Short Article - Interventional Cardiology (2012) Volume 4, Issue 2
What do we know about the natural history of severe symptomatic aortic valve stenosis?
- Corresponding Author:
- Özcan Birim
Department of Cardio-Thoracic Surgery
Room BD 575, Erasmus MC, Dr Molewaterplein 40
3015 GD, Rotterdam, The Netherlands
Tel: +31 10 703 5412
Fax: +31 10 703 3993
E-mail: o.birim@erasmusmc.nl
Abstract
Keywords
aortic valve stenosis, medical treatment, severe, symptomatic
After hypertension and coronary artery disease, aortic valve stenosis (AS) is the most frequent cardiovascular disease. AS is increasingly observed in octogenarians and even in nonagenarians. The prevalence of AS is currently reported to be 2.5% at the age of 75 years and almost 8% at 85 years [1].
Angina pectoris, syncope and congestive heart failure are the classic manifestations of severe symptomatic AS. However, severe symptomatic AS may manifest clinically in earlier stages with more subtle symptoms, such as decrease in exercise tolerance, fatigue or exertional dyspnea. The onset of symptoms is a critical point for making treatment decisions. It has been reported that only 50% of patients who present with angina survive for 5 years or more, whereas the average survival is 3 years for patients who present with syncope and 2 years in patients with congestive heart failure [2].
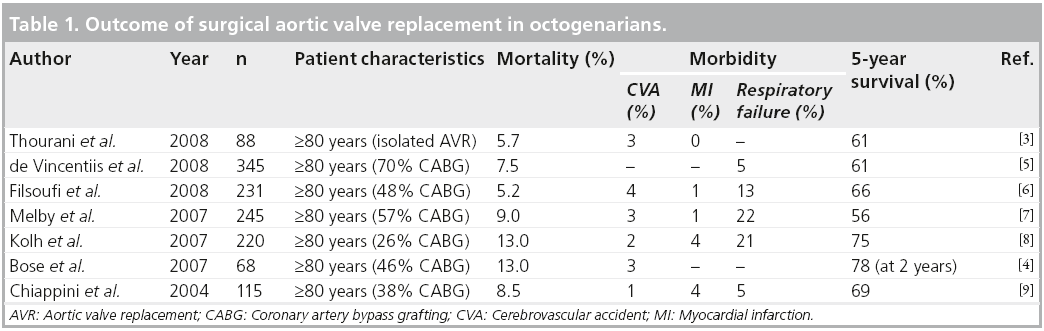
At present, surgical aortic valve replacement is the gold standard for treatment of severe symptomatic AS and numerous reports document the safety and efficacy of this approach even in elderly patients. However, elderly patients experience higher morbidity and mortality compared with younger patients, with mortality rates ranging from 5.7 to 13% (Table 1) [3–9]. Although consensus exists regarding the utility of aortic valve replacement for severe symptomatic AS, the decision to offer surgery to the elderly highrisk population is much more complex. Some patients are physically unfit for surgery, or surgery is denied because of a treatment preference of either the patient or the physician. Certain comorbid factors, such as preoperative cerebrovascular accident, respiratory insufficiency, renal failure and reduced left ventricular function, are independent predictors of in-hospital mortality in octogenarians [3,5,6].
