Case Report - Neuropsychiatry (2018) Volume 8, Issue 5
Visual Therapy in Open Space Rehabilitation of Acquired Visual Field Defect
- Corresponding Author:
- Anna Przekoracka-Krawczyk
Laboratory of Vision Science and Optometry, Faculty of Physics, Adam Mickiewicz University, Umultowska 85, 61-614, Poznań, Poland
Fax: +48 61 829 5155
Abstract
Purpose
Visual field defect (VFD) is one of the most common impairments that can occur after the brain damage. Different approaches: optical aids, compensatory training and restorative training were extensively evaluated, however each of these therapies still leave much to be desired, since they did not always accomplish the expected result. The aim of the presented case is to demonstrate that optometric vision therapy (OVT) in open space, commonly used in patients with binocular vision disorders, may be an alternative and efficient treatment of VFD, since it focuses on the integration of sensory and motor functions with the strong engagement of visual attention.
Case Report
This report describes the case of young patient diagnosed with a bilateral tunnel vision defect and central sparing. This was caused by a cyst in the occipital area. OVT was implemented to improve the visual field, accommodation and vergence skills. After 8 months of the therapy (25 in-office sessions with home enhancement) all visual parameters and visual field were in normal range.
Conclusions
OVT appears to be a promising rehabilitation method especially in young patients with acquired brain injury. Further investigation however, of the effect of OVT on the visual field enlargement is needed.
Keywords
Visual field defect, Optometric vision therapy, Restoration training
Introduction
Acquired brain injury (ABI), beyond the physical, cognitive and/or psychological impairments, strongly affects visual functions. Commonly reported difficulties comprise: accommodative disorders, resulting in blurred vision; binocular disorders of double vision that derive from a noncomitant deviation; reading difficulties related to eye movement disorders; comprehension and/ or attention difficulties and visual field defects (VFD) [1]. The studies of Suchoff et al. [2] and Rowe et al. [3] agree, that almost 50% of patients with ABI were diagnosed with VFD. Moreover, VFD is the one of the most common visual deficits in ABI [4].
Two rehabilitation strategies for VFD can be classified as either active or passive ones. The former aims at restoration some part of visual field, and the latter is directed to compensate the loss, by teaching more effective ways of using the remainder of the visual fields or through expansion of visual field by prisms [4,5].
One passive treatment – compensatory training, attempts to effectively manage the remaining visual field, thus adapting to the visual field loss. This training applies scanning strategies (large eye movements) and target-localization tasks to facilitate visual exploration in daily life [4,5]. After treatment both visual search field expansion and a reduction of time needed for searching objects were reported [6].
Another approach – restorative training aimed at restoration of visual field loss. Recent review distinguished between two different methods aimed to restore visual field: (i) a borderfield training which focuses on exercises at the edge between intact and blind area, and (ii) a blindsight training based on the tasks performed within damaged visual field [7]. Interestingly, Matteo et al. [7] suggested that both techniques bring different benefits, since the former improves visual signal detection, whereas the latter enhances their processing. However, it is observed that the influence of the implemented rehabilitation on visual field border often differs considerably between patients [8]. For example, the recent study by Poggel et al. [8] presented a patient whose visual field remained unchanged after the border training, the other patient, in turn, had almost full recovery of visual field after the treatment. Moreover, computer training, used in border rehabilitation and based on having patients practise perimetry at home using a special software (Vision Restoration Therapy (VRT) by NOVAVISION), was widely discussed, since first studies reported its positive effect on the visual field in hemianopic patients, [9] whereas another research did not confirm these results. This latter study showed little or no significant effect on visual field expansion [10] interestingly, the combination of VRT with transcranial direct current stimulation (tDCS) resulted in the enlargement of visual field compared with border training alone. However, this shift of visual border was still not greater than 5˚ [11].
The alternative way for treating VFD in active way may be an optometric vision therapy (OVT) in open space. This therapy was used primarily for improvement of visual functions in amblyopia, strabismus, oculomotor deficits, and accommodative, or vergence disorders [12]. This approach can also be applied in the case of ABI patients [13,14]. The consideration of techniques which strongly engage visual attention, that improves visual-spatial awareness into OVT sessions, seems to be effective in rehabilitation of VFD.
This case reports the effectiveness of OVT in open space in rehabilitation of VFD in a case of young ABI patient.
