Research Article - Clinical Practice (2017) Volume 14, Issue 6
Vertebral puncture reduces vertebral fracture-associated pain-do osteoplastic procedures qualify as successful placebo interventions?
- Corresponding Author:
- Kasperk C
Department of Endocrinology
Metabolism and Clinical Chemistry
University of Heidelberg, Heidelberg, Germany
E-mail: christian.kasperk@med.uniheidelberg.de
Abstract
Objective: The results of three randomized sham-controlled trials investigating the outcome after osteoplastic procedures demonstrated contradictory results and are flawed by using local anaesthesia as a sham procedure in the placebo- as well as in the osteoplasty cohort. This raises the need for a true sham procedure that eliminates the effect of local anaesthetics in pain relief. Methods: To establish the safety of such a procedure, we performed a study with 14 patients suffering from painful osteoporotic vertebral fractures. These patients underwent sole vertebral puncture with a Jamshidi needle in general anaesthesia. Results: The mean postoperative VAS value decreased from 5.84 ± 2.21 standard deviation (sd) to 3.55 ± 2.53 the next day, 3.25 ± 1.92 after 2 weeks, 3.55 ± 2.25 after 1 month and 2.89 ± 1.71 after 3 months. The observed effects were within the range of published pertinent osteoplasty trials (intervention groups). Conclusions: A “placebo” procedure like vertebral puncture is urgently needed to clarify the impact of non-surgical factors like total muscle relaxation in a prone position and placebo-related effects in osteoplasty.
Keywords
kyphoplasty, vertebroplasty, osteoplasty, sham, back pain, relaxation, placebo
Introduction
Osteoplastic procedures like kyphoplasty and vertebroplasty aim to improve quality of life by alleviating vertebral fracture-associated pain and immobility. Numerous randomized and non-randomized controlled trials compared the outcome “pain reduction” and “quality of life” after osteoplastic interventions with the outcome after conservative treatment [1-5]. These trials report on a significantly quicker, stronger and longer lasting pain-reduction and thus improved quality of life after osteoplastic interventions. However, these trials do not adequately reveal the role of the surgical and psychosocial impact on the post-operative pain perception. Furthermore, the mechanism how osteoplastic procedures accomplish pain reduction in osteoporotic vertebral fracture patients remains unclear because
(a) A partial or complete restoration of initial vertebral body shape and height is rarely accomplished in kyphoplasty (or vertebroplasty) and is therefore no prerequisite for a successful pain-reducing osteoplasty. Furthermore, evidence for a correlation between the degree of vertebral height restauration by an osteoplastic procedure and the accomplished degree of pain reduction is lacking.
(b) The pain-reducing effects of osteoplastic procedures occur independently of the chemical nature of the implant; exothermically hardening plastic material (i.e. polymethylmetacrylate) as well as isothermic hardening calcium phosphate cements has the same pain-reducing effects [2].
(c) Remarkably, the local pain-reducing effects of osteoplastic procedures can be observed in fresh (= exhibiting bone edema in a recent MRI) as well as in old vertebral fractures (>1 year old) [2-6].
Two sham-controlled trials [7,8] did not observe a significant difference with regard to pain reduction and quality of life after vertebroplasty compared to controls; these trials select local anaesthesia as a sham procedure, however, they also utilize the same procedure in the vertebroplasty group. Another more recent randomized, sham-controlled trial also chose local anaesthesia as a control procedure to imitate invasive vertebroplasty; however in this double blinded RCT, vertebroplasty appeared superior for pain reduction to the placebo group although, again, both groups received local subcutaneous lidocaine injections during the procedures [9].
Local anaesthesia is a well-established treatment for painful degenerative changes of the spine [10], therefore the observed different outcomes in these blinded vertebroplasty RCTs may be due to pharmacological differences of the used local analgesics or due to differences of the infiltration technique. It is also unclear whether the usage of a balloon device to create a void within the fractured vertebra (as done in kyphoplasty) before implantation of cement material has an additional clinical benefit for the patient because a clinical trial comparing vertebroplasty and kyphoplasty did not show significant differences with regard to the outcome “pain reduction” [6].
