Commentary - Interventional Cardiology (2015) Volume 7, Issue 4
Ventricular premature depolarization ablation and reversal of nonischemic cardiomyopathy
- Corresponding Author:
- Francis E
Marchlinski
2Electrophysiology Section, Cardiovascular Division, Hospital of the University of Pennsylvania
9 Founders Pavilion, 3400 Spruce St, Philadelphia, PA 19104, USA
Tel: +1 215 662 6005
Fax: +1 215 662 2879
E-mail: Francis.Marchlinski@uphs.upenn.edu
Abstract
“...targeted catheter ablation represents a potential therapeutic option to reverse a cycle of worsening HF and deteriorating LV function.”
Keywords
cardiomyopathy, catheter ablation, heart failure, tachycardia, ventricular premature depolarization, ventricular tachycardia
Ventricular premature depolarization (VPD)-induced cardiomyopathy is a condition in which frequent ventricular ectopic impulses result in left ventricular (LV) dysfunction leading to systolic heart failure (HF) [1–3]. The causal relationship between VPDs and nonischemic cardiomyopathy (NICM) has been firmly established based on the reversal of the cardiomyopathy with elimination of VPDs using medications or, more commonly, catheter ablative therapy [4]. Recognition of the potential risk of VPDs for producing LV dysfunction is essential to provide proper treatment that can improve LV ejection fraction (LVEF).
VPDs can be due to abnormal impulse formation, triggered activity or reentry [5,6]. However, much of the natural history and pathophysiology of VPD-related ventricular dysfunction remains unknown. In the past, even frequent VPDs were considered to be benign. This affirmation was based on limited clinical studies [7]. It is now recognized that VPDs can initiate or exacerbate acute HF in patients with preexisting structural heart disease (VPD-induced worsening) or can be the sole reason for ventricular dysfunction (VPD-mediated).
The animal model based on chronic rapid pacing has long been recognized to cause depressed LV function and frank HF [8]. Chronic rapid pacing induces adverse LV remodeling and neurohormonal activation. Chronic rapid pacing in the animal model also has been demonstrated to induce several proapoptotic cascades, LV myocyte remodeling and alteration in excitation–contraction [9–11]. However, the mechanism of the relation between VPDs and depression of LV function is not fully understood. One animal study suggested that VPD-induced NICM could be primarily functional rather than a fixed abnormality and therefore in large part reversible with VPD elimination [12]. Ventricular dyssynchrony and increased oxygen consumption with VPDs are two of the other proposed mechanisms. In an animal model, pacing to produce bigeminy could indeed induce a cardiomyopathy that was reversible without structural changes of the myocardium [12]. There remains a critical need to more completely understand the physiologic, molecular and cellular cause of VPDinduced/ worsened cardiomyopathy. Many patients with frequent VPDs will not develop a cardiomyopathy.
Several clinical predictors of VPD-induced cardiomyopathy (VPD CM) have been identified. Classically, a high VPD burden of more than 24% has been associated with impaired LVEF [13]. A longitudinal study found subclinical deterioration in LV function over 5 years in those with a high burden of VPDs (≥10–20%) [14]. Despite the absence of a definitive cutoff, the risk of developing NICM appears to be greater with a higher VPD burden. A threshold of approximately 10,000 VPDs/day appears required to induce NICM [13]. Other factors suggested to confer an increased risk of developing NICM include male sex, increased BMI, asymptomatic nature of VPDs, shorter VPD coupling interval (600 ms), an epicardial origin, interpolated VPDs and the presence of retrograde p waves [15–17]. Furthermore, patients developing VPDNICM were more likely to be asymptomatic or had prolonged palpitations (>60 months) [18]. One study indicated that patients with VPDs of right ventricular origin have a higher risk to develop NICM [19]. However, a recent study has convincingly demonstrated that VPDs from nonoutflow tract sites can also induced a NICM [13]. In a retrospective analysis, Deyell et al. demonstrated that QRS duration was an independent predictor of lack of recovery of LV function after successful ablation of VPDs [20]. The authors suggest that an increase in VPD duration might be a marker for an increase in fiber disarray due to microfibrosis and these patients with subclinical cardiac pathology may be predisposed to developing decreased function with the stress of frequent VPDs. In a recent longitudinal study, Carballeira et al. systematically evaluated the risk factors implicated in the development of VPDs CM in patients with more than 10,000 VPDs/day. QRS duration longer than 153 ms and a nonoutflow tract site of origin were associated with the subsequent development of VPD CM. Interestingly, the absolute arrhythmia burden was not associated with development of LV dysfunction in that study [21].