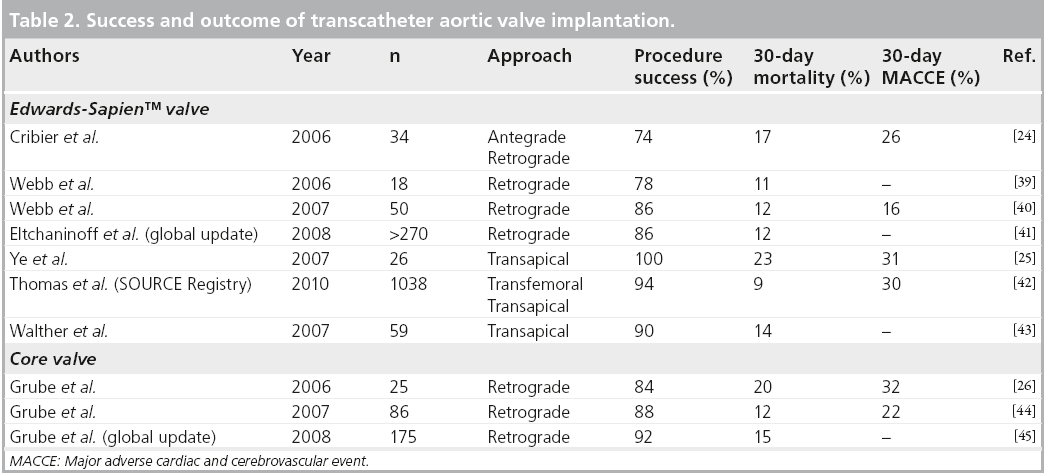
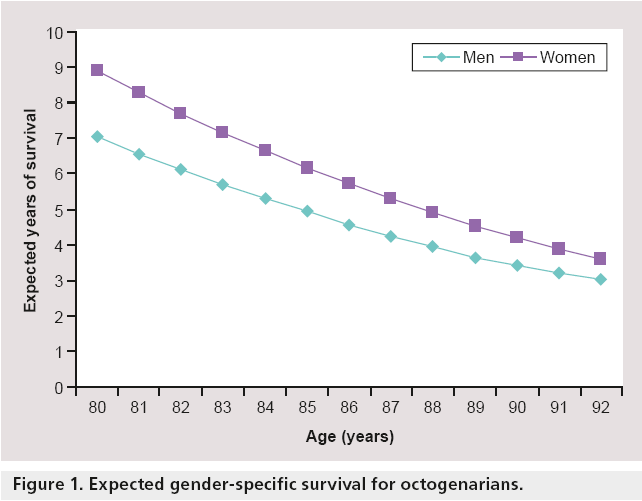
At present, patients who are high-risk candidates for surgical valve replacement may be offered transcatheter aortic valve implantation (TAVI). Although promising, periprocedural complications and mortality rate are significant (Table 2). The prognosis is influenced by increased age (patient’s life expectancy) and various comorbidities. In this setting, the cardiologist and surgeons have to balance the mortality and morbidity associated with surgery or TAVI against the expected duration and quality of life with medical treatment, as the life expectancy of elderly people is short, regardless of whether or not the patient has severe symptomatic AS (Figure 1). The benefit of surgery or alternative treatment methods such as TAVI is uncertain because the majority of information about the outcome of medical treatment dates back to the presurgical and precatheterization era [2]. Therefore, the aim of this article is to outline the evidence of natural history with medical treatment to assist in optimal clinical decisionmaking in the high-risk elderly population with severe symptomatic AS.
