Research Article - Clinical Investigation (2017) Volume 7, Issue 3
Utilization of informatics for integrating biology and the bedside to access preliminary outcome data of post-operative complication of spine surgery associated with diabetes mellitus
- Corresponding Author:
- Tomoko Tanaka
Division of Neurosurgery
University of Missouri School of Medicine One Hospital Drive
Columbia, Missouri 65212
E-mail: tanakat@heatlh.missouri.edu
Submitted: 04 June 2017; Accepted: 12 July 2017; Published online: 17 July 2017
Abstract
Study Design: Retrospective
Study Objective: To evaluate the utility of Informatics for Integrating Biology and the Bedside database (i2b2) of University of Missouri in comparing post-operative outcomes after spinal surgery of patients with Diabetes Mellitus (DM) to those without.
Summary of background data: Studies in cardiovascular surgery, orthopedic surgery, and spine surgery have shown an association of poor preoperative hyperglycemia control with worse outcomes. However, the details of that association are not well described. Outcomes of spine surgery gleaned from nationwide databases are not universally available; some require significant costs, while others are not always available to all investigators. Informatics for Integrating Biology and the Bedside (i2b2) is a National Institutes of Health -sponsored National Center for Biomedical Computing developed for researchers to search electronic medical records for de-identified patient data to facilitate research investigations.
Methods: The Informatics for Integrating Biology and the Bedside (i2b2) database of University of Missouri was queried for various spine surgeries using categories of Non-DM patients, DM patients, and complications.
Results: Between Jan. 1, 2000 and Sept. 30, 2015 a total of 26009 spine surgeries were performed at University of Missouri Health Care. Diabetes Mellitus (DM) was not present in 20834, with 5175 had DM. DM patients had a twofold higher incidence of wound infection, Deep Venous Thrombosis, and Urinary Tract Infection. Pulmonary Embolism and myocardial infarction were 3 times more common in DM. Stroke rate was 3.9 more likely in DM. Overall, comorbidities were 2.4 fold higher in DM. The estimated time to acquire the above data was 8 hours.
Conclusions: Informatics for Integrating Biology and the Bedside is an excellent tool to extract preliminary data to develop hypothesis, test hypothesis, and gather preliminary report in a reasonable period of time. De-identified data allows researchers to perform acquire data without IRB approval.
Keywords
Diabetes mellitus, Spine surgery, Complication, Informatics for Integrating biology and the bedside (i2b2), Outcome study, Electric medical record
Abbreviations
ACS-NSQIP: American College of Surgeons National Surgical Quality Improvement Program; AO Spine: Arbeitsgemeinschaft für Osteo-synthesefragen Spine; CMS: Center for Medicare & Medicaid Services; DVT: Deep Venous Thrombosis; DM: Diabetes Mellitus; i2b2: Informatics for Integrating Biology and the Bedside Database; ICD-9 CM: International Classification of Disease, Ninth Clinical Modification; ICD-10-CM: International Classification of Disease, Tenth Revision, Clinical Modification; IRB: Institutional Review Board; MI: Myocardial Infarction; NCBC: National Center for Biomedical Computing; NIH: National Institutes of Health; NIS: Nationwide Inpatient Sample (NIS); N2QOD: National Neurosurgery Quality and Outcomes Database; PE: Pulmonary Embolism; REDCap: Research Electronic Data Capture; UTI: Urinary Tract Infection.
Introduction
Hyperglycemia and Type 2 Diabetes Mellitus (DM) create major health issues for patients in the United States. DM is present in 29.1 million Americans, representing 9.3% of population of the United States. In 2012, 21 million people were diagnosed with DM with estimations that another 8.1 million people remain undiagnosed. Estimated direct medical costs of DM are substantial ($176 billion in 2012). Medical expenditures of patients with DM are 2.3 times higher than people without a diagnosis of DM. Hyperglycemia and associated DM are major national health care issues since the conditions contribute to serious comorbid complications in multiple organ systems, including heart disease, hypertension, cerebral vascular stroke, peripheral vascular disease, blindness, kidney failure, and neuropathy [1]. Surgical subspecialty providers are aware of the negative impact of post-operative care associated with DM patients [2]. Recent changes implemented by the Center for Medicare & Medicaid Services (CMS) penalize providers with higher rates of unplanned readmissions, creating potential financial burdens in addition to the health considerations.