VPD CM is largely underrecognized and for that reason the true prevalence is unknown. Some authors have stated that it can represent 34% of patients referred for electrophysiological evaluation of VPDs [22]. The diagnosis should be suspected in any patient who presents with frequent VPDs in the presence of an otherwise unexplained cardiomyopathy. Since many patients are asymptomatic, the presentation can be late only after manifest systolic HF develops. Sometimes, it can be extremely difficult to determine whether the frequent VPDs are the initiator or the consequence of a NICM. Frequently VPDs are considered secondary and not treated aggressively. It should be noted that adequate VPD control is necessary for significant recovery.
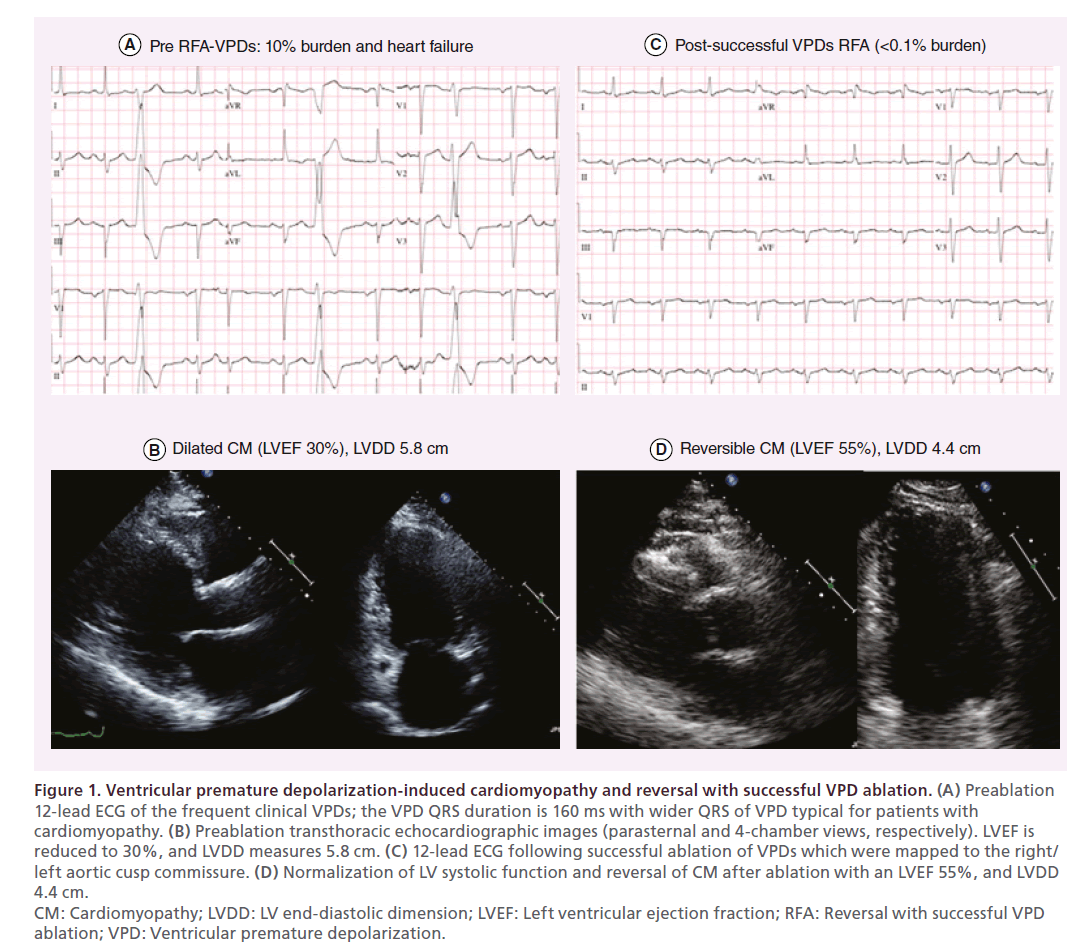
The management of VPDs in NICM is based on eliminating most if not all of the VPDs, with the goal of improving HF symptoms and reversing LV dysfunction. A favorable response to arrhythmia elimination with improvement in LV function ultimately confirms the diagnosis of VPD CM (Figure 1). Not only arrhythmia control but also standard medical treatment with vasodilators and beta-blockers can mitigate the abnormal neurohormonal response and aid in positive remodeling. In many cases, the correct diagnosis (VPD CM vs NICM with frequent VPDs) may only be evident after restoration and maintenance of sinus rhythm.
Figure 1: Ventricular premature depolarization-induced cardiomyopathy and reversal with successful VPD ablation. (A) Preablation
12-lead ECG of the frequent clinical VPDs; the VPD QRS duration is 160 ms with wider QRS of VPD typical for patients with
cardiomyopathy. (B) Preablation transthoracic echocardiographic images (parasternal and 4-chamber views, respectively). LVEF is
reduced to 30%, and LVDD measures 5.8 cm. (C) 12-lead ECG following successful ablation of VPDs which were mapped to the right/
left aortic cusp commissure. (D) Normalization of LV systolic function and reversal of CM after ablation with an LVEF 55%, and LVDD
4.4 cm.
CM: Cardiomyopathy; LVDD: LV end-diastolic dimension; LVEF: Left ventricular ejection fraction; RFA: Reversal with successful VPD