Case Report
Patient was 12 years old Caucasian female (A.P.) with a history (18 months) of physical activitytriggered headaches, vertigo and visual field loss. Neuroimaging (CT, MR) revealed 4.5 × 4 × 3 cm cyst in the occipital area of both left and right hemispheres, which was shifted more to the left. Based on the ophthalmological examination and neuroimaging optic nerve (II) and visual pathway were intact. Patient was qualified to surgical procedure.
During the neurological examination prior to neurosurgical intervention, the patient presented concentric visual field loss, expressed more temporal and impaired visual acuity (20/33 right eye (OD) and 20/40 left eye (OS)) at distance. Total resection procedure was performed, without complications, using ipsilateral access. Post-procedure MRI revealed linear scar (approx. 3 mm thick) extending from peripheral region of parietal lobe to the occipital horn of lateral ventricle.
Thirty days after surgery visual acuity was still reduced (20/100 OD and 20/67 OS). The visual field was limited to the central part, resulted in reading problems and difficulties with activities of daily living. Slit lamp examination of anterior and posterior segments of the eyes did not reveal any abnormalities. The cycloplegic refraction was OD plano cyl – 0.50 ax 106˚ and OS sph +0.50 cyl – 0.50 ax 82˚. Six months after surgical procedure, no spontaneous recovery of VFD was noted, therefore the patient was referred to Adam Mickiewicz University and University of Medical Sciences in Poznan for further consultation.
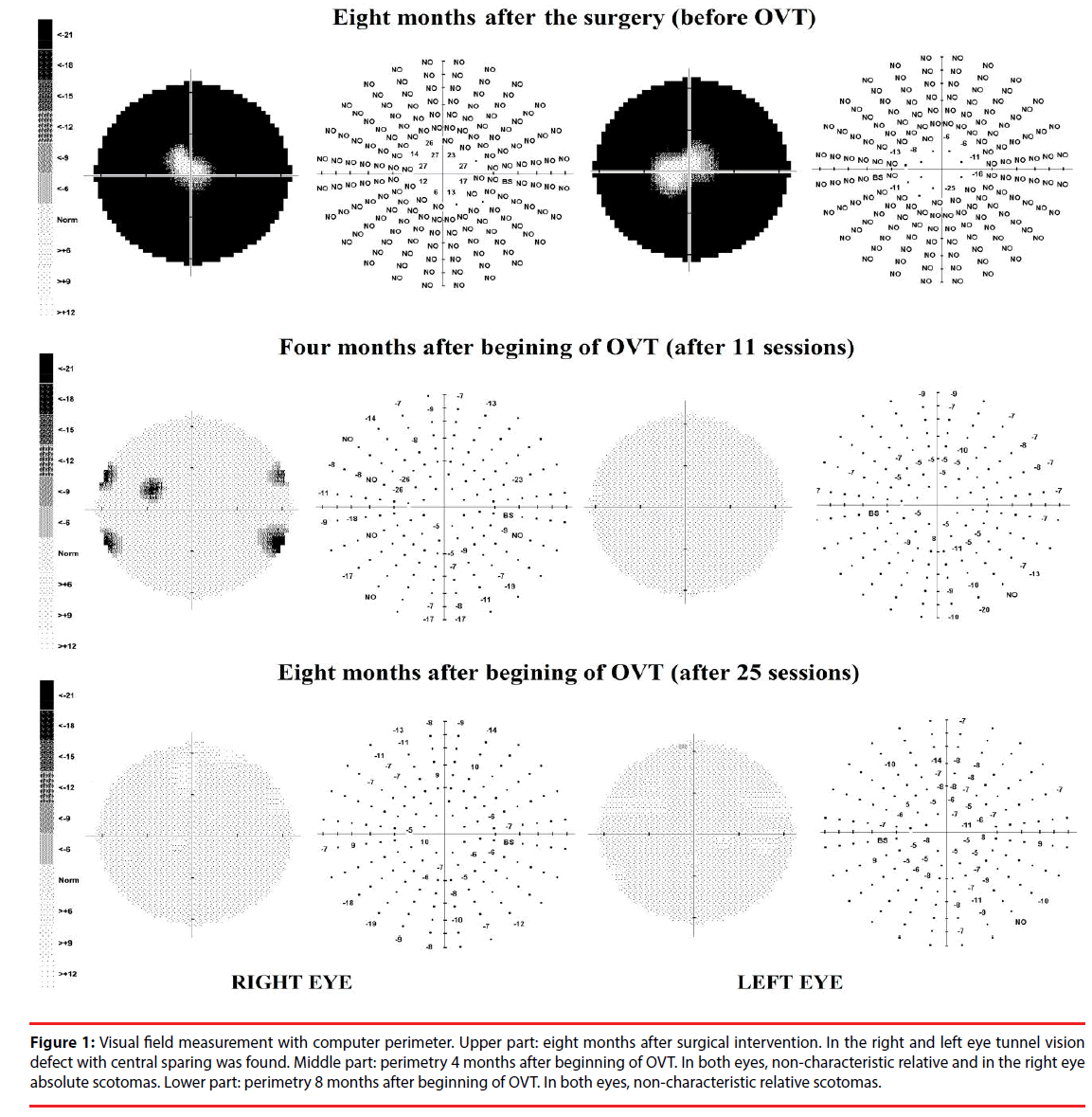
Eight months after surgical intervention, the eye examinations indicated bilateral tunnel vision defect with central sparing (Figure 1). Visual acuity was reduced (20/40 OD and 20/23 OS). Refraction showed the small amount of with-the-rule astigmatism, but spectacle correction did not improve the visual acuity. Pupils were round, significantly dilated (about 8 mm in diameter) and reactive to light and accommodation. Heterophoria measured by cover test, was 1 Δ base in at distance and 7 Δ base in at near. Vergence ranges were within reference ranges (according to Morgan’s expecteds) [15] although a full range of eye movements was observed, smooth pursuits were characterized by many refixations and saccades were characterized by undershooting. Near point of convergence (NPC) was remote (break 15.5 cm/recovery 19,5 cm) and +/-2,00 D accommodative facility (10 cpm OD, 9 cpm OS, 5 cpm OU) and amplitude of accommodation (7.5 D OD; 8.5 D OS) were reduced. Subjectively, the