Natural history: the evidence
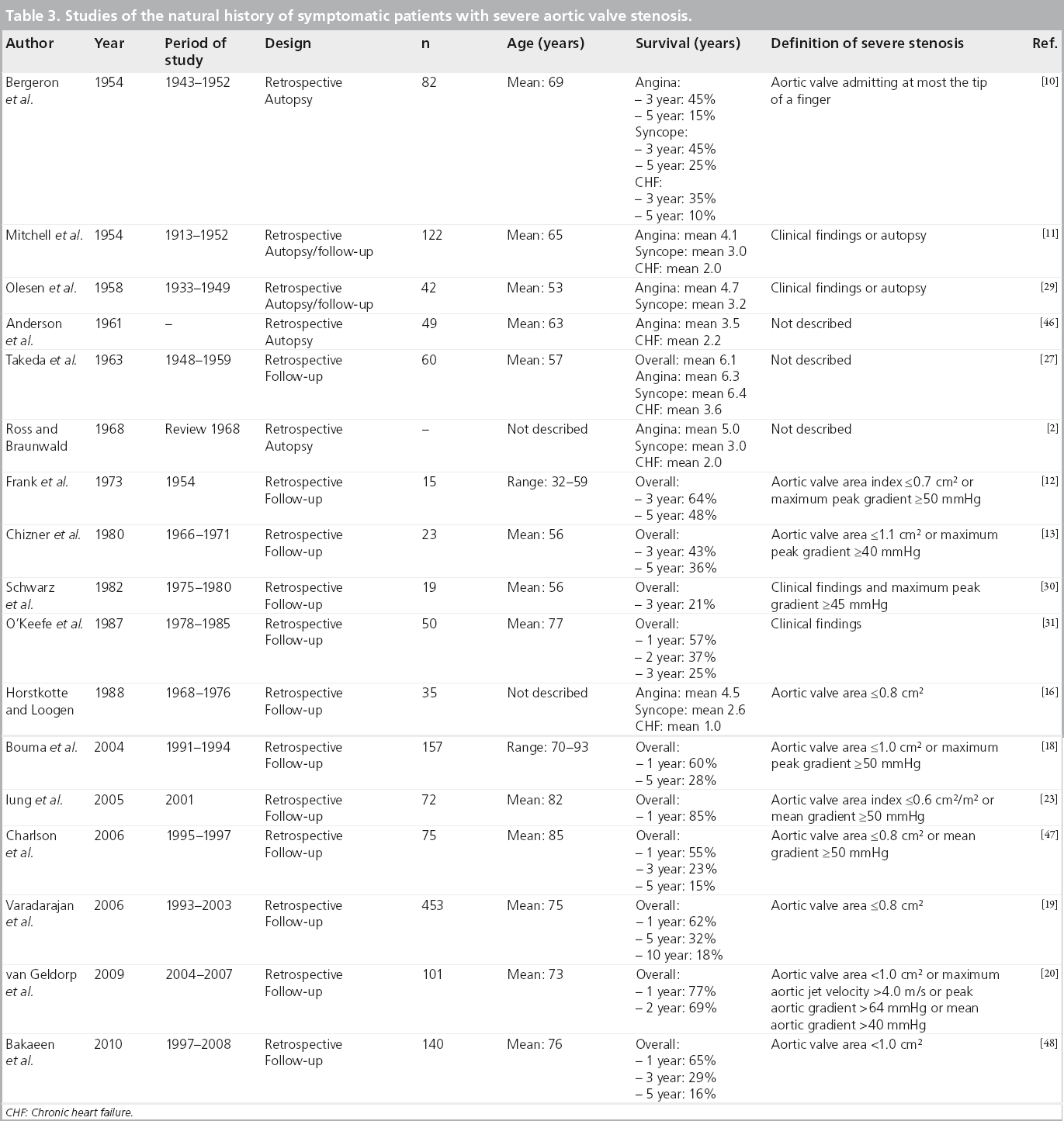
The first report presenting survival data of patients treated conservatively for severe symptomatic AS was published in 1954. Bergeron et al. described the natural history outcome of 82 patients, mean age of 69 years, with severe symptomatic AS who had been followed up over an 11-year period [10]. All patients were examined at necropsy at which severe AS was described as “an aortic valve admitting at most the tip of a finger”. In their analysis, 3-year survival was 45% in patients presenting with angina, 45% in patients with syncope and 35% in patients with congestive heart failure (Table 3). In line with these observations, the next important contribution to the understanding of the natural history of severe symptomatic AS was also in 1954 by Mitchell et al. [11]. Over a 39-year period, they investigated the natural history outcome in 122 patients with severe symptomatic AS. Aortic stenosis was proven at autopsy, or the diagnosis was made clinically and verified by the demonstration of calcium in the region of the aortic valve by x-ray and fluoroscopic study. Mean survival in patients presenting with angina, syncope and congestive heart failure was 4.1, 3.0 and 2.0 years, respectively.
Table 3: Studies of the natural history of symptomatic patients with severe aortic valve stenosis.
