Mini Review - Interventional Cardiology (2022) Volume 14, Issue 4
VPExam and virtual care: Exploring the frontiers of novel digital tools
- Corresponding Author:
- James V. Cireddu
Department of Cardiology,
University Hospitals Harrington Heart and Vascular,
Cleveland,
Ohio,
USA,
E-mail: James.Cireddu@UHHospitals.org
Received date: 21-Jun-2022, Manuscript No. FMIC-22-67156; Editor assigned: 23-Jun-2022, PreQC No. FMIC-22-67156 (PQ); Reviewed date: 11-Jul-2022, QC No. FMIC-22-67156; Revised date: 18-Jul-2022, Manuscript No. FMIC-22-67156 (R); Published date: 25-Jul-2022, DOI: 10.37532/1755- 5310.2022.14(4).532
Abstract
Telehealth is a growing field of importance, but the loss of comprehensive physical exam data creates barriers to managing complex heart failure patients. Innovative digital tools such as VPExam Virtual Care combine augmented reality guidance of video acquisitions with Bluetooth stethoscopes and single lead ECG to improve diagnostic accuracy by assessing volume status, cardiopulmonary auscultation, detection of arrythmias, and providing structured data including vitals, medication reconciliation, and labs. VPExam intervention has been shown to significantly improve the outcomes of high-risk heart failure patients discharged to Skilled Nursing Facilities and Home Care. VPExam QI revealed timely reliable cardiology consultation for follow up of heart failure hospitalization and urgent consultations created moderate significance modification in clinical management in 84% of encounters, while being associated with a 40% relative risk reduction in 30-day hospital readmission rate and a 56% relative risk reduction in 30-day mortality rate. This review summarizes challenges to cardiac transitions of care as well as the evolution of cardiac virtual care with actionable physical exam data to reduce readmissions and mortality.
Keywords
Telemedicine • Quality improvement • Remote patient monitoring • Transition of care • Physical exam
Introduction
Heart Failure (HF) is a leading cause of morbidity and mortality in 5.7 million Americans with management costs predicted to reach 70 billion dollars by 2030 [1]. Skilled Nursing Facilities (SNFs) care for older patients with significant comorbidities [2]. Morbidity and mortality rates are high for hospitalized heart failure patients discharged to SNFs with 30-day readmission rates between 27% to 43% due to errors in transitions, inadequate discharge planning, and lack of appropriate follow-up with health care providers [3]. Optimizing HF management in SNF populations is a growing focus of value-based care.
Numerous meta-analyses have demonstrated that compared to conventional care, the addition of telemedicine in heart failure management leads to reduced hospitalization and mortality [4,5]. Traditional telemedicine platforms present obstacles including affordability of equipment, difficult to use technology requiring extensive training, lack of standardization, and patient privacy issues. These barriers are especially challenging to SNF and Home Care populations with significant comorbidities, functional impairments, and barriers to transportation [6].
Telemedicine can offer these populations improved access, but this is typically at the expense of clinical data such as a comprehensive physical examination. Many of the most common and expensive cardio-pulmonary diseases rely on physical examination for detection of decompensation or exacerbation. Lack of physical exam data can result in loss of early detection of clinical decompensation, reduced clinical confidence, and increased risk of misdiagnosis.
Literature Review
Virtual Physical Examination (VPExam) overview
VPExam is a Health Insurance Portability and Accountability Act (HIPAA) compliant medical device data system that overcomes barriers to traditional telemedicine utilizing a combination of Augmented Reality (AR) based guidance leading a minimally trained technician (including but not limited to nurses or medical assistants) through appropriate camera positioning for video capture based upon anatomical landmarks. VPExam augmented reality guided overlays combined with sample videos as well as text and audio instructions teach users to obtain optimal video recordings of clinical findings such as evaluation of jugular venous distention and degree of lower extremity edema in a reproducible manner.