ablation; VPD: Ventricular premature depolarization.
The reversal of the cardiomyopathy with catheter ablation has been firmly established by Mountantonakis et al. with over 90% of patients achieving long-term VPD control [23]. Importantly, they also noted that a reduction in VPD burden by 80% has comparable improvement in LV function to complete VPD elimination. A threshold reduction to less than 5000 VPDs/ day appears required for improvement [4]. Regarding the efficacy of catheter ablation for eliminating VPDs, a recent trial randomized 330 patients with normal LVEF and right ventricular outflow tract VPDs to either medical therapy or ablation. Elimination of VPDs at 1 year was achieved in 80% of the ablation group versus 12% of the medical group. The ablation group had a 2% incidence of minor complications that all resolved completely before discharge versus 10% in the medical group [24]. Multiple important observational studies support the findings of the randomized study and point to a potential for an even higher success rate at experienced centers [17,19–24].
Elimination of VPDs with ablation has been shown to improve LVEF, ventricular dimensions, functional mitral insufficiency and quality of life [19–25]. It should be noted that elimination of high VPDs burden (>10%) in patients with impaired LVEF could be associated with improvement of LVEF even when structural cardiac abnormalities are present [4,20,25]. Regarding the time to normalization of LVEF, in a study of 75 patients with VPD CM who had successful catheter ablation, the mean time to normalization of LVEF was 5 ± 6 months, with 68% recovering by 4 months [26]. Several articles have been published recently trying to identify markers for the irreversibility of LVdilated cardiomyopathy in patients with VPDs or VT. Campos et al. described that a unipolar abnormality area cutoff of greater than 32% of total LV surface (<8.27 mV) was 96% sensitive and 100% specific in identifying significant irreversible cardiomyopathy among patients with LV dysfunction [23].