In 1968, still before the era of hemodynamic assessment of AS severity, Ross and Braunwald summarized data from seven postmortem studies on the natural history of severe symptomatic AS [2]. Most of these studies were retrospective and published before 1955. Based on their analysis, they observed that the average life expectancy after the onset of angina pectoris, syncope and congestive heart failure was 5, 3 and 2 years, respectively. Ever since, these data have become commonly used to describe the natural history of severe symptomatic AS.
In the decade after this report, two studies assessed the hemodynamic consequence of valvular obstruction in severe symptomatic patients with AS [12,13]. In a report by Frank et al. comprising 15 patients, the 5- and 10-year survival rates were 48 and 10%, respectively [12]. Among the 23 patients reported by Chizner et al., 26% were deceased 1 year after the onset of symptoms and 64% by 5 years [13]. Not surprisingly, a prospective study examining the natural history of severe symptomatic AS has not been conducted since the introduction of aortic valve replacement. Because of the limited number of patients who were not operated on for severe symptomatic AS, some studies retrospectively identified the natural history of patients who refused or were denied aortic valve replacement [12–17]. The natural history of this small subset of highly selected patients probably does not represent the natural history of all patients with severe symptomatic AS.
In 2004, Bouma et al. reported on a cohort of 280 elderly patients with severe symptomatic AS of which 120 were operated upon and 160 were treated conservatively [18]. The overall 1-year survival of these 160 patients was 60% and the 5-year survival was 28%. They found no difference in survival among patients ≥80 years with severe symptomatic AS and without cardiac comorbidity. One of the most recent series was published by Varadarajan et al. in 2006 [19]. In this study, the authors screened their echocardiographic database over a 10-year period for patients with severe AS (Doppler estimated aortic valve area [AVA] of 0.8 cm² or less). Seven hundred and forty patients were identified, of whom 453 had no aortic valve replacement through follow-up. These patients had a 1-, 5- and 10-year survival of 62, 32 and 18%, respectively. In a recent series, van Geldorp et al. also screened the Erasmus MC echocardiographic database over a 3.5-year period for patients with severe symptomatic AS [20]. One hundred and seventy seven patients were identified, of whom 101 were treated conservatively. These patients had a 1- and 2-year survival of 77 and 69%, respectively.
The most recent series was published in 2010 by Rajani et al. [21]. The authors published a series of 85 patients who were screened for TAVI. Of these patients, 38 received TAVI and 47 patients (55%) were managed medically as these patients were deemed not suitable for a TAVI procedure. Survival was better for the TAVI group compared with the medically managed group. However, as medically treated patients were deemed not suitable for TAVI, these results are biased owing to selection bias.
Discussion
Successful cardiac surgical therapy in octogenarians and nonagenarians is increasingly performed and the number of procedures will increase even further over the coming years as healthcare in general improves and the population ages. Despite the high risk, surgical valve replacement is still the gold standard in those patients who are medically fit and have severe symptomatic AS. The decision to proceed with aortic valve replacement depends on many factors, including the patient’s wishes and expectations. However, some patients are at high risk due to several reasons and some will refuse surgery, even with a clear understanding of the risks and benefits.
The development of TAVI offers a viable option for patients at high surgical risk. Recent studies have highlighted the underuse of aortic valve replacement, ranging from 30 to 60% of elderly patients with severe symptomatic AS [22,23]. As a result of the emergence of TAVI, some high-risk patients are now being referred because the strategy of the cardiologists is changing. The feasibility and immediate efficacy of the percutaneous devices have been demonstrated, while its long-term outcomes, particularly with respect to device durability, remains to be proven. However, the rates of periprocedural complications and major adverse cardiac and cerebrovascular event rates within 30 days are of concern and need further improvement [24–26].