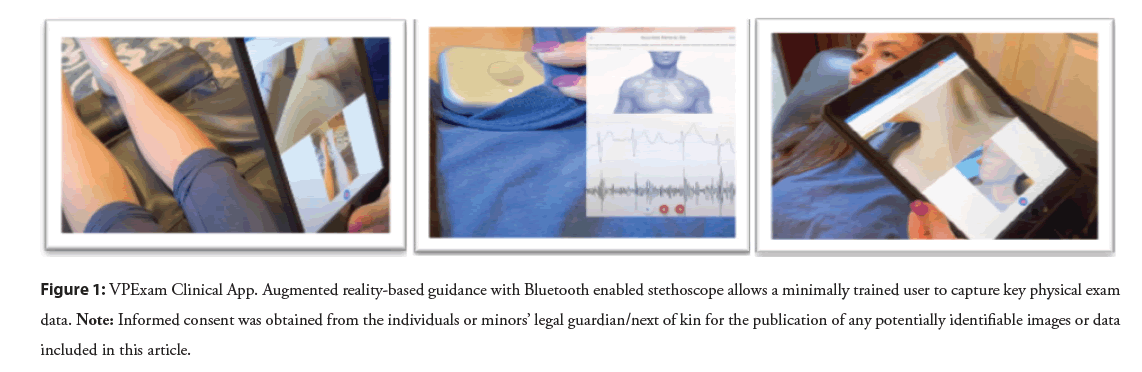
VPExam is integrated with Bluetooth enabled stethoscopes including the Eko Duo with single lead ECG to capture a full heart and lung exam with active user instruction (Figure 1). Virtual physical examination components are customizable by providers to optimize an efficient clinical workflow. The type of physical exam is customizable based on medical specialty.
Figure 1: VPExam Clinical App. Augmented reality-based guidance with Bluetooth enabled stethoscope allows a minimally trained user to capture key physical exam data. Note: Informed consent was obtained from the individuals or minors’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
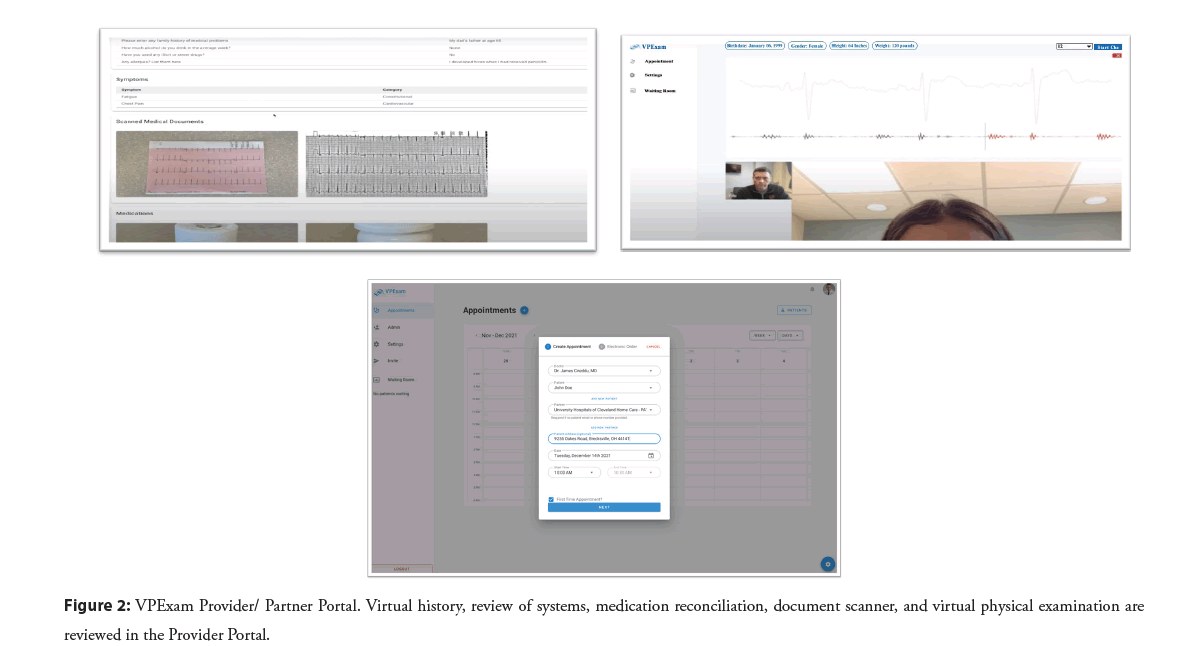
Time efficient review of asynchronous clinically relevant patient management data has proven critical for ongoing physician engagement. VPExam allows nurses to transmit structured data including manual transmission of vitals, voice recognition based virtual history and review of systems, medication reconciliation with photographs of pill bottles, and a document scanner to transmit laboratory results, orders, logs, ECGs, etc (Figure 2). Providers review VPExam Physician Portal asynchronous data prior to initiating a real time HIPAA compliant video conference with the patient. The Eko stethoscope with ECG can also be used by the provider during real time synchronous video conferencing in coordination with the nurse/Medical Assistant (MA) user with the patient (Figure 2). VPExam routinely transmits digital physical exam data for comprehensive assessment of volume status, cardiopulmonary auscultation, ECG detection of arrythmias, and structured data including vitals, medication reconciliation, and labs.