In patients with cardiomyopathy and previously implanted biventricular pacemaker or defibrillator, VPDs can decrease the amount of biventricular pacing to suboptimal levels and lead to an inadequate response to cardiac resynchronization [23]. A decrease in biventricular pacing to less than 98% has been associated with adverse outcomes [27]. It has been shown that CRT can be optimized by VPD ablation in patients with frequent PVCs (>10,000/24 h) [28].
Despite the effort to identify associated risk factors and the success of catheter ablation, the use of catheter ablation before the development of LV dysfunction is not recommended in the current HRS/ESC guidelines regarding the use of VT ablation in patients with frequent asymptomatic VPDs [29]. Clearly, higher risk patients: those with VPD burden greater than 10,000 and VPD QRS duration greater than 150 ms warrant close longitudinal follow-up with repeat echocardio graphic imaging. Any change in LV chamber size and/ or decrease in LV function should be managed aggressively, which includes strong consideration for catheter ablation.
NICM caused by frequent VPDs is an important and often underrecognized but potentially reversible cause of HF and cardiomyopathy. Early recognition of the arrhythmia and successful elimination with targeted catheter ablation represents a potential therapeutic option to reverse a cycle of worsening HF and deteriorating LV function.
Financial & competing interests disclosure
This work was funded in part by a grant for international research, Horlait-Dapsens Foundation, Belgium (RCA) and the Richard T and Angela Clark Clinical Innovation Fund for Electrophysiology. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Kostis JB, McCrone K, Moreyra AE et al. Premature ventricular complexes in the absence of identifiable heart disease. Circulation 63(6), 1351–1356 (1981).
- Bjerregaard P. Premature beats in healthy subjects 40–79 years of age. Eur. Heart J. 3(6), 493–503 (1982).
- Bikkina M, Larson MG, Levy D. Prognostic implications of asymptomatic ventricular arrhythmias: the Framingham Heart Study. Ann. Intern. Med. 117(12), 990–996 (1992).
- Mountantonakis SE, Frankel DS, Gerstenfeld EP et al. Reversal of outflow tract ventricular prematuredepolarization-induced cardiomyopathy with ablation: effect of residual arrhythmia burden and preexisting cardiomyopathy on outcome. Heart Rhythm 8(10), 1608–1614 (2011).
- Lerman BB, Stein K, Engelstein ED et al. Mechanism of repetitive ventricular tachycardia. Circulation 92(3), 421–429 (1995).
- January CT, Riddle JM. Early after depolarizations: mechanism of induction and block. A role for L-type Ca2+ current. Circ. Res. 64(5), 977–990 (1989).
- Kennedy HL, Whitlock JA, Sprague MK et al. Long-term follow-up of asymptomatic healthy subjects with frequent and complex ventricular ectopy. N. Engl. J. Med. 312(4), 193–197 (1985).
- Whipple GH, Sheffield LT, Woodman EG, Thoephilis C, Friedman S. Reversible congestive heart failure due to rapid stimulation of the normal heart. Proc. New Engl. Cardiovasc. Soc. 20, 39–40 (1961–1962).
- Armstrong PW, Stopps TP, Ford SE, de Bold AJ. Rapid ventricular pacing in the dog: pathophysiologic studies of heart failure. Circulation 74(5), 1075–1084 (1986).
- Wilson JR, Douglas P, Hickey WF et al. Experimental congestive heart failure produced by rapid ventricular pacing in the dog: cardiac effects. Circulation 75(4), 857–867 (1987).
- Shannon RP, Komamura K, Stambler BS, Bigaud M, Manders WT, Vatner SF. Alterations in myocardial contractility in conscious dogs with dilated cardiomyopathy. Am. J. Phys. 260(6 Pt 2), H1903–H1911 (1991).