Pain reduction by the published “sham” procedures is similar to pain reduction by vertebroplasty [7,8] and pain reduction by vertebroplasty is similar to pain reduction by kyphoplasty [6]. Thus, we wondered what would be the effect of a true sham procedure performed without local anaesthesia, without inserting cement and without inserting a balloon catheter into the painfully fractured vertebral body.
Therefore, vertebral puncture in general anaesthesia qualifies as a sham procedure without any pre- or post-operative local anaesthesia because
(a) The puncture of the fractured vertebral body is the first step in all osteoplastic procedures, and
(b) The prone positioning of the patient in total muscle relaxation may allow for an otherwise not achievable realignment of the spine.
Methodology applied
A pilot study was set up as non-controlled interventional study to evaluate the safety of a true sham procedure. This pilot study was approved by the ethics committee of the University of Heidelberg to demonstrate that a true sham procedure like vertebral puncture does not harm the patient as a prerequisite for future truly sham-controlled randomized osteoplasty trials. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Helsinki Declaration of 1975, as revised in 1983.
14 patients suffering from painful osteoporotic vertebral fractures for more than 6 months were recruited in our outpatient clinic (TABLE 1). The inclusion criteria were colocalization of pain and radiographic vertebral fractures Genant grade 3 [11], exhibiting gas accumulation within the vertebrae (“Kümmell’s disease” [12]). The indication for vertebral puncture was discussed among an interdisciplinary team of internists, radiologists and orthopaedic surgeons. Patients with radiographic signs of recent vertebral fractures, multiple myeloma, malignoma, secondary osteoporosis or severe medical conditions were excluded.
| no. pat. | 14 | ||||
| Age [years] | 68.6 (47-82) | ||||
| no. female | 13 | ||||
| treated fractures | 1 | 10 | |||
| 2 | 3 | ||||
| 3 | 1 | ||||
| mean | sd | min | max | ||
| BMD T-score | Lumbar | -1.78 | 1.26 | -3.4 | -0.1 |
| Femoral | -2.03 | 0.60 | -3.1 | -1.0 |
Table 1. Patient characteristics of our study population.
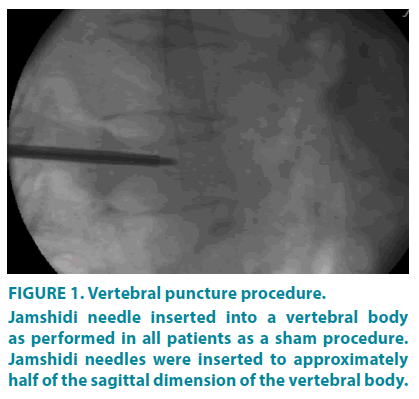
Vertebral puncture was performed in general anaesthesia under fluoroscopic control. After skin incision, a Jamshidi needle was inserted into every pedicle just exceeding half the depth of the fractured vertebral body (FIGURE 1) and was subsequently removed. No other device was inserted or any bone cement or local analgesics introduced into the vertebral body. Wounds were sutured, general anaesthesia concluded and patients transferred back to a normal ward. All patients have been on standard anti-osteoporotic medication (bisphosphonates, calcium and vitamin D). There was no change of quality or dose of any analgesic medication allowed preand post-operatively. Patients were mobilized the following day and discharge took place on the second day after the operation. Patients were evaluated by VAS [13] one day before and postop, followed-up after 2 weeks, 1 and 3 months. VAS-scores were taken at every time point, means and standard errors calculated and results compared to preoperative results.