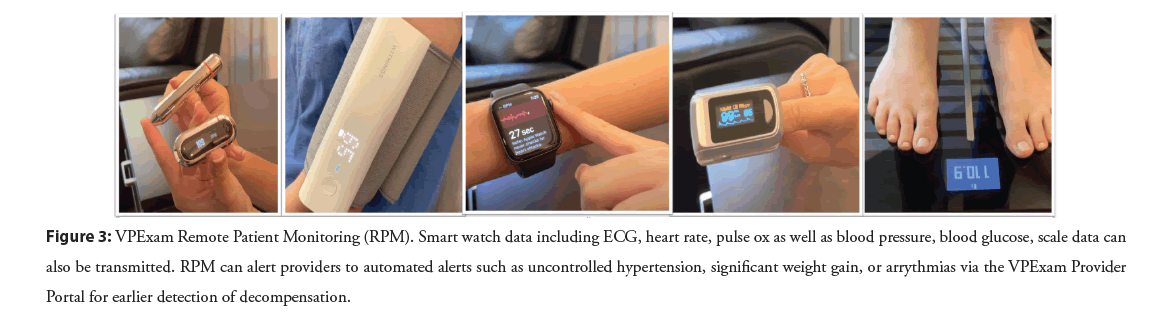
VPExam also offers additional Remote Patient Monitoring (RPM) utilizing Apple Health and Google Fit Health Kit data transmission to the VPExam Provider Portal including blood glucose, body mass index, cardio fitness, blood pressure, electrocardiogram, heart rate, oxygen saturation, walking heart rate, and weight (Figure 3). VPExam RPM allows for transmitting alerts such as tachycardia with arrythmia from a smart watch revealing a patient going into atrial fibrillation or greater than three-pound weight gain from a Bluetooth scale revealing a patient suffering from decompensation of heart failure. Abnormal RPM data can trigger deployment of personnel to perform VPExam in patients’ home or facility for earlier physician intervention.
Figure 3: VPExam Remote Patient Monitoring (RPM). Smart watch data including ECG, heart rate, pulse ox as well as blood pressure, blood glucose, scale data can also be transmitted. RPM can alert providers to automated alerts such as uncontrolled hypertension, significant weight gain, or arrythmias via the VPExam Provider Portal for earlier detection of decompensation.
Takeaways from VPExam QI
VPExam Virtual Care for Heart Failure Optimizing Transitions of Care Quality Improvement Project (VPExam QI) was designed as a single-arm prospective comparative community case study recruiting patients admitted for heart failure with anticipated discharge to SNFs or Home Care [7]. Nursing satisfaction was 4.8/5 (± 0.22). 0% technical errors were detected across partners at three SNFs and deployment on over 550 Home Care devices.
VPExam QI patients received clinical follow up for approximately 2-3 weeks duration and data collection for 3 months following VPExam encounter. There were no patients who declined participation and there were no dropouts. 19% of study encounters occurred with Home Care services and 81% of encounters occurred at Skilled Nursing Facilities. During the 6-month pilot, 33.8% of all hospitalized heart failure patients at University Hospitals of Cleveland Regional Hospitals were enrolled into VPExam QI with cardiology management based on guideline directed therapy.
84% of patient encounters required moderate significance changes in clinical modification based upon VPExam followup. The most common changes involved diuretic adjustments in 44% of encounters and vasoactive medication adjustments in 44% of encounters. Less frequent moderate significance clinical modifications included identification of medication reconciliation errors in 8% of encounters and alteration of antiarrhythmic medications in 4% of encounters. Moderate significance modification encounters were impacted by volume status assessment (47.6%), cardiopulmonary auscultation (33.3%), ECG detection of arrythmias/atrial fibrillation (14.2%), and structured data transmission of vitals, medication reconciliation, and lab results (95.2%).