patient reported blurred and frequent double vision at near, especially during reading. To quantify the patient’s symptoms, a specific vision-targeted Symptoms Checklist - brain injury vision symptom survey (BIVSS) was used, that allowed for the comparison of the subjective indices preand post-therapy [16]. On the first examination A.P. obtained 68 points indicating main problems with eyesight clarity (double and blurred vision); visual comfort (eyestrain, headaches or dizziness after using her eyes, eye fatigue); light sensitivity as well as depth perception (lack of confidence walking, missing steps, clumsiness).
Figure 1: Visual field measurement with computer perimeter. Upper part: eight months after surgical intervention. In the right and left eye tunnel vision defect with central sparing was found. Middle part: perimetry 4 months after beginning of OVT. In both eyes, non-characteristic relative and in the right eye absolute scotomas. Lower part: perimetry 8 months after beginning of OVT. In both eyes, non-characteristic relative scotomas.
OVT was recommended consisting of weekly 60 min in-office sessions, with 5 times per week home reinforcement (30-40 min). Emphasis was placed on the improvement of the following parameters: amplitude of accommodation (with Accommodative Push-Ups); accommodative facility (with flippers, Hart Chart Accommodative Rock); pursuit eye movements (with Marsden ball, rotating pegboard, pencils); saccades (with Hart Chart, pencils, Shur Mark); near point of convergence (with a pencil pushup, Brock string); eye-hand coordination (with Marsden ball, rotating pegboard and Russel Ring); visuospatial awareness (with Marsden ball, peripheral awareness chart, figure and star drawing on the whiteboard, saccade and card scanning, scarf juggling and Press Lite procedures). The therapy procedures are described in detail elsewhere [1,17-20].
After 16 weeks of treatment (11 in-office sessions) the improvement of visual parameters was noticed. Patient subjectively noted that the visual field seemed wider and she improved in daily activities. Figure 1 (middle part) shows the perimetric results for both eyes. Visual acuity without correction was similar (20/33 OD and OS), however significant improvement with spectacle correction (OD plano cyl - 0.25 ax 105˚, OS plano cyl - 0.50 ax 80˚) was observed (20/17 OD and OS). Therefore, spectacles were prescribed. Ocular motility was much better, as well as accommodative facility (14.5 cpm OD, 15 cpm OS, 12 cpm OU). NPC was still slightly remote (break: 10.5 cm/recovery 17.5 cm).