- Huizar JF, Kaszala K, Potfay J et al. Left ventricular systolic dysfunction induced by ventricular ectopy: a novel model for premature ventricular contraction-induced cardiomyopathy. Circ. Arrhythm Electrophysiol. 4(4), 543–549 (2011).
- Baman TS, Lange DC, Ilg KJ et al. Relationship between burden of premature ventricular complexes and left ventricular function. Heart Rhythm 7(7), 865–869 (2010).
- Niwano S, Wakisaka Y, Niwano H et al. Prognostic significance of frequent premature ventricular contractions originating from the ventricular outflow tract in patients with normal left ventricular function. Heart 95(15), 1230–1237 (2009).
- Ban JE, Park HC, Park JS et al. Electrocardiographic and electrophysiological characteristics of premature ventricular complexes associated with left ventricular dysfunction in patients without structural heart disease. Europace 15(5), 735–741 (2013).
- Yokokawa M, Kim HM, Good E et al. Impact of QRS duration of frequent premature ventricular complexes on the development of cardiomyopathy. Heart Rhythm 9(9), 1460–1464 (2012).
- Bogun F, Crawford T, Reich S et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm 4(7), 863–867 (2007).
- Del Carpio Munoz F, Syed FF, Noheria A et al. Characteristics of premature ventricular complexes as correlates of reduced left ventricular systolic function: study of the burden, duration, coupling interval, morphology and site of origin of PVCs. J. Cardiovasc. Electrophysiol. 22(7), 791–798 (2011).
- Yokokawa M, Kim HM, Good E et al. Relation of symptoms and symptom duration to premature ventricular complex-induced cardiomyopathy. Heart Rhythm 9(1), 92–95 (2012).
- Deyell MW, Park KM, Han Y et al. Predictors of recovery of left ventricular dysfunction after ablation of frequent ventricular premature depolarizations. Heart Rhythm 9(9), 1465–1472 (2012).
- Carballeira Pol L, Deyell MW, Frankel DS et al. Ventricular premature depolarization QRS duration as a new marker of risk for the development of ventricular premature depolarization-induced cardiomyopathy. Heart Rhythm 11(2), 299–306 (2014).
- Yokokawa M, Good E, Crawford T et al. Recovery from left ventricular dysfunction after ablation of frequent premature ventricular complexes. Heart Rhythm 10(2), 172–175 (2013).
- Campos B, Jauregui ME, Park KM et al. New unipolar electrogram criteria to identify irreversibility of nonischemic left ventricular cardiomyopathy. J. Am. Coll. Cardiol. 60(21), 2194–2204 (2012).
- Ling Z, Liu Z, Su L et al. Radiofrequency ablation versus antiarrhythmic medication for treatment of PVCs from the right ventricular outflow tract: prospective randomized study. Circ. Arrhythm Electrophysiol. 7(2), 237–243 (2014).
- Huang CX, Liang JJ, Yang B et al. Quality of life and cost for patients with premature ventricular contractions by radiofrequency catheter ablation. Pacing Clin. Electrophysiol. 29(4), 343–350 (2006).
- Penela D, Van Huls Van Taxis C, Aguinaga L et al. Neurohormonal, structural, and functional recovery pattern after premature ventricular complex ablation is independent of structural heart disease status in patients with depressed left ventricular ejection fraction: a prospective multicenter study. J. Am. Coll. Cardiol. 62(13), 1195–2202 (2013).
- Hayes DL, Boehmer JP, Day JD et al. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm 8(9), 1469–1475 (2011).
- Lakkireddy D, Di Biase L, Ryschon K et al. Radiofrequency ablation of premature ventricular ectopy improves the efficacy of cardiac resynchronization therapy in nonresponders. J. Am. Coll. Cardiol. 60(16), 1531–1539 (2012).
- Pedersen CT, Kay GN, Kalman J et al. EHRA/HRS/APHRS expert consensus on ventricular arrhythmias. Heart Rhythm 11(10), e166–e196 (2014).