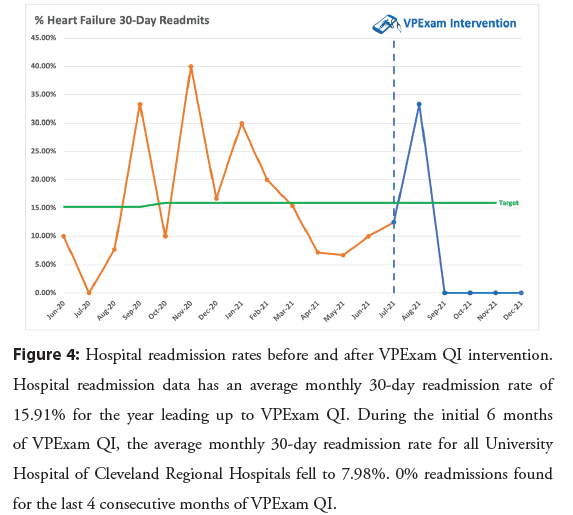
The historic control population of heart failure patients discharged from June 2020 to June 2021 had an average monthly all cause readmission rate of 15.91%. Following intervention with VPExam QI interventions, 30-day hospital readmission rates dropped to 7.98% with a 40.1% relative risk reduction. In the final four of six months of VPExam QI, readmission rates fell precipitously to 0% (Figure 4).
Figure 4: Hospital readmission rates before and after VPExam QI intervention. Hospital readmission data has an average monthly 30-day readmission rate of 15.91% for the year leading up to VPExam QI. During the initial 6 months of VPExam QI, the average monthly 30-day readmission rate for all University Hospital of Cleveland Regional Hospitals fell to 7.98%. 0% readmissions found for the last 4 consecutive months of VPExam QI.
Hospital readmission data has an average monthly 30-day readmission rate of 15.91% for the year leading up to VPExam QI. During the initial 6 months of VPExam QI, the average monthly 30-day readmission rate for all University Hospital of Cleveland Regional Hospitals fell to 7.98%. 0% readmissions found for the last 4 consecutive months of VPExam QI.
Across heart failure subtypes, patients with heart failure mortality rate following hospitalization were approximately 10.4% at 30 days, 22% at 1 year, and 42.3% at 5 years [8]. 30-day mortality in VPExam QI was significantly lower at 30 days at 4.54% with a relative risk reduction of 56.3 % compared to historical controls.
Discussion
Virtual care barriers
Significant barriers identified in literature review preventing successful integration of quality improvement initiatives include:
1. The presentation of HF can be non-specific and make it difficult to diagnose
2. Guideline-directed drugs are underused due to doubt on their utility and safety concerns
3. SNF providers uncomfortable managing HF due to complexity and autonomy at end-of-life decisions
4. There is mistrust and lack of timely communication between SNF staff, patients, and their families
5. There are limited resources in terms of diagnostic studies and access to specialists for care of patients
6. There is poor information sharing and transfer capabilities [2,6,9,10].
VPExam QI reveals unique VPExam tools overcome many of these barriers while creating a successful local Virtual Care Network between hospital systems and Partner SNFs and Home care. VPExam deployment to SNFs and Home Care is feasible, scalable, and cost effective. VPExam Virtual Care Networks enable high compliance with follow-up with high satisfaction from nursing staff. Structured data transmission of vitals improved detection of uncontrolled hypertension, hypotensive episodes, and tachyarrhythmias often missed in traditional telemedicine. Structured data transmission of medication reconciliation often identified high risk transition of care errors. Structured data transmission of labs including renal function, Brain Natriuretic Peptide (BNP) trends, and blood count stability improved the quality of medical decision making.
VPExam is also uniquely suited to improve clinical decisions with unique physical exam data. Volume status including jugular venous distention and lower extremity edema influenced moderate modification management in 50% of encounters. Synchronous and asynchronous stethoscope auscultation of the heart to detect murmurs, rubs, gallops, irregularity, as well as auscultation of the lungs to detect wheezing and rhonchi influenced moderate modification management in over 31% of encounters. Synchronous and asynchronous single lead ECG transmission for arrythmia detection including atrial fibrillation influenced moderate modification management in over 13.6% of encounters.
There are also financial considerations for various stakeholders. Transfer of Skilled Nursing Facility (SNF) residents to emergency departments are linked to increased morbidity and mortality as well as significant cost [9]. The average cost of readmission is $15,200 across various payers. Within cardiology, there are over 233,100 readmissions for heart failure, 81,600 readmissions for cardiac arrythmias, and 74,300 readmissions following myocardial infarct annually. Other high-risk conditions with benefit from VPExam cardiopulmonary and volume status evaluation include COPD with 106,300 readmissions, pneumonia with 7,500 readmissions, and renal failure with 96,900 readmissions annually [11].