The hand drawn survival figure, based on data from seven postmortem studies on the natural history of AS, published by Ross and Braunwald in 1968 is still being used in current clinical practice as the accepted clinical view regarding the natural history of severe symptomatic AS [2]. However, the natural history studies described in this article have significant limitations when extrapolating findings to current clinical decision-making. Studies in which prognosis is based only on postmortem cases are biased, because prognosis will appear better if living patients with symptoms are also included. For example, Takeda et al. reported an average survival of 4.4, 3.8 and 2.8 years after angina, syncope and congestive heart failure, respectively [27]. However, they excluded living patients in their calculation. If living patients were included, mean survival calculations would be 6.3, 6.4 and 3.6 years after angina, syncope and congestive heart failure, respectively.
A problem that has arisen in clinical practice is the definition of ‘severe’ AS. Over recent years, echocardiography has evolved to become the major tool for evaluating patients with valvular AS. At present, severe AS is defined by the American College of Cardiology/American Heart Association Practice Guidelines as an AVA less than 1.0 cm², mean gradient greater than 40 mmHg or jet velocity greater than 4.0 m/s [28]. In the past, the severity of AS was based on clinical examination [11,27,29–31]. As cardiac catheterization evolved and provided an objective measurement of the severity of AS by means of the AVA, the criterion for severe AS was first set as an AVA less than 0.7 cm2 [32]. However, the precise hemodynamic criterion for ‘severe’ AS has varied in the past (Table 3). As a consequence, the validity (patient generalizability) of earlier studies must be questioned.
Coronary angiography was not performed in most of the published series, although the presence of coronary artery disease is clearly a major risk factor for mortality. In a study by Turina et al., 50% of patients with severe symptomatic AS with additional coronary artery disease died within the first year of follow-up, while only 16% of patients without coronary artery disease died [33]. Therefore, survival and symptoms may even be improved if medically treated patients undergo percutaneous coronary intervention of significant coronary lesions.
Furthermore, treatment decisions made in the past differ greatly from those of today. For example, today an impaired left ventricular function would be an indication for operation [34], whereas in the past it would be considered a relative contraindication. In addition, the etiology of AS and the characteristics of the patient population have changed markedly over the past decades, and it can be questioned whether the course of AS in middle-aged patients of the 1960s should guide the management of today’s octogenarians and nonagenarians with severe symptomatic AS. Moreover, studies have involved few elderly patients and have reported on combined end points (e.g., a combination of death and cardiac surgery), which makes their results difficult to interpret [16,35,36].
Important 1-year data of the randomized trial in the USA, PARTNER-US, in which TAVI is compared with standard therapy in a group of patients unsuitable for surgical aortic valve replacement have recently been published [37]. At 1 year, the rate of death was 31% with TAVI, as compared with 50% with standard therapy (p < 0.001). However, the incidence of major strokes at 30 days (5.0 vs 1.1%; p = 0.06) and major vascular complications (16.2 vs 1.1%; p < 0.001) was higher with TAVI as compared with standard therapy. These data must be interpreted with caution as patients in the TAVI group compared with the standard therapy group had a significantly lower incidence of prognostic factors that have an effect on outcome, such as a lower EuroSCORE, lower rate of chronic obstructive pulmonary disease and lower rate of atrial fibrillation. Moreover, only 12% of those patients considered not be suitable candidates for surgery were considered suitable for TAVI and underwent randomization. An important issue in the future will be the cost–benefit of TAVI versus medical therapy, since after 1 year 31% of the TAVI patients are dead and 20% have severe symptoms (New York Heart Association Class 3 or 4), resulting in a 1 year asymptomatic or mild symptomatic survival of only 50%. Nevertheless, recently Reynolds et al. showed that among selected inoperable patients with severe symptomatic AS, compared with standard therapy, TAVI resulted in significant improvements in health-related quality of life [38].