Outcome studies investigating the impact of DM have been conducted in several different surgical subspecialties and critical intensive care. Cardiovascular surgery has been particularly interested in the association of hyperglycemia and surgical outcome because stress conditions induce increased levels of counter-regulatory hormones, such as glucagon, epinephrine, cortisol and growth hormone. The response affects carbohydrate metabolism, including insulin resistance, increased hepatic glucose secretion, impaired peripheral glucose utilization, and insulin deficiency [3]. These impairments lead to increased morbidity and mortality in the perioperative period.
DM is also associated with consequences after spine surgery, as illustrated in several studies comparing DM with non-DM patients’ outcomes in large nationwide databases. These studies include American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) [4,5] the Nationwide Inpatient Sample (NIS) [6], and the National Neurosurgery Quality and Outcomes Database (N2QOD) [7]. Each database is a separate system unlinked to the others. Each system is not mature enough to measure outcome metrics [8]. Acquiring data to assess preliminary data, develop hypotheses, or research planning from these database systems could be time consuming and costly, as seen in Table 1.
| American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) |
National (Nationwide) Inpatient Sample (NSI) |
Quality Outcomes Database (QOD)/ National Neurosurgery Quality and Outcomes Database (N2QOD) | Informatics for Integrating Biology and the Bedside (i2b2) |
|
| URL | www.facs.org/quality-programs/acs-nsqip | www.hcup-us.ahrq.gov/nisoverview.jsp | www.neuropoint.org | www.i2b2.org |
| Description | Nationally validated, risk-adjusted, outcomes-based approach to measure and improve the quality of surgical care. Employs prospective, peer-controlled, validated database to quantify 30-day, risk-adjusted surgical outcomes. | Part of The Healthcare Cost and Utilization Project (HCUP) Database. Developed through a Federal-State-Industry partnership and sponsored by the Agency for Healthcare Research and Quality (AHRQ). Available for purchase online. Nationwide Databases are delivered via download. State Databases are shipped on physical media (CD/DVD). | Continuous national clinical registry for neurosurgical procedures and practice patterns. Primary purposesare to track quality of surgical care for the most common neurosurgical procedures and provide practice groups and hospitals with an immediate infrastructure for analyzing and reporting the quality of neurosurgical care. | NIH-funded National Center for Biomedical Computing (NCBC) based at Partners HealthCare System in Boston, Mass. |
| Cost | $10,000 to $29,000 / year | $350 for each year result (data available since 1998) | $13,000/ year for software | N/A |
| Requirement | Require assigned trained Surgical Clinical Reviewer(SCR) | N/A | N/A | N/A |
| Utilizing code | CPT | ICD-9 CM | N/A | ICD-9 CM, ICD-10-CM |
Table 1: Database Comparisons
Informatics for Integrating Biology and the Bedside (i2b2) is a National Institutes of Health (NIH) -funded National Center for Biomedical Computing (NCBC) based at Partners Health Care System in Boston, MA. The current system is able to extract data based on International Classification of Disease, Ninth and Tenth Revision, Clinical Modification (ICD 9, 10-CM). I2b2 is a tool that researchers can use to be able to access large patient data sets to determine numbers of patients with various diagnoses and comorbidities. In searching our institutional data with i2b2, our goal was to assess the viability of investigating the relationships between DM and outcome after spine surgery. We hypothesized that i2b2 would readily identify differences between patients with DM and without DM in regards to complications after surgery.
Materials and Methods
We performed a retrospective analysis of patients in the University of Missouri Health Care System utilizing Informatics for Integrating Biology and the Bedside (i2b2).
Training
The investigator making the query registered for access to i2b2 through the University of Missouri Institute for Clinical and Translational Science [9], creating an account with the system. The investigator then participated in a free 2-hour interactive workshop lead by a faculty member of the Institute for Clinical and Translational Science. About 15-20 registered investigators gathered in the class room. The log in user name, and password were provided prior to class members. The workshop included an introductory lecture of concept of informatics for integrating biology and the bedside and the system. An interactive tutorial of the system demonstrated an example query to familiarize users with the system. The investigators then had an opportunity to practice queries. Those individuals with question or particular query needs were able to obtain separate one-on-one sessions.