Patient reported occasionally blurred and double vision, especially during prolonged reading. An additional 4 months of OVT was implemented that focused on fusional vergence ranges and NPC (with tranaglyphs, vectograms, Brock string, prism flippers, Eccentric Circles, Lifesaver cards, Aperture Rule). She also continued techniques aimed at improving her visuospatial awareness.
These previously weakened parameters were improved. The patient’s visual acuity was above the norm (20/17 OD and OS, 20/13 OU); she was able to converge the eyes to the nose; amplitude of accommodation was high (18 D OD and OS) and accommodative facility was better than norms (18 pcm OD, 20 pcm OS, 15 pcm OU). Alternate cover test revealed small exophoria within a normal range (1 Δ at distance and 3Δ at near). Visual symptoms were reduced, as reflected in the results of the BIVSS (11 points). Significant objective improvement of the visual field was found in perimetry results (Figure 1).
The next follow-up appointment, (4 months) revealed all visual parameters were acceptable and there was a small change in a distance spectacle prescription. One-year follow-up examination indicated proper visual functions with full visual field and contact lenses were applied.
Discussion
In the presented case study, the patient was diagnosed with decreased central (visual acuity) and peripheral visual field loss. We may suspect that visual cortex located in area of calcarine sulcus, which is strongly related to central vision, was only partially affected by the cyst, but the pressure in the more lateral areas of visual cortex could resulted in the peripheral visual field loss. Ocular and visual pathway was intact, what strongly suggest that visual deficits must arise from the brain structure damage. Visual functions improved significantly as a result of the implemented approach.
Studies have shown that some patients with VFD experienced spontaneous improvement or even a full recovery. This restoration data is however ambiguous, ranging from 7% to 85% of patients [21]. Clinicians have claimed that about 50% of VFD patients had no visual field recovery [3]. In most cases, a recovery usually appears within the first 3 months from the injury and further improvements are negligible [3,5]. In this case, almost no spontaneous improvement was found after eight months from the surgical procedure, therefore further spontaneous recovery was not expected.
As mentioned above, passive approaches to the treatment of a VFD revealed no significant effect on the restoration of the visual field and two methods of restoration training, a borderfield training and a blindside training, brought different results. Moreover, these methods very rarely resulted in a complete recovery of visual field. Matteo et al. [7] suggested that combining both border and blindsight rehabilitation may be successful.
In turn, OVT appears to be promising treatment of VFD, since significant enlargement of visual field was demonstrated in this case. The success can result from the combination of eyehand coordination tasks and the involvement of the attention into peripheral vision that may stimulate the visual cortex more than other procedures, leading to these significant improvements. Furthermore, the techniques used in this approach are based on exercising both border and blindsight visual field.
Although all restorative treatments are based on the concept of neuroplasticity of visual system which allow for the restoration of the lost visual functions, the presented intensive visuo-motor rehabilitation, coupling integration of the sensory and motor systems may have resulted in enhancing potential brain plasticity. Even though the study showed that visual cortex has the capacity to reorganize after damage to the brain even in adults, [22] it seems that the plasticity is more powerful and efficient during early life [23]. Moreover, the success of the rehabilitation may depend on the time span between brain injury and the commencement of the therapy.
Based on presented case of the patient diagnosed with bilateral visual field defects, we demonstrated high effectiveness of OVT in the treatment of visual field loss. We suspect that procedures used in OVT [24,25] may more efficiently stimulate the visual cortex and process of vision. Nevertheless, further studies investigating the effectiveness of OVT on other types of VFDs in children and adults are needed.
Acknowledgements
The authors thank Małgorzata Banaszak for technical support during the therapy.
Conflicts of Interest
The authors confirm that this article content has no conflicts of interest.
References
- Scheiman M, Wick B. Clinical Management of Binocular Vision:Heterophoric: Accommodative and Eye Movement Disorders. 3rd Edtn. Philadelphia, PA: Lippincott Williams & Wilkins (2008).
- Suchoff IB, Kapoor N, Ciuffreda KJ, et al. The frequency of occurrence, types, and characteristics of visual field defects in acquired brain injury: a retrospective analysis. Optometry 79(5), 259-265 (2008).