All statistical analyses were performed using SAS system, release 9.3 (SAS Institute Inc., Cary, NC.). A test result with p ± 0.05 was considered statistically significant. In order to investigate changes over time, an ANOVA has been performed using the SAS procedure PROC MIXED. Furthermore, Dunnett’s test has been applied in order to compare the mean values at different time points with the mean value at the beginning.
Results
Vertebral puncture reduces pain of osteoporotic vertebral fractures
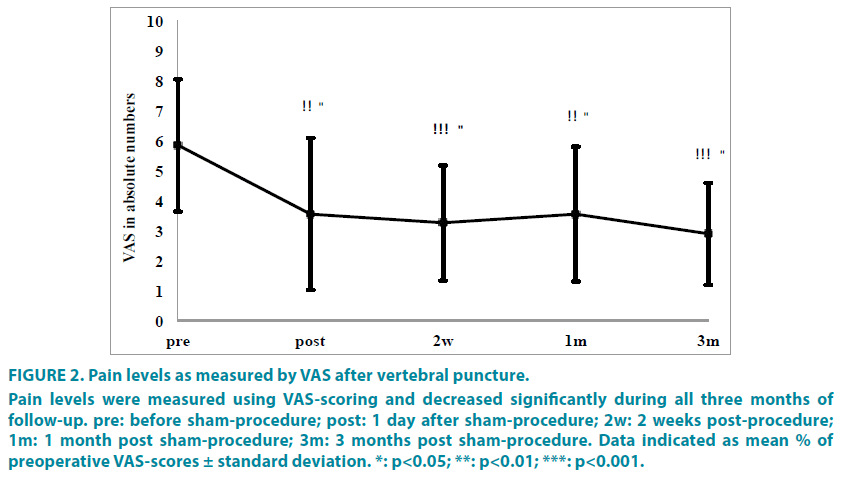
Mean preoperative absolute VAS values were 5.84 ± 2.21 standard deviation (sd) and decreased to 3.55 ± 2.53 the next day, 3.25 ± 1.92 after 2 weeks, 3.55 ± 2.25 after 1 month and 2.89 ± 1.71 after 3 months (FIGURE 2). Pain decrease was statistically significant from the day after sham-procedure onwards and displayed significance in the mixed linear model of p=0.0006.
Figure 2: Pain levels as measured by VAS after vertebral puncture.
Pain levels were measured using VAS-scoring and decreased significantly during all three months of follow-up. pre: before sham-procedure; post: 1 day after sham-procedure; 2w: 2 weeks post-procedure; 1m: 1 month post sham-procedure; 3m: 3 months post sham-procedure. Data indicated as mean % of preoperative VAS-scores ± standard deviation. *: p<0.05; **: p<0.01; ***: p<0.001.
Safety
There were no adverse events observed in any of the 14 patients treated by vertebral puncture. Adverse events were defined as local trauma, bleeding, neurological deficit, infection, thrombosis, thromboembolism, acute coronary syndrome or all-cause death.
Discussion
This study shows that vertebral puncture reduces vertebral fracture-associated pain, does not harm patients with painful osteoporotic vertebral fractures but rather improves the clinical symptoms. Therefore, vertebral puncture in general anaesthesia qualifies as a true sham procedure in future clinical osteoplasty trials investigating the additional impacts of
(a) Inserting bone cement into a fractured vertebra as done in vertebroplasty,
(b) Creation of an intravertebral void by a balloon catheter and stabilization of the fractured vertebra by application of bone cement into the preformed cavity as done in kyphoplasty.