Data query
Diagnostic ICD-9 CM codes were extracted by the investigator to perform the necessary data queries. In this project, key query words included “spinal surgery,” “spinal fusion,” “Diabetes Mellitus (DM),” “non-DM” and complications of “wound infection,” “myocardial infarction (MI),” “deep venous thrombosis (DVT),” “stroke,” “urinary tract infection (UTI),” and “pulmonary embolism (PE).” A data Query was conducted from 01/01/2000 through 09/30/2015. The query required 4 hours for key word and entry and data acquisition.
Results
ICD-9 CM code (Table 2) extraction required 4 h, query search for data required 6 h. Therefore, to derive the data took about 12 h which included classroom training time of 2 h by a new user. Based on the extracted ICD-9 CM code, the individual with specialize informatics training accomplish the same task who had generated 24 counts by running 24 queries. It took 6 h to create and excite the result of queries.
| ICD 9 Code | |
| Diabetes Mellitus | Diabetes mellitus without mention of complication, type II or unspecified type, not stated as uncontrolled (250.00) Diabetes mellitus without mention of complication, type I [juvenile type], not stated as uncontrolled (250.01) Diabetes mellitus without mention of complication, type II or unspecified type, uncontrolled (250.02) Diabetes mellitus without mention of complication, type I [juvenile type], uncontrolled (250.03) |
| Spinal Fusion | Spinal fusion, not otherwise specific (81.00) Atlas-axis spinal fusion ( 81.02) Other cervical fusion of the anterior column, anterior technique (81.02) Other cervical fusion of the posterior column, posterior technique (81.03) Dorsal and dorsolumbar fusion of the anterior column, anterior technique (81.04) Dorsal and dorsolumbar fusion of the posterior column, posterior technique (81.05) Lumbar and lumbosacral fusion of the anterior column, anterior technique (81.06) Lumbar and lumbosacral fusion of the posterior column, posterior technique (81.07) Lumbar and lumbosacral fusion of the anterior column, posterior technique (81.08) Insertion of interbody spinal fusion device (84.51); Insertion of recombinant bone morphogenetic protein (84.52) Fusion or refusion of 2-3 vertebrae (81.62) Fusion or refusion of 4- 8 vertebrae (81.63) Fusion or refusion of 9 or more vertebrae (81.64) |
| Wound infection | Postoperative infection (998.5) Infected postoperative seroma (998.51) Other postoperative infection (998.59) Due to unspecified device, implant and graft (996.60) Due to other internal orthopedic device, implant and graft (996.67) |
| Wound dehiscent | Non-healing surgical wound (998.83)] |
| Myocardial Infarction | Of other anterior wall (410.1) Of anterolateral wall (410.0) Of other lateral wall (410.5) Of other specified sites (410.8) Of other inferior wall (410.4) Intermediate coronary syndrome (411.1) Of inferolateral wall (410.2) Of inferoposterior wall (410.3) Subendocardial infarction (410.7) Of other specified sites (410.8) True posterior wall infarction (410.6) Unspecified site (410.9) |
| Other cardiac complication | Other specified complications (998.89) |
| Deep Venous Thrombosis | Acute venous embolism and thrombosis of unspecified deep vessels of lower extremity (453.40) Acute venous embolism and thrombosis of deep veins of upper extremity (453.82) Acute venous embolism and thrombosis of deep vessels of proximal lower extremity (453.41) Acute venous embolism and thrombosis of deep vessels of distal lower extremity (453.42) Acute venous embolism and thrombosis of upper extremity, unspecified (453.83)] |
| Pulmonary Embolism | Pulmonary embolism and infarction (415.1) Iatrogenic pulmonary embolism and infarction (415.11) Septic pulmonary embolism (415.12) |
| Stroke | Cerebral thrombosis, with cerebral infarction, Cerebral embolism, with cerebral infarction, Hypertension (997.91) Iatrogenic cerebrovascular infarction or hemorrhage (997.02) Unspecified transient cerebral ischemia (435.9) Cerebral artery occlusion, unspecified, with cerebral infarction ( 434.91) |
| Urinary Tract Infection | Urinary tract infection of newborn (771.82) Urinary tract infection, site not specified (599.0) Acute cystitis (595.0) Due to indwelling urinary catheter (996.64) |
Table 2: ICD-9 Codes of related current project
Between 01/01/2000 and 09/30/2015, 26009 spinal operations were performed at University of Missouri Health Care, which included 20834 non-DM patients and 5175 patients with DM (Table 3).