Virtual care feasibility
VPExam QI results demonstrate that virtual care in transitions of care to SNFs and Home Care offer a large opportunity to improve quality of care and mitigate risk of errors for cardio-pulmonary patients. The reduction in 30-day hospitalization and mortality supports that unique Virtual Care data empowers care providers to optimize transitional quality of care.
VPExam helps reduce the cost of transporting patients to specialists and hospitals including ambulance cost and nursing time expenses. Virtual care also helps reduce the risk of contracting infectious diseases such as COVID while visiting the health care. In addition to the financial incentivization to utilizing virtual care to mitigate the cost of readmissions, the platform can also increase individual provider productivity.
Virtual care offers earlier detection of clinical decompensation to underserved communities and better decisions by clinicians resulting in reduced risk of hospital admission and mortality on discharge. In turn, improved transitional care assists health care systems in preventable penalties, unnecessary care escalation, and more efficient utilization of limited inpatient and ICU beds.
Transitional outlook of virtual care
Implementing virtual care to improve transitions of care in the underserved SNF and Home Care patient populations represents a promising measure to address high readmission rates in HF patients. VPExam offers capabilities to efficiently transmit virtual physical exam cardio-pulmonary and volume status assessments with supplemental structured data including vitals, medication reconciliation, and labs critical to heart failure management.
Conclusion
Noninvasive virtual care platforms offer novel interventions to optimize quality of care impacting readmission and mortality rates. Future projects should focus not only on how virtual care can be integrated to provide better quality of care, but also address the paradigm of cost-effective health care delivery given the growing challenges of health care resource scarcity. Ongoing government and hospital support for digital innovation research allow physicians the opportunity to define the way developing technologies will be used in future workflows to optimize efficiency and quality of care.
References
- Ponikowski P, Voors AA, Anker SD, et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 37(27): 2129-2200 (2016).
- Orr NM, Forman DE, De Matteis G, et al. Heart failure among older adults in skilled nursing facilities: More of a dilemma than many now realize. Curr Geriatr Rep. 4(4): 318-326 (2015).
[CrossRef] [Google Scholar] [PubMed]
- Jurgens CY, Goodlin S, Dolansky M, et al. Heart failure management in skilled nursing facilities: A scientific statement from the American Heart Association and the Heart Failure Society of America. Circ Heart Fail. 8(3): 655-87 (2015).
- Zhu Y, Gu X, Xu C. Effectiveness of telemedicine systems for adults with heart failure: A meta-analysis of randomized controlled trials. Heart Fail Rev. 25(2): 231-243 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Gingele AJ, Ramaekers B, Brunner-La Rocca HP, et al. Effects of tailored telemonitoring on functional status and health-related quality of life in patients with heart failure. Neth Heart J. 27(11): 565-574 (2019).
[CrossRef] [Google Scholar] [PubMed]
- Woo K, Dowding D. Factors affecting the acceptance of Telehealth services by heart failure patients: An integrative review. Telemed J E Health. 24(4): 292-300 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Shah N, Annam A, Cireddu NJ, et al. VPExam virtual care for heart failure optimizing transitions of care quality improvement project (VPExam QI). Cardiovasc Digit Health J. 3(3): 146-155 (2022).
[CrossRef] [Google Scholar] [PubMed]
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation. 135(10): e146-e603 (2017).
[CrossRef] [Google Scholar] (All versions) [PubMed]
- Joseph JW, Kennedy M, Nathanson LA, et al. Reducing emergency department transfers from skilled nursing facilities through an emergency physician telemedicine service. West J Emerg Med. 21(6): 205-209 (2020).
[CrossRef] [Google Scholar] [PubMed]
- Heckman GA, Shamji AK, Ladha R, et al. Heart failure management in nursing homes: A scoping literature review. Can J Cardiol. 34(7): 871-880 (2018).
[CrossRef] [Google Scholar] [PubMed]
- Weiss AJ, Jiang HJ. Overview of clinical conditions with frequent and costly hospital readmissions by payer, 2018: Statistical Brief #278. HCUP User Support. (2021).
[Google Scholar] [PubMed]