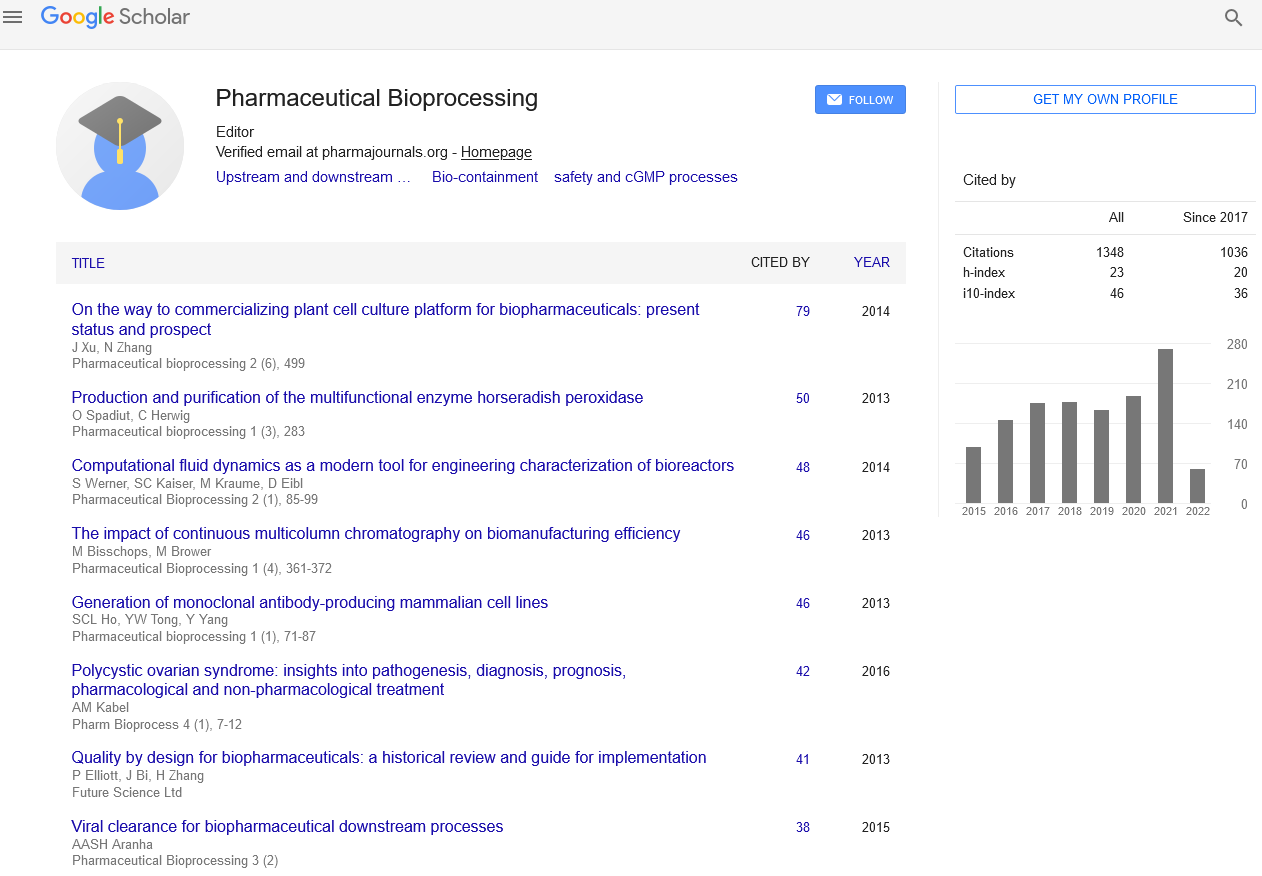
Short Communication - Pharmaceutical Bioprocessing (2020) Volume 8, Issue 2
World Drug Delivery 2016- Nanoparticle and microparticle-based drug delivery of ophthalmic pharmaceuticals- Irach B. Taraporewala - Sitara Pharmaceutical Group
- *Corresponding Author:
- Irach B. Taraporewala
Sitara Pharmaceutical Group, USA
E-mail: irachtaraporewala@ohrpharmaceutical.com
Abstract
Nanoparticle and microparticle drug delivery is a highly attractive prospect for the development of future ophthalmic pharmaceutical products. For chronic ocular diseases such as glaucoma, where Patient compliance with eye drop therapy is low, sustained release therapy via nanoparticle or microparticle drug delivery approaches is especially of promise. It also is a viable approach for treatments post ophthalmic surgical procedures. While the ocular anatomy provides for a number of physical barriers for drug molecule entry, penetration and release in therapeutically viable concentrations at the specific site within the eye where it is therapeutically required, newer approaches to nanoparticle and microparticle design and fabrication also allow for the targeting of the innermost structures of the eye such as the macula and retinal pigment epithelium through such delivery systems. The presentation will address the novel biopolymeric materials, fabrication techniques and therapeutic approached currently being developed as advances in nanotechnology and microparticle technology for ophthalmic indications including cationic, amphoteric and non-ionic particle technologies and non-emulsion based fabrication techniques such as the use of hydrogel templates and 3D printing approaches to the generation of nanoparticles and microparticles for ophthalmic treatments. The regulatory technical challenges of developing such novel ophthalmic drug products and their solutions will also be addressed.