| Total Spine Cases | Spine surgery with DM (%) | Spine Surgery wo DM (%) | Odds Ratio | 95% Confidence Interval | p-value | |||
|---|---|---|---|---|---|---|---|---|
| Total case # | 26009 | 5175 (19.89) | 20834 (80.10) | N/A | N/A | N/A | N/A | |
| All comorbidity | 1679 | 632 (12.21) | 1047 (5.03) | 2.63 | 2.34 | 2.92 | <2.2e-16 | |
| DVT | 135 | 47 (0.91) | 88 (0.42) | 2.16 | 1.51 | 3.08 | 1.344e-05 | |
| MI | 383 | 172 (3.32) | 211 (1.01) | 3.36 | .74 | 4.12 | <2.2e-16 | |
| PE | 94 | 40 (0.77) | 54 (0.26) | 2.99 | 1.99 | 4.52 | 3.547e-08 | |
| Stroke | 183 | 91 (1.79) | 92 (0.44) | 4.06 | 3.02 | 5.40 | <2.2e-16 | |
| UTI | 884 | 325 (6.28) | 559 (2.68) | 2.43 | 2.11 | 2.80 | <2.2e-16 | |
| Wound Infection | 299 | 102 (1.97) | 197 (0.95) | 2.11 | 1.66 | 2.68 | 5.893e-10 | |
Table 3: Spine surgery comorbidity with/without DM comparisons
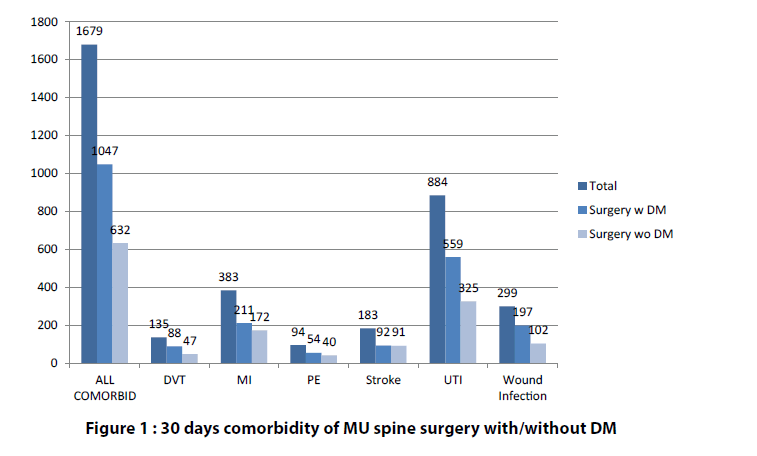
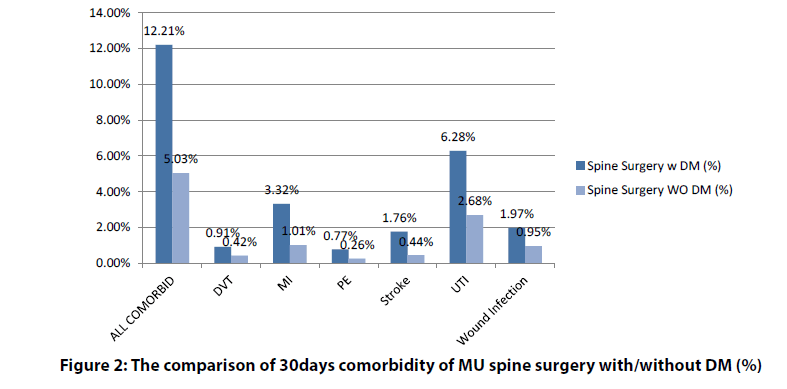
Postoperative complications within 30 days are illustrated in Figure 1 and Figure 2. Type I and Type II DM patients were combined as a single group in this review of complications. Complications were more common in the DM patients (Table 3). These complications included the following: All comorbidities 12.21% vs. 5.03% , deep venous thrombosis (DVT) 0.91% vs. 0.42%, myocardial infraction (MI) 3.3% vs. 1.01%, pulmonary embolism (PE) 0.77% vs. 0.26%, stroke 1.76% vs. 0.44% , urinary tract infection (UTI) 6.28% vs. 2.68% and wound infection 1.97% vs. 0.95% (Figure 1 and Figure 2).