- Rowe FJ, Wright D, Brand D, et al. A prospective profile of visual field loss following stroke: prevalence, type, rehabilitation, and outcome. BioMed. Res. Int 2013(1), 719096 (2013).
- Pambakian A, Currie J, Kennard C. Rehabilitation strategies for patients with homonymous visual field defects. J. Neuroophthalmol 25(2), 136-142 (2005).
- Lane AR, Smith D, Schenk T. Clinical treatment options for patients with homonymous visual field defects. Clin. Ophthalmol 2(1), 93-102 (2008).
- Kerkhoff G, Münssinger U, Meier EK. Neurovisual rehabilitation in cerebral blindness. Arch. Neurol 51(5), 474-481 (1994).
- Matteo BM, Viganò B, Cerri CG, et al. Visual field restorative rehabilitation after brain injury. J. Vis 16(9), 1-18 (2016).
- Poggel DA,Treutwein B, Sabel BA, et al. A matter of time: improvement of visual temporal processing during training-induced restoration of light detection performance. Front. Psychol 6(1), 22 (2015).
- Kasten E, Wüst S, Behrens-Baumann W, et al. Computer-based training for the treatment of partial blindness. Nat. Med 4(9), 1083-1087 (1998).
- Schreiber A, Vonthein R, Reinhard J, et al. Effect of visual restitution training on absolute homonymous scotomas. Neurology 67(1), 143-145 (2006).
- Plow EB, Obretenova SN, Jackson ML, et al. Temporal profile of functional visual rehabilitative outcomes modulated by transcranial direct current stimulation. Neuromodulation 15(4), 367-373 (2012).
- Nawrot P, Michalak KP, Przekoracka-Krawczyk A. Does home-based vision therapy affect symptoms in young adults with convergence insufficiency? Optica. Applicata 43(1), 551-566 (2013).
- Han MHE. The Role of the Neuro-Rehabilitation Optometrist: Acquired Brain Injury: An Integrative Neuro-Rehabilitation Approach. Springer New York (2007).
- Thiagarajan P, Ciuffreda KJ, Capo-Aponte JE, et al. Oculomotor neurorehabilitation for reading in mild traumatic brain injury (mTBI): an integrative approach. NeuroRehabilitation 34(1), 129-146 (2014).
- Morgan MW. Analysis of clinical data. Am. J. Optom. Arch. Acad. Optom 21(1), 477-491 (1944).
- Laukkanen H, Scheiman M, Hayes JR. Brain Injury Vision Symptom Survey (BIVSS) Questionnaire. Optom. Vis. Sci 94(1), 43-50 (2017).
- Griffin JR, Grisham JD. Binocular anomalies: Diagnosis and Vision Therapy. 4th Edtn. Boston, MA: Butterworth-Heinemann (2002).
- Lane KA. Developing Ocular Motor and Visual Perceptual Skills: An Activity Workbook: Thorofare NJ: SLACK Incorporated (2005).
- Press LJ. Press Lites – procedures for visual field awareness. Optomet. Visual Perfor 1(2), 62-67 (2013).
- Love K. Visual-Spatial Therapeutic Rehabilitation for the Brain Injured Patient. Optomet. Visual Perfor 2(3),112-117 (2014).
- Kasten E, Poggel EA, Müller-Oehring E, et al. Restoration of vision II: Residual functions and training-induced visual field enlargement in brain-damaged patients. Restor. Neurol. Neurosci 15(2-3), 273-287 (1999).
- Brodtmann A, Puce A, Darby D, et al. Extrastriate visual cortex reorganizes despite sequential bilateral occipital stroke: implications for vision recovery. Front. Hum. Neurosci 9(1), 224 (2015).
- Guzetta A, D'Acunto G, Rose S, et al. Plasticity of the visual system after early brain damage. Dev. Med. Child. Neurol 52(10), 891-900 (2010).
- Peachey GT, Peachey PM. Optometric Vision Therapy for Visual Deficits and Dysfunctions: A Suggested Model for Evidence-Based Practice. Vision. Deve. Rehab 1(4), 289-238 (2015).
- Przekoracka-Krawczyk A, Wojtczak-Kwaśniewska M. The efficiency of optometric vision therapy in accommodative esotropia with high AC/A ratio. J. Ophthatherapy 3(1), (2018).