Management decision in elderly high-risk patients with severe symptomatic AS must be taken thoughtfully and should be made on an individual basis, taking into account patients’ life expectancy and quality of life, patients’ wishes and cardiac and noncardiac comorbid factors. Once coronary disease, other valvular heart disease, neurological deficits, renal failure and other comorbidities are added to the clinical setting, outcome worsens and these factors must be taken into consideration when deciding whether to correct AS in elderly patients. As life expectancy in the octogenarian is short and the main aim in the elderly is to improve quality of life rather than to increase the duration of life, surgeons and cardiologists have to question whether they do their patients a favor or a disservice with the chosen therapy. Based on the available data, TAVI promises significantly improved 1-year survival when compared with medical management. Nevertheless, the technology of TAVI is still in its infancy and rigorous evaluation of transcatheter technology with adequate follow-up is needed. In addition, the natural history of medically managed patients with severe symptomatic AS in the modern era is still unclear, as most published data is outdated or biased. In this regard, much remains to be learned about the current natural history of severe symptomatic AS, especially in high-risk elderly patients.
Future perspective
At present, surgical aortic valve replacement is still the gold standard for treatment of severe symptomatic AS. However, TAVI has been proven to be a feasible treatment option to treat high-risk inoperable elderly patients with severe symptomatic AS. An assessment of the durability and long-term clinical safety and effectiveness of the bioprosthetic valves will require more prolonged follow-up of patients who participate in clinical trials of TAVI.
The key issue in the future is to adequately select those elderly patients who will benefit from TAVI and select those who will benefit from medical treatment. For example, treatment options could be different in an 85-yearold patient with severe AS, mild angina and comorbidity (medical treatment could be a better option) compared with an 85-year-old patient with severe AS, congestive heart failure and no further comorbidity (TAVI could be a better option). Additional randomized trials on specific patient populations with certain symptoms and comorbidity is necessary to determine the best treatment option in those groups of patients. In addition, a clinical course of patients who are denied TAVI (which was 88% in the PARTNER-US trial) should be documented.
Financial and competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Executive summary
▪ Surgical aortic valve replacement is still the gold standard for treatment of severe symptomatic aortic valve stenosis.
▪ Patients who are inoperable or high-risk candidates may be offered transcatheter aortic valve implantation.
▪ The feasibility and immediate efficacy of transcatheter aortic valve implantation has been demonstrated, while its long-term outcome, particularly with respect to device durability, remains to be proven.
▪ The majority of published series describing the natural history of severe symptomatic aortic valve stenosis are biased because most reported series are postmortem studies and date back to the presurgical and precatheterization era, or are biased due to highly selected patient populations.
▪ The first randomized trial (PARTNER-US) comparing transcatheter aortic valve implantation with medical therapy in a group of inoperable patients with severe symptomatic aortic valve stenosis clearly demonstrates an improved 1-year survival in the transcatheter group. However, data cannot be extrapolated to all inoperable patients since the study population was highly selected (only 12% of inoperable patients were included in the study).
▪ The natural history of medically treated patients with severe symptomatic aortic valve stenosis in the modern era is still unclear. Additional randomized trials on specific patient populations with certain symptoms and comorbidity is necessary. The clinical course of patients who are denied transcatheter aortic valve implantation should be documented.
References
- Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J. Am. Coll. Cardiol. 21(5), 1220–1225 (1993).
- Ross J Jr, Braunwald E. Aortic stenosis. Circulation 38(Suppl. 1), 61–67 (1968).
- Thourani VH, Myung R, Kilgo P et al. Long-term outcomes after isolated aortic valve replacement in octogenarians: a modern perspective. Ann. Thorac. Surg. 86(5), 1458–1465 (2008).
- Bose AK, Aitchison JD, Dark JH. Aortic valve replacement in octogenarians. J. Cardiothorac. Surg. 2, 33 (2007).
- de Vincentiis C, Kunkl AB, Trimarchi S et al. Aortic valve replacement in octogenarians: is biologic valve the unique solution? Ann. Thorac. Surg. 85(4), 1296–1301 (2008).
- Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Silvay G, Adams DH. Excellent early and late outcomes of aortic valve replacement in people aged 80 and older. J. Am. Geriatr. Soc. 56(2), 255–261 (2008).
- Melby SJ, Zierer A, Kaiser SP et al. Aortic valve replacement in octogenarians: risk factors for early and late mortality. Ann. Thorac. Surg. 83(5), 1651–1657 (2007).