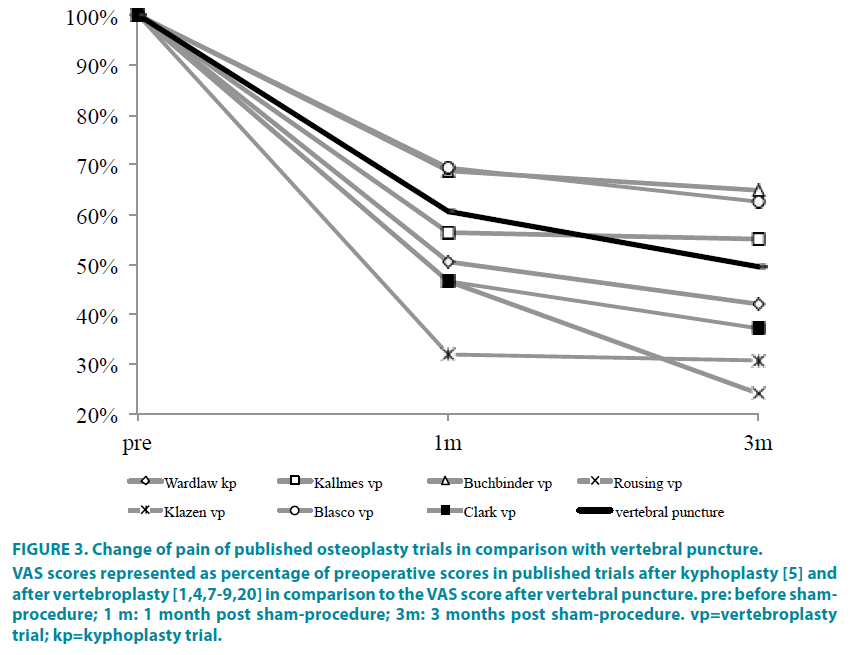
Due to the amazing improvement of vertebral fracture-associated pain after vertebral puncture, the reported improvements of preoperative pain levels in the published RCTs investigating vertebroplasty and kyphoplasty were plotted together with the VAS changes of the cohort of this pilot study as shown in FIGURE 3.
Figure 3: Change of pain of published osteoplasty trials in comparison with vertebral puncture.
VAS scores represented as percentage of preoperative scores in published trials after kyphoplasty [5] and after vertebroplasty [1,4,7-9,20] in comparison to the VAS score after vertebral puncture. pre: before shamprocedure; 1 m: 1 month post sham-procedure; 3m: 3 months post sham-procedure. vp=vertebroplasty trial; kp=kyphoplasty trial.
Vertebral puncture is causing a similar pain relief as osteoplastic procedures at least for the first three months as demonstrated in vertebroplasty and kyphoplasty randomized controlled trials (RCTs, FIGURE 3). The mechanism whereby vertebral puncture may reduce vertebral fracture pain remains elusive.
It has been reported that in the natural course of a vertebral fracture, pain subsides (VAS ≤ 3) by itself in approximately 50% of patients [14]. This observation does not apply to our observations after vertebral puncture because all patients had old vertebral fractures and were treated with pain medication for >6 months. In vertebral puncture, the perioperative management including the impact of complete muscle relaxation during general anaesthesia, the prone positioning of the patient, the intensive perioperative care for an in-patient with severe pain, in addition to the puncture itself may all contribute to the postoperative improvement of pain. An additional factor might be a placebo effect [15].
It is well known that surgical trials dealing with pain and quality of life are prone to bias due to the “surgical impact” if not controlled against true sham controls [16-18]. To understand the impact and mechanism of action of pain-reducing procedures such as osteoplastic interventions, it is inevitable to consider the placebo effect because the basis of placebo analgesia was demonstrated to be a powerful effect of a central opioidergic mechanism [15,19]. In a recent editorial, Miller et al. [18,20] even suggest that vertebroplasty itself may actually be an effective placebo procedure. However, this conclusion appears premature because the outcomes of the available sham-controlled trials investigating vertebroplasty [7-9] in conscious sedation are flawed by the utilization of local anaesthesia as a sham procedure. By note, local anaesthetics are widely used in daily orthopaedic routine for the treatment of back pain, but the differentiation of the exact disease entity of pain remains elusive [10].
