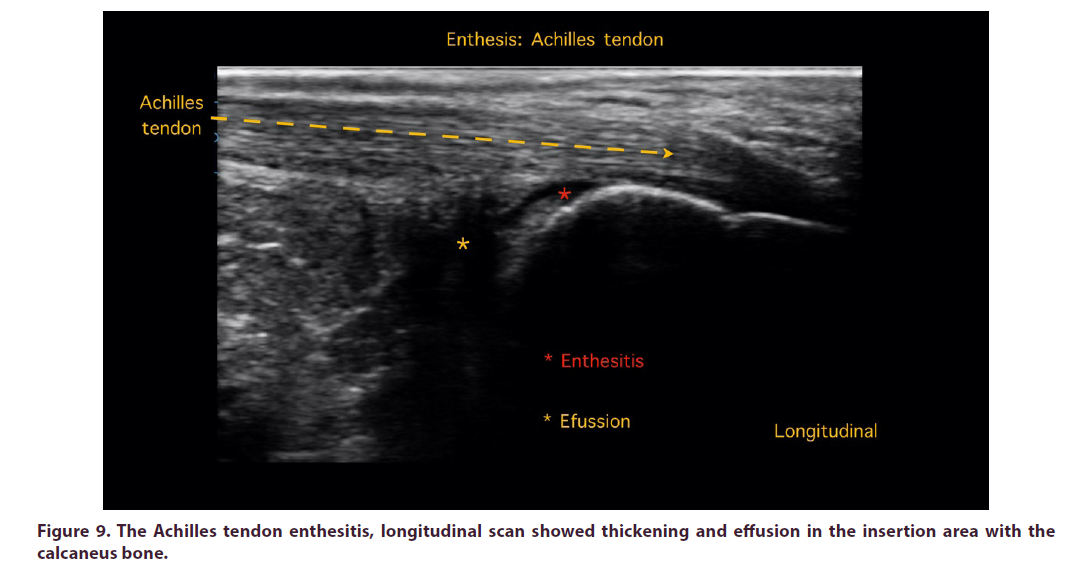
Additionally, the Achilles tendon scan showed thickening and effusion in the insertion area with the calcaneus, characteristic changes of enthesitis, which mimic the peripheral alterations characteristic of spondyloarthritis (Figure 9).
Feet
No alterations in echogenicity were observed in the ultrasound evaluation of the second and fifth metatarsophalangeal joints, in the plantar view we did not found flexor tenosynovitis.
Patient did not complete classification criteria for other autoimmune rheumatic diseases and infectious causes of arthritis were objectively excluded, because of a typical pattern of clinical presentation, he was diagnosed with reactive arthritis secondary to COVID-19 infection. Treatment with non-steroidal anti-inflammatory drugs and oral glucocorticoids was started, with complete resolution of symptoms 6 weeks after onset.
Discussion
The potential of COVID-19 infection to induce an uncontrolled immune response and generate clinical manifestations of autoimmunity in different organs and systems has been reported since the beginning of the pandemic [2, 6,7].
Ono K, et al. reported the first case of reactive arthritis after a COVID-19 infection, describing a presentation of symmetric arthritis y enthesitis [8]. Jali I, described a new case with arthritis in the small joints of the hands [9]. We use ultrasound as a more sensitive method than physical examination to document joint, tendon and enthesis alterations. We observed an asymmetric polyarticular inflammatory pattern with ultrasound changes that show synovial hypertrophy and neovascularization characterized by a variable degree power Doppler signal, according to the OMERACT definitions. The ultrasound signs of calcaneal and patellar tendon enthesopathy mimic the changes in entheses observed in patients with spondyloarthritis; however, the patient had no lumbar pain or evidence of sacroiliitis, the HLA B27 was negative.
The limitations that exist for our report is that there is still no standardized definition for the series of musculoskeletal clinical manifestations that begin after COVID-19 infection, however with the accelerated number of new cases reported in the literature, a consensus to construct a case definition as reactive arthritis or simply arthritis post-COVID 19.
Conclusion
Ultrasound is a low-cost, patient-friendly tool with greater sensitivity than physical examination for the objective detection and characterization of arthritis patterns after COVID-19 infection.
References
- Selmi C, Gershwin ME. Diagnosis and classification of reactive arthritis. Autoimmun. Rev. 13(4–5), 546–549 (2014).
- Gupta A, Madhavan MV, Sehgal K et al. Extrapulmonary manifestations of COVID–19. Nat. Med. 26(7), 1017–1032 (2020).
- Wendling D, Prati C, Chouk M et al. Reactive Arthritis: Treatment Challenges and Future Perspectives. Curr. Rheumatol. Rep. 22(7), 29 (2020).
- Joshua F, Lassere M, Bruyn GA et al. Summary findings of a systematic review of the ultrasound assessment of synovitis. J. Rheumatol. 34, 839–847 (2007).
- D'Agostino MA. Enthesitis detection by ultrasound: where are we now?. Clin. Exp. Rheumatol. 36:114(5), 127–130 (2018).
- Chen N, Zhou M, Dong X et al. Epidemiologicalandclinical characteristics of 99 cases of 2019 novel coronaviruspneumonia in Wuhan, China: a descriptive study. Lancet. 395, 507–513 (2020).
- Saricaoglu EM, Hasanoglu I, Guner R. The first reactive arthritis case associated with COVID–19. J. Med. Virol. 93(1), 192–193 (2021).
- Ono K, Kishimoto M, Shimasaki T et al. Reactive arthritis after COVID–19 infection. RMD. Open. 6(2), e001350 (2020).
- Jali I. Reactive Arthritis After COVID–19 Infection. Cureus. 12(11), e11761 (2020).