There is a relatively high prevalence of blinding eye diseases in the developing nations, which by some estimates are 10- to 40-fold higher than that in the developed countries. For example, in Saudi Arabia, over 1.5% of the total population, and over 20% of the population over 60 years of age are estimated to be blind by the World Health Organization criteria.1 The leading causes of blindness in Saudi Arabia include cataracts, trachoma, corneal scars, glaucoma, retinal degenerative diseases such as diabetic retinopathy (DR), age-related macular degeneration (AMD) and congenital anomalies.1 Some of these are related to, and exacerbated by, the high incidence of Diabetes Mellitus, with an overall prevalence of over 23% of the population.2 A report by the Saudi Ministry of Health suggests that diabetes and obesity may be on the increase.3 Therefore, there is an increased recognition, especially in Saudi Arabia and the Middle East, that eye diseases are a major health problem, leading to a high socio-economical burden.3 Major Saudi Arabian government research and technological initiatives are underway, both in medicine and nanotechnology that may pave the way for novel therapeutic applications through multi-disciplinary collaborations between governments, researchers from many countries and industries.The field of ‘nanomedicine’ uses nanoscale technologies (≤100 nm, typically) for the diagnosis, treatment and/or prevention of diseases, as well as to gain an understanding of the pathophysiology of various diseases, with an ultimate goal of improving quality of life.5 In this respect, nanomedicine offers numerous advantages compared to treatments with drugs alone. These include sustained delivery of therapeutic agents, targeted delivery of drugs to specific cells or tissue, improved delivery of both water-insoluble drugs and large biomolecule drugs, and reduced side effects.6–8 Liposomes are small spherical vesicles, typically composed of lipid bilayers surrounding aqueous inner phase. The bilayers and the inner aqueous phase can act as the reservoir for hydrophobic drugs and hydrophilic drugs, respectively.9,10 Liposomes are one example of nanomedicines that have been previously used in ocular drug delivery.9,11–13 Liposome-based ocular drug-delivery systems were described as early as in 1981 by Smolin et al.14 The encapsulation of idoxuridine into liposomes increased the corneal penetration of the drug,15 and showed improved efficacy in controlling Herpetic keratitis in comparison to the free drug solution.14 Subsequently, a variety of other biomaterials for ocular drug delivery have been developed, including polymeric nanoparticles,16,17 dendrimers,18 and hydrogels19 [Figure 1], that may be administered in a versatile manner. In this mini-review, we highlight recent developments in polymer and nanotechnology based drug-delivery systems for the anterior and posterior segments of the eye. Successful translation of these promising approaches would require a careful assessment of both the risk and reward arising from the use of the nanomedicines and we discuss both these aspects in this review.
The incidence of topical and corneal infections have increased in recent years owing to an increased number of corneal surgeries for cataracts, glaucoma and corneal transplantations, and the increased use of contact lenses. Even though the cornea is protected from the external environment by a continuous tear fluid film that turns over rapidly, a variety of microorganisms can invade the cornea, leading to keratitis or conjunctivitis. Such ocular infections can cause major health problems if untreated, causing corneal reddening, opacification, rupture, irritation and inflammation, leading to obscure vision and even permanent blindness.20 Drug-delivery systems that improve drug residence time on the corneal surface can have a significantly positive impact. Improved pre-corneal residence time can increase the absorption of drugs through periocular tissue to even reach the inner ocular tissues. The enhanced drug bioavailability can down the frequency of drug administration, and rise thepatient compliance. Various nanomedicine strategies, such as the mucoadhesive nanoparticles and drug-eluting contact lenses have been explored, and are highlighted here.
Improving corneal residence time
Even though eye drops are the most conventional formulation for ocular drug delivery, they typically provide low bioavailability (less than 5%) owing to poor pre-corneal retention and penetration. The factors affecting pre-corneal retention include rapid tear turnover, blinking, and solution drainage, which result in the loss of drug after topical administration. Therefore, frequent instillations of eye drops are required to maintain a therapeutic drug level on the pre-corneal surface. Frequent use of concentrated eye drops can induce toxicity, corneal dryness and possible severe systemic side effects.
Tear liquid contains secreted mucins and surface associated mucins. The mucins form a hydrophobic blanket that moves over the ocular surface to clear debris and pathogens. Prior studies have suggested that charged polymers (both cationic and anionic) could have hydrogen bonding and electrostatic interactions with mucins, rendering them ‘mucoadhesive’ Mucoadhesive forces between an anionic polymer surfactant (Carbopol®) and mucins, attributable to hydrogen bonding interaction between them, were significantly higher than the forces between other neutral polymers and mucins. Such polymers have been used to design ocular drug-delivery sxsystems for topical administration in order to increase the ocular residence time. Poly(lactic-co-glycolic acid) (PLGA) nanoparticles could be blended with a cationic polymer surfactant (Eudragit®RL), or coated with anionic Carbopol®to improve interactions with mucins. Carbopol®-coated, cyclosporine A (CsA)-encapsulated-PLGA nanoparticles with negative surface charge showed higher tear film CsA concentration after instillation on healthy rabbit eyes in comparison to non-coated PLGA nanoparticles. Positively charged Eudragit®RL-PLGA nanoparticles can further increase the tear film concentration (Cmax) and the area under the concentration-time curve between 0 and 24 h (AUC0-24 h) on healthy rabbit eyes, in connection to both Carbopol®-PLGA non-coated nanoparticles and nanoparticles and
Biography
Irach B. Taraporewala has over 30 years’ experiece in drug discovery/drug development R&D. He currently is President of the Sitara Pharmaceutical Consulting Group. He previously served as founder, CEO, President and Chief Technology Officer, and on the Board of Directors of OHR Pharmaceutical, Inc. an ophthalmology drug development company, and as a Drug Development consultant at PAREXEL Consulting. Dr. Taraporewala has published papers in drug development and delivery in reputed journals and has lectured extensively. He received a Ph.D. in Medicinal Chemistry from the Philadelpjhia College of Pharmacy and Science, and has been Principal Investigator on several NIH/DoD biomedical research grants.