- Kolh P, Kerzmann A, Honore C, Comte L, Limet R. Aortic valve surgery in octogenarians: predictive factors for operative and long-term results. Eur. J. Cardiothorac. Surg. 31(4), 600–606 (2007).
- Chiappini B, Camurri N, Loforte A, Di Marco L, Di Bartolomeo R, Marinelli G. Outcome after aortic valve replacement in octogenarians. Ann. Thorac. Surg. 78(1), 85–89 (2004).
- Bergeron J, Abelmann WH, Vazquez-Milan H, Ellis LB. Aortic stenosis; clinical manifestations and course of the disease; review of one hundred proved cases. AMA Arch. Intern. Med. 94(6), 911–924 (1954).
- Mitchell AM, Sackett CH, Hunzicker WJ, Levine SA. The clinical features of aortic stenosis. Am. Heart J. 48(5), 684–720 (1954).
- Frank S, Johnson A, Ross J Jr. Natural history of valvular aortic stenosis. Br. Heart J. 35(1), 41–46 (1973).
- Chizner MA, Pearle DL, deLeon AC Jr. The natural history of aortic stenosis in adults. Am. Heart J. 99(4), 419–424 (1980).
- Braunwald E. On the natural history of severe aortic stenosis. J. Am. Coll. Cardiol. 15(5), 1018–1020 (1990).
- Rapaport E. Natural history of aortic and mitral valve disease. Am. J. Cardiol. 35(2), 221–227 (1975).
- Horstkotte D, Loogen F. The natural history of aortic valve stenosis. Eur. Heart J. 9(Suppl. E), 57–64 (1988).
- Iivanainen AM, Lindroos M, Tilvis R, Heikkila J, Kupari M. Natural history of aortic valve stenosis of varying severity in the elderly. Am. J. Cardiol. 78(1), 97–101 (1996).
- Bouma BJ, van den Brink RB, Zwinderman K et al. Which elderly patients with severe aortic stenosis benefit from surgical treatment? An aid to clinical decision making. J. Heart Valve Dis. 13(3), 374–381 (2004).
- Varadarajan P, Kapoor N, Bansal RC, Pai RG. Clinical profile and natural history of 453 nonsurgically managed patients with severe aortic stenosis. Ann. Thorac. Surg. 82(6), 2111–2115 (2006).
- van Geldorp MW, van Gameren M, Kappetein AP et al. Therapeutic decisions for patients with symptomatic severe aortic stenosis: room for improvement? Eur. J. Cardiothorac. Surg. 35(6), 953–957 (2009).
- Rajani R, Buxton W, Haworth P et al. Prognostic benefit of transcatheter aortic valve implantation compared with medical therapy in patients with inoperable aortic stenosis. Catheter. Cardiovasc. Interv. 75(7), 1121–1126 (2010).
- Bouma BJ, van Den Brink RB, van Der Meulen JH et al. To operate or not on elderly patients with aortic stenosis: the decision and its consequences. Heart 82(2), 143–148 (1999).
- Iung B, Cachier A, Baron G et al. Decisionmaking in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur. Heart J. 26(24), 2714–2720 (2005).
- Cribier A, Eltchaninoff H, Tron C et al. Treatment of calcific aortic stenosis with the percutaneous heart valve: mid-term follow-up from the initial feasibility studies: the French experience. J. Am. Coll. Cardiol. 47(6), 1214–1223 (2006).
- Ye J, Cheung A, Lichtenstein SV et al. Six-month outcome of transapical transcatheter aortic valve implantation in the initial seven patients. Eur. J. Cardiothorac. Surg. 31(1), 16–21 (2007).
- Grube E, Laborde JC, Gerckens U et al. Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: the Siegburg first-in-man study. Circulation 114(15), 1616–1624 (2006).
- Takeda J, Warren R, Holzman D. Prognosis of aortic stenosis; special reference to indications for operative treatment. Arch. Surg. 87, 931–936 (1963).