There are several limitations to this pilot study. First, only a very small number of patients were selected by an interdisciplinary team who agreed on the inclusion of patients with severely fractured vertebral bodies, because osteoplastic procedures in these cases appeared too risky with regards to cement leakage or balloon catheter displacement. Therefore, the selection of painfully fractured vertebral bodies in this work does not really represent a typical osteoporotic vertebral compression fracture. We also followed-up on the patient cohort for only three months. Finally, all treated severely fractured vertebrae were older than 6 months, again not representing the typical situation of a patient with osteoporosis and painfully fractured vertebral bodies. However, vertebral puncture reduces pain in severely fractured osteoporotic vertebral bodies exhibiting Kümmels’ disease for at least 3 months, does not harm the patient, and thus qualifies as a sham procedure for future randomized sham-controlled trials investigating clinical outcomes after osteoplastic interventions.
We suggest that the effects of vertebro- and kyphoplasty should be tested against vertebral puncture in general anaesthesia to allow for more objective conclusions on the impact of osteoplastic interventions on such multifactorial parameters as pain relief and quality of life.
Funding source
This work was supported by the Havemann Family, Berlin, Germany and by the Hopp Foundation, St. Leon-Rot, Germany.
Conflict of interest
None of the authors has conflicts of interest to disclose.
Acknowledgments
No acknowledgements to be made.
References
- Blasco J, Martinez-Ferrer A, Macho J, et al. Effect of vertebroplasty on pain relief, quality of life, and the incidence of new vertebral fractures: a 12-month randomized follow-up, controlled trial. J. Bone Miner. Res. 27(5), 1159-1166 (2012).
- Kasperk C, Hillmeier J, Nöldge G, et al. Treatment of painful vertebral fractures by kyphoplasty in patients with primary osteoporosis: a prospective nonrandomized controlled study. J. Bone Miner. Res. 20(4), 604-612 (2005).
- Kasperk C, Grafe IA, Schmitt S, et al. Three-year outcomes after kyphoplasty in patients with osteoporosis with painful vertebral fractures. J. Vasc. Interv.Radiol.21,701-709 (2010).
- Klazen CA, Lohle PN, deVries, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet.376(9746),1085-1092 (2010).
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet.373(9668), 1016-1024 (2009).
- Liu JT, Liao WJ, Tan WC, et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos.Int. 21(2), 359-364 (2010).
- Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures.N. Engl. J. Med. 361, 557-568 (2009).
- Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures.N. Engl. J. Med. 361, 569-579 (2009).
- Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet.388(10052),1408-1416 (2016).
- Falco FJ, Manchikanti L, Datta S, et al.An update of the effectiveness of therapeutic lumbar facet joint interventions.Pain Physician.15(6), E909-953 (2012).
- Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique.J. Bone Miner. Res. 8(9), 1137-1148 (1993).
- Li H, Liang CZ, Chen QX.Kümmell's disease, an uncommon and complicated spinal disorder: a review. J. Int. Med. Res. 40(2), 406-414 (2012).
- Boonstra AM, SchiphorstPreuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 31(2),165-169 (2008).
- Venmans A, Klazen CA, Lohle PN, et al. Natural history of pain in patients with conservatively treated osteoporotic vertebral compression fractures: results from VERTOS II. AJNRAm. J. Neuroradiol.33(3), 519-521 (2012).
- Tracey I. Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nat. Med. 16, 1277-1283 (2010).
- Johnson. Surgery as a placebo.Lancet.344(8930),1140-1142 (1994).
- McCulloch P, Altman DG, Campbell WB, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet.374(9695),1105-1112 (2009).
- Miller FG. The enduring legacy of sham-controlled trials of internal mammary artery ligation.Prog.Cardiovasc.Dis. 55(3), 246-250 (2012).
- Benedetti F, Mayberg HS, Wager TD, et al. Neurobiological mechanisms of the placebo effect. J. Neurosci.25(45), 10390-10402 (2005).
- Rousing R, Andersen MO, Jespersen SM, et al. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine.34(13), 1349-1354 (2009).