Figure 1: 30 days comorbidity of MU spine surgery with/without DM
Figure 2: The comparison of 30days comorbidity of MU spine surgery with/without DM (%)
Compared to non-DM, DM patients had a twofold higher incidence of wound infection, DVT and UTI; a threefold higher incidence of PE, MI cardiac complications; and a fourfold increase of stroke (Table 3 and Figure 2).
Discussion
In this study, we show that we can quickly survey our electronic medical record database to obtain meaningful information linking diabetes mellitus to outcome after spinal fusion surgery with relatively little time using i2b2. We found that complications after spinal fusion surgery were significantly increased in patients with diabetes mellitus.
These results are similar to those seen in other studies. A number of studies of spine surgery [2,6,10-14] have reviewed the relationship between surgical outcomes and comorbidity in prediabetes and diabetes conditions. Tetreault et al. [2] surveyed 916 Arbeitsgemeinschaft für Osteosynthesefragen (AO) Spine International members of predictive perioperative complication factors; 83.1% of the participants believed DM increased perioperative mortality rates. Two other studies examined DM and spine surgery using data from a nationwide database.
Qin et al. [4] reported outcomes after lumbar spine surgery utilizing the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database, which provides information about major surgical procedures at more than 240 institutions in the United States. The ACS-NSQIP data is risk-adjusted and based on patients’ outcomes at 30 days - one of major outcome metrics of Centers for Medicare & Medicaid Services (CMS). Qin et al. 4concluded that both insulin-independent and insulin-dependent DM were associated with increased risk of 30-day medical complications [4]. Cook et al. [6] compared non-DM (n=34300) patients to those with DM (n=3432) by using Nationwide Inpatient Sample (NIS). They demonstrated significantly worse perioperative outcome and longer duration of hospitalization in uncontrolled DM compared to non- DM and controlled DM.
The major databases which have been utilized for outcome studies indicated above are ACS-NSQIP, NSI, and Quality Outcomes Database (QOD)/ National Neurosurgery Quality and Outcomes Database (N2QOD). Each database has different purpose, organization, approach and cost (Table 1). However, improvement and monitoring systems are the most basic function. Pittman et al. [15] utilized i2b2 and N2QOD to study time and cost efficiency of i2b2 and Research Electronic Data Capture (REDCap) system. They recognized errors in human data entry, the time-consuming process, and difficulty extracting accurate coding from different types of note styles, but demonstrated cost effective effectiveness with i2b2 compared to without i2b2. The i2b2 is a deidentified data query, in which investigators are not required to obtain the institutional review board (IRB) approval. Therefore, investigators may access their own institutional data and compare them to nationwide database results to test hypothesis and obtain preliminary data without IRB. Additionally, national databases have annual or request item fees. Once an institution has access to i2b2 no additional costs are accrued by individual investigators.
Through the Department of University of Missouri Institute for Clinical and Translational Science, use of i2b2 could also be extended to make data query available to other institutions which utilize informatics systems. Therefore, a query could be expanded to multiple institutions. I2b2 would be great tool to examine preliminary results and test project hypotheses. In fact, current preliminary data in this study was used for grant application subsequently awarded. Schieffer et al. [15] suggested that i2b2 could be utilized to test a predocotoral trainee curriculum, and that student generated research hypotheses could be tested. When the investigators would like to review institutional preliminary data, the result is available within a reasonable time period. When investigators would like to review individual electronical medical records, once IRB approval has been obtained, the projects can be completed.
In this study, we used i2b2 to acquire data from January 1, 2000 to September 30, 2015 in order to use ICD-9 codes for diagnoses. We made this decision since i2b2 was not initially compatible with ICD-10. This decision permitted the acquisition of the data used for our grant submission on 05/03/2016. While ICD-10 use was instituted for coding on October 1, 2015, i2b2 did not become compatible with ICD-10 until December 2016 at University of Missouri. Future studies using i2b2 to acquire preliminary data should be able to take advantage of the diagnostic accuracy of ICD-10. Some additional steps will likely be necessary to combine ICD-10-related data with ICD-9-related data, which was beyond the scope of this study.