- Bonow RO, Carabello BA, Chatterjee K et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 48(3), e1–e148 (2006).
- Olesen KH, Warburg E. Isolated aortic stenosis; the late prognosis. Acta Med. Scand. 160(6), 437–446 (1958).
- Schwarz F, Baumann P, Manthey J et al. The effect of aortic valve replacement on survival. Circulation 66(5), 1105–1110 (1982).
- O’Keefe JH Jr, Vlietstra RE, Bailey KR, Holmes DR Jr. Natural history of candidates for balloon aortic valvuloplasty. Mayo Clin. Proc. 62(11), 986–991 (1987).
- Selzer A. Changing aspects of the natural history of valvular aortic stenosis. N. Engl. J. Med. 317(2), 91–98 (1987).
- Turina J, Hess O, Sepulcri F, Krayenbuehl HP. Spontaneous course of aortic valve disease. Eur. Heart J. 8(5), 471–483 (1987).
- Robiolio PA, Rigolin VH, Hearne SE et al. Left ventricular performance improves late after aortic valve replacement in patients with aortic stenosis and reduced ejection fraction. Am. J. Cardiol. 76(8), 612–615 (1995).
- Kennedy KD, Nishimura RA, Holmes DR Jr, Bailey KR. Natural history of moderate aortic stenosis. J. Am. Coll. Cardiol. 17(2), 313–319 (1991).
- Otto CM. Valvular aortic stenosis: disease severity and timing of intervention. J. Am. Coll. Cardiol. 47(11), 2141–2151 (2006).
- Leon MB, Smith CR, Mack M et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N. Engl. J. Med. 363(17), 1597–1607 (2010).
- Reynolds MR, Magnuson EA, Lei Y et al. Health-related quality of life after transcatheter aortic valve replacement in inoperable patients with severe aortic stenosis. Circulation 124(18), 1964–1972 (2011).
- Webb JG, Chandavimol M, Thompson CR et al. Percutaneous aortic valve implantation retrograde from the femoral artery. Circulation 113(6), 842–850 (2006).
- Webb JG, Pasupati S, Humphries K et al. Percutaneous transarterial aortic valve replacement in selected high-risk patients with aortic stenosis. Circulation 116(7), 755–763 (2007).
- Eltchaninoff H, Zajarias A, Tron C et al. Transcatheter aortic valve implantation:technical aspects, results and indications. Arch. Cardiovasc. Dis. 101(2), 126–132(2008).
- Thomas M, Schymik G, Walther T et al. Thirty-day results of the Sapien AorticBioprosthesis European Outcome (SOURCE)registry: a European registry of transcatheteraortic valve implantation using the EdwardsSapien valve. Circulation 122(1), 62–69(2010).
- Walther T, Falk V, Borger MA et al. Minimally invasive transapical beating heartaortic valve implantation – proof of concept. Eur. J. Cardiothorac. Surg. 31(1), 9–15 (2007).
- Grube E, Schuler G, Buellesfeld L et al. Percutaneous aortic valve replacement forsevere aortic stenosis in high-risk patientsusing the second-and current thirdgenerationself-expanding CoreValveprosthesis: device success and 30 day clinicaloutcome. J. Am. Coll. Cardiol. 50(1), 69–76(2007).
- Grube E, Ulrich G, Schuler G et al. Experience with CoreValve aortic valvereplacement in patients for surgical aorticvalve replacement. J. Am. Coll. Cardiol. Intv. 1(Suppl. B), 21 (2008).
- Anderson MW. The clinical course of patientswith calcific aortic stenosis. Proc. Staff Meet. Mayo Clin. 36, 439–444 (1961).
- Charlson E, Legedza AT, Hamel MB.Decision-making and outcomes in severesymptomatic aortic stenosis. J. Heart Valve Dis. 15(3), 312–321 (2006).
- Bakaeen FG, Chu D, Ratcliffe M et al. Severeaortic stenosis in a veteran population:treatment considerations and survival. Ann. Thorac. Surg. 89(2), 453–458 (2010).