The data acquired by i2b2 is at a fairly granular level. Access of individual patient charts will obviously require an IRB-approved study. Nevertheless, i2b2 data provides insights into the types of data to include in these further studies. The proposed approach of obtaining preliminary data without cost and time is extremely important to researchers, making i2b2 a key research tool for investigating patient outcomes.
Limitations
1. i2b2 only recently compatible with ICD-10, so analysis here was performed on ICD-9 diagnoses coding.
2. ICD-9 codes not merged with ICD-10 codes in this study. Some logistical constraints and additional steps are likely to merge that data.
3. Mortality comparisons are not possible
4. Non-coded data, such as reasons for patient appointment cancellations, cause of death, or surgical intervention, cannot be retrieved for comparison.
Conclusion
Informatics for Integrating Biology and the Bedside is a great tool to extract preliminary data, develop hypothesis, and test hypothesis in a reasonable period of time. De-identified data allows researchers to acquire data without IRB approval. The potential exists to expand its use to broader datasets involving multiple institutions.
References
- CDC. 2014 National Diabetes Statistics Report. 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.
- Tetreault L, Nouri A, Singh A, Fawcett M, Nater A, Fehlings MG. An Assessment of the Key Predictors of Perioperative Complications in Patients with Cervical Spondylotic Myelopathy Undergoing Surgical Treatment: Results from a Survey of 916 AOSpine International Members. World Neurosurg. 83: 679-690 (2015).
- Duggan EW, Klopman MA, Berry AJ, Umpierrez G. The Emory University Perioperative Algorithm for the Management of Hyperglycemia and Diabetes in Non-cardiac Surgery Patients. Curr. Diabet. Rep. 16: 34 (2016)
- Qin C, Kim JY, Hsu WK. Impact of Insulin Dependence on Lumbar Surgery Outcomes: An NSQIP Analysis of 51,277 Patients. Spine (Phila Pa 1976) 41: 687-693 (2016).
- Golinvaux NS, Varthi AG, Bohl DD, Basques BA, Grauer JN. Complication rates following elective lumbar fusion in patients with diabetes: insulin dependence makes the difference. Spine (Phila Pa 1976) 39: 1809-1816 (2014).
- Cook C, Tackett S, Shah A, et al. Diabetes and perioperative outcomes following cervical fusion in patients with myelopathy. Spine (Phila Pa 1976) 33: 254-260 (2008).
- McGirt MJ, Speroff T, Dittus RS, Harrell FE, Asher AL. The National Neurosurgery Quality and Outcomes Database (N2QOD): general overview and pilot-year project description. Neurosurg. Focus. 34: 6 (2013)
- Missios S, Bekelis K. How well do subjective Hospital Compare metrics reflect objective outcomes in spine surgery? J Neurosurg. Spine. 1-7 (2016).
- Mosa AS, Yoo I, Apathy NC, Ko KJ, Parker JC. Secondary Use of Clinical Data to Enable Data-Driven Translational Science with Trustworthy Access Management. Mol. Med. 112: 443-448 (2015).
- Satake K, Kanemura T, Matsumoto A, Yamaguchi H, Ishikawa Y. Predisposing factors for surgical site infection of spinal instrumentation surgery for diabetes patients. Eur. Spine. J. 2013; 22: 1854-1858 (2013).
- Hikata T, Iwanami A, Hosogane N, et al. High preoperative hemoglobin A1c is a risk factor for surgical site infection after posterior thoracic and lumbar spinal instrumentation surgery. J. Orthop. Sci. 19: 223-228 (2014).
- Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J. Bone. Joint. Surg. Am. 95: 1651-1658 (2013).
- Wang TY, Sakamoto JT, Nayar G, et al. Independent Predictors of 30-Day Perioperative Deep Vein Thrombosis in 1346 Consecutive Patients After Spine Surgery. World. Neurosurg. 84: 1605-1612 (2015).
- Schimmel JJ, Horsting PP, de Kleuver M, Wonders G, van Limbeek J. Risk factors for deep surgical site infections after spinal fusion. Eur. Spine. J. 19: 1711-1719 (2010).
- Schieffer KM, Peters DG, Richter CK, Loc WS, Pawelczyk JA. Incorporating Informatics for Integrating Biology and the Bedside (i2b2) into Predoctoral Trainee Curriculum to Evaluate Student-Generated Hypotheses. Clin. Transl. Sci. 8: 729